The current coronavirus disease-2019 (COVID-19) pandemic caused 10,541 deaths among nursing home residents in France, by July 17th, 2020. This study reported the results of an urgent pre-hospital intervention in eight French nursing homes.
A retrospective study was conducted from March 26th to May 7th, 2020, before and after the intervention of a task force which took action from April 9th to April 11th, 2020. The task force included nurses and specialists of the county general hospital. The intervention had four steps: i) daily notification of deaths; ii) audit by infectious diseases and hygiene specialists focused on nursing team reinforcing, tracking of suspected cases, patients’ cohorting, review of preventive and protective measures, hydration, thromboembolism prevention; iii) intervention of an emergency team which urgently performed procedures suggested; iv) relay with a geriatric team.
There were a total of 770 residents distributed in eight facilities with capacity varying from 53 to 145 residents. The number of deaths peaked at 139 in week 2 and the trough at 0 occurred in weeks 6−7. Comparison between periods (before vs after intervention) showed a significant decrease in number of new deaths (83/770; 11% vs 35/687; 5%, p = 0.0001) and new COVID-19 cases (348/770; 45% vs 123/422; 29%, p < 0.001).
The urgent pre-hospital intervention by a multidisciplinary task force achieved mortality reduction during COVID-19 outbreak in nursing homes. Pre-hospital intervention is a valid alternative to hospitalization in case of hospital saturation.
The current coronavirus disease 2019 (COVID-19) pandemic caused 13,876,441 confirmed cases and 593,087 deaths worldwide by July18th, 2020; among them, 164,247 cases and 30,046 deaths were reported in France.1 Moreover, the median age at death was over 80 years and it highlighted that elderly people had the highest risk of death.2,3 In nursing homes, COVID-19 outbreak was dramatic and many countries reported elevated rates of contagion and deaths among residents. In this context, France reported 39,464 cases and 10,541 (27%) deaths among nursing home residents by July 17th, 2020.4
In France, the governmental epidemiology surveillance for COVID-19 in nursing homes monitors the epidemic from late March 2020 with the purpose of limiting the spread of severe acute respiratory syndrome coronavirus 2 (SARS-Cov2) infections in nursing homes. In this contest, the saturation of the county general hospital made it impossible to take care of nursing home residents affected by COVID-19. Thus, a new strategy was conceived to face COVID-19 outbreak in nursing homes. It was based on a task force which was activated whenever three or more deaths among suspected COVID-19 cases in a single nursing home were notified to the health regional agency (Agence Régionale de Santé or ARS). The task force included nurses and specialists of the county general hospital. It performed an audit to verify the standards of care at the nursing home and enforced preventive measures and patients’ treatments within the walls of the nursing home without referring patients to hospitals.
This study reports results of a survey conducted in eight nursing homes in France and the kind of measures enforced as well as their effectiveness in terms of new COVID-19 cases and deaths.
Materials and methodsA before-after study was conducted in eight nursing homes in the Ile de France region in France. COVID-19 epidemic was studied from March 26th, 2020 to May7th, 2020, before and after the intervention of a task force. All residents of the eight nursing homes were included in the study.
This study was conducted in accordance with Declaration of Helsinki and national and institutional standards. Approval by the local ethics committee was not required because a non-interventional research was conducted, meaning that all procedures and drugs administrated did not differ from daily clinical practice, according to the current French legislation. A written consent form was not proposed to patients because the non-interventional nature of the study required only the absence of patients’ opposition, according to the French law.5,6 No patient or legal representative expressed opposition for inclusion in this study, which has not received any support from private organizations.
The task force intervention was activated in the eight facilities from April 9th, 2020 to April 11th, 2020 and took a minimum of three days to two weeks (from week 3 to week 5), depending on the conditios of each facility. Indeed, the duration of the intervention varied according to the capacity of each facility to overcome difficulties, recruiting new health care personnel and buying new medical supplies. The task force consisted of nurses and specialists of the county general hospital (infectious diseases, hygiene and public prevention, emergency, and geriatrics specialists). The intervention of the task force included four steps: i) daily notification of deaths to the health authority by the facility; ii) in case of three or more deaths, audit by infectious diseases and hygiene and public prevention specialists to assess the standards of care of the facility, focusing on: presence of health care personnel (coordinator physician, nurses and nursing auxiliaries), medical supplies (oxygen supplementation machines, gloves, masks, gowns, hydro-alcoholic solution, conforming floor detergent), nursing reinforce (24 h presence of a nurse), tracking of suspected cases among the health care personnel, patients’ cohorting, review of preventive and protective measures, introduction of quarantine and isolation rooms (where appropriate), intravenous or subcutaneous hydration, thromboembolism prevention by low molecular weight heparin, administration of corticosteroids in patients with severe pneumonia and severe inflammatory syndrome (extremely high C-reactive protein and elevated leukocytosis) but with no suspicion of bacterial pneumonia,7,8 antibiotic administration in patient with suspected bacterial pneumonia; iii) intervention of an emergency team (physicians and nurses) which urgently performed medical and nursing procedures (non-invasive oxygenation, hydration, thromboembolism prevention, administration of corticoids or antibiotics) and patient follow-up in the very next days; iv) relay with a geriatric team which continued patients’ treatment and healthcare during the following days and weeks.
For the definition of COVID-19 cases, both probable and confirmed cases were included, according with international recommendations. Molecular tests were not performed systemically due to shortage of SARS-Cov2 PCR reagents in the entire French territory and prioritization for in-hospital diagnosis. Molecular tests were performed to confirm diagnosis in scarcely symptomatic patients, according to case-by-case medical decision.9,10
The following analyses were performed: i) description of characteristics of each facility according to task force audit; ii) description of the evolution of new COVID-19 cases and deaths; iii) comparison of new cases in each facility and in total population before and after the task force intervention; and iv) comparison of death rates in each facility and in total population before and after the task force intervention.
For statistical analysis, χ2-test was performed. Nominal statistical significance was set at p < 0.05.
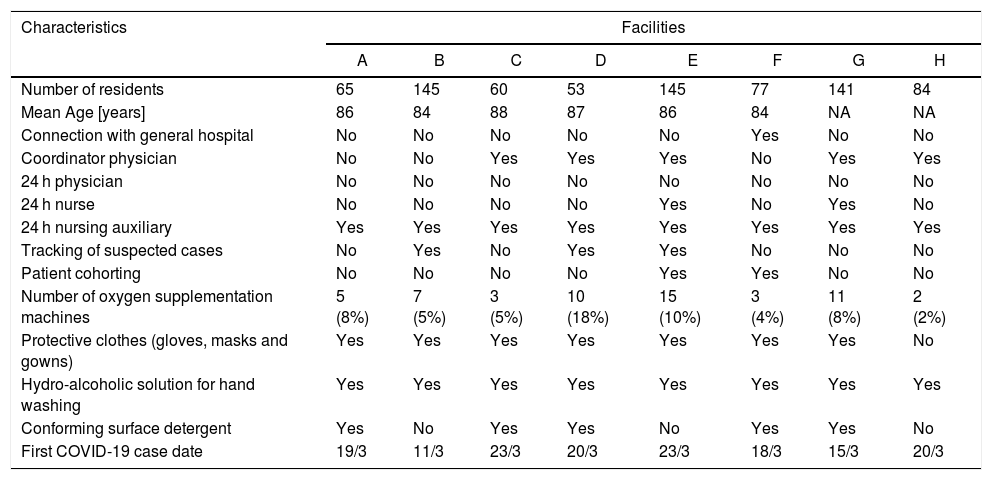
ResultsOverall, 770 residents were included in the study, distributed in eight facilities with capacity varying from 53 to 145 residents. Characteristics of the eight facilities were summarized in Table 1.
Characteristics of included facilities.
| Characteristics | Facilities | |||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | |
| Number of residents | 65 | 145 | 60 | 53 | 145 | 77 | 141 | 84 |
| Mean Age [years] | 86 | 84 | 88 | 87 | 86 | 84 | NA | NA |
| Connection with general hospital | No | No | No | No | No | Yes | No | No |
| Coordinator physician | No | No | Yes | Yes | Yes | No | Yes | Yes |
| 24 h physician | No | No | No | No | No | No | No | No |
| 24 h nurse | No | No | No | No | Yes | No | Yes | No |
| 24 h nursing auxiliary | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Tracking of suspected cases | No | Yes | No | Yes | Yes | No | No | No |
| Patient cohorting | No | No | No | No | Yes | Yes | No | No |
| Number of oxygen supplementation machines | 5 (8%) | 7 (5%) | 3 (5%) | 10 (18%) | 15 (10%) | 3 (4%) | 11 (8%) | 2 (2%) |
| Protective clothes (gloves, masks and gowns) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Hydro-alcoholic solution for hand washing | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Conforming surface detergent | Yes | No | Yes | Yes | No | Yes | Yes | No |
| First COVID-19 case date | 19/3 | 11/3 | 23/3 | 20/3 | 23/3 | 18/3 | 15/3 | 20/3 |
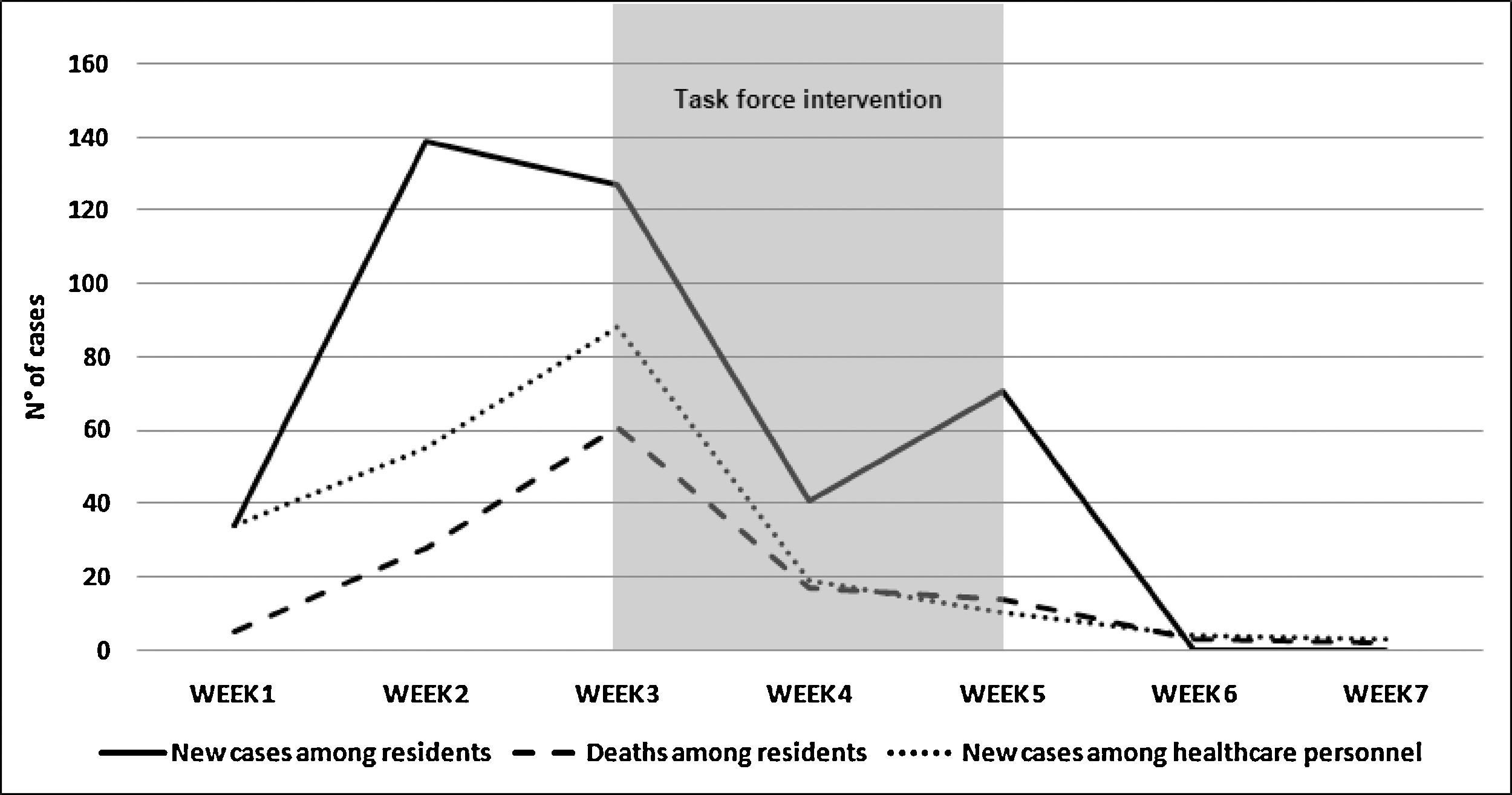
During the study period, the number of new deaths peaked at 139 in week 2 (from March 30th, 2020 to April 5th, 2020) and the trough of 0 occurred in week 6 and week 7 (from April 27th, 2020 to May 7th, 2020). The evolution of new cases had two peaks at the beginning of the study period in week 2 (from March 30th, 2020 to April 5th, 2020) at 139 new cases and in week 5 (from April 20th,2020 to April 26th, 2020) at 71 new cases. Task force intervention was implemented in the eight facilities at the end of week 3, from April 9th, 2020 to April 11th, 2020. Fig. 1 shows evolution of new COVID-19 cases and new deaths among residents of the facilities and healthcare personnel from March 26th, 2020 to May 7th, 2020.
Evolution of new COVID-19 cases and deaths from March 26th, 2020 to May 7th, 2020.
NOTE: task force intervention started in the eight facilities at the end of Week 3. Audit by infectious diseases and hygiene and public prevention specialists took place from April 9th, 2020 to April 11th, 2020. Interventions of emergency and geriatrics teams lasted from few days up to two weeks.
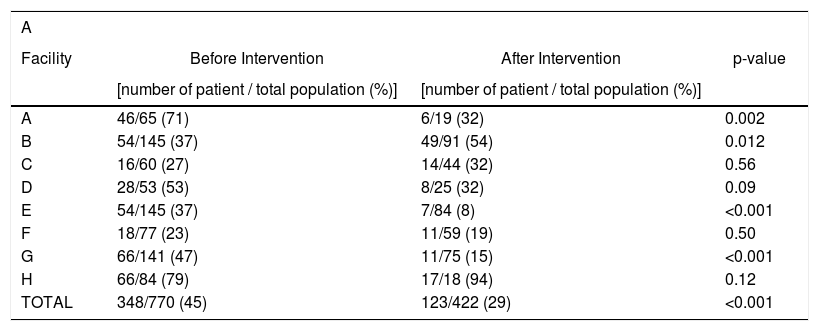
Comparison between periods (before vs after intervention) showed a significant decrease in the number of new cases in the overall population (348/770 (45%) vs 123/422 (29%), p < 0.001). A significant reduction in number of new deaths was observed in the facilities as a whole (94/770; 12% vs 36/676; 5%, p < 0.001). Table 2 shows the differences before and after the task force intervention in terms of new cases and deaths.
Before and after comparison of the task force intervention between facilities (A = new COVID-19 cases; B = deaths).
| A | |||
|---|---|---|---|
| Facility | Before Intervention | After Intervention | p-value |
| [number of patient / total population (%)] | [number of patient / total population (%)] | ||
| A | 46/65 (71) | 6/19 (32) | 0.002 |
| B | 54/145 (37) | 49/91 (54) | 0.012 |
| C | 16/60 (27) | 14/44 (32) | 0.56 |
| D | 28/53 (53) | 8/25 (32) | 0.09 |
| E | 54/145 (37) | 7/84 (8) | <0.001 |
| F | 18/77 (23) | 11/59 (19) | 0.50 |
| G | 66/141 (47) | 11/75 (15) | <0.001 |
| H | 66/84 (79) | 17/18 (94) | 0.12 |
| TOTAL | 348/770 (45) | 123/422 (29) | <0.001 |
| B | |||
|---|---|---|---|
| Facility | Before Intervention | After Intervention | p-value |
| [number of patient / total population (%)] | [number of patient / total population (%)] | ||
| A | 11/65 (17) | 2/54 (4) | 0.021 |
| B | 18/145 (12) | 11/127 (9) | 0.32 |
| C | 10/60 (17) | 2/50 (4) | 0.034 |
| D | 8/53 (15) | 0/45 (0) | 0.008 |
| E | 1/145 (12) | 5/127 (4) | 0.012 |
| F | 6/77 (8) | 6/71 (8) | 0.88 |
| G | 19/141 (13) | 10/122 (8) | 0.17 |
| H | 4/84 (5) | 0/80 (0) | 0.048 |
| TOTAL | 94/770 (12) | 36/676 (5) | <0.001 |
This study showed a mortality reduction among nursing home residents during a COVID-19 outbreak after urgent implementation of standards of care. Furthermore, it underlines the lack of human and material resources in some French nursing homes.
The main result of task force’s intervention was the significant mortality reduction. Although, a direct confrontation was not possible because of different settings, organization and population, our results are encouraging when compared to the severity of the COVID-19 epidemic among nursing homes in other countries.11 Moreover, our results are remarkable when compared with national data (5% vs 27% mortality).4 Finally, an indirect benefit of the implemented strategy was the reduction of residents’ hospitalization which contributed to reducing the pressure on the general hospital and, therefore, saving beds for general population.
Until now, the causes of death among COVID-19 patients have focused on co-morbidities and direct effects of SARS-CoV-2 infection, like pleurisy, pericarditis, lung consolidation, and pulmonary edema.12,13 However, in this study, mortality among nursing home residents reduced significantly after adoption of measures close to in-hospital standard of care, such as 24 h nurse presence, hydration and thromboembolism prevention. This is in line with results of other studies which demonstrated that nursing home quality has an impact on healthcare of COVID-19 patients and on morbidity and mortality.14,15 These results are encouraging and suggest that mortality among nursing home residents can be prevented by improving standards of care. Indeed, some deaths are not a direct consequence of SARS-CoV-2 infection but rather a consequence of the “confinement disease”, namely the physiopathological impairment developed because routinely clinical practices are not applied, such as hydration, thromboembolism prevention, and treatment of bacterial pneumonia.16,17 However, the current strategy based on task force activation after three or more deaths in a single nursing home needs to be revised. Indeed, earlier activation could have prevented many deaths, as suggested by the significant reduction of mortality after the task force intervention.
Notification to ARS and activation of the task force did not lead to an increase of new COVID-19 cases in the overall population analyzed, although the surveillance was higher after the task force intervention compared to before. On the contrary, new cases reduced before and after the task force intervention. However, it is impossible to tease out the role of preventing enforcement measures and the natural resolution of the epidemic, as well as the role of asymptomatic carriers.18
In this survey, each of the eight nursing homes presented some shortcomings in their organization. About human resources, the most evident limitation was the absence of a 24 -h nurse in 6/8 (75%) facilities which was exacerbated by the high number of sick leaves during the COVID-19 epidemics. Also, there was a coordinator physician in only 4/8 (50%) facilities. When material resources were analyzed, the most astonishing finding was the absence of a conforming surface detergent in 3/8 (38%) facilities. Moreover, the availability of oxygen supplementation for residents was very limited in many facilities such as in Facility D where it was sufficient for only 18%. These findings underscore the importance of reinforcing health care personnel and material supplies in many French nursing homes, to limit current and future disasters.19–21
The main limitation of this study was the late initiation of the observation period before the task force intervention in relation to the date of first COVID-19 cases reported by each facility. Thus, it is not possible to exclude that the results were boosted by the natural end of the outbreak which could have happened independently from the study intervention. Also, the study design did not allow to perform subgroup analyses to determine which measure was the most relevant in terms of decreasing mortality. Indeed, all measures were introduced as a package in each facility with the same criteria and patients received the same standard of care during the task force intervention. Further analyses are ongoing to describe the epidemic of SARS-CoV-2 infection in French nursing homes and the effectiveness of interventional measures enforced from the beginning of the epidemic.
ConclusionsIn conclusion, the urgent activation of a multidisciplinary task force reduced mortality during COVID-19 outbreak in nursing homes through reinforcement of standards of care. This result suggests that mortality of COVID-19 elderly patients is not only a direct consequence of SARS-CoV-2 infection but also a consequence of the “confinement disease”.
Preventing measures should be enforced earlier in the epidemic to achieve better control of COVID-19 outbreak. Considering the probable overlap between flu and COVID-19 epidemics in autumn/winter 2020/2021, we hope that extraordinary measures in nursing homes will have been taken by then, including a support of well-trained hospital nurses and specialists.
Funding statementThe article did not receive any financial support by private or public societies.
Declaration of interestNone.
Data availabilityThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Not applicable.