Many regions of the world where dengue epidemics are seasonal are also facing the COVID-19 pandemic. This is a medical concern because both diseases are difficult to distinguish since they have similar clinical symptoms and laboratory findings, and because they have different clinical management. So far, co-infection of SARS-CoV-2 and dengue virus (DENV) has not been studied. Herein we report the first case of a patient with co-infection of COVID-19 and dengue. Both infections were simultaneously laboratory confirmed by positive RT-qPCR for SARS-CoV-2 and RT-qPCR for DENV, NS1, IgM and IgG antibody tests for dengue. The patient had a favorable clinical improvement, without severe symptoms. This case emphasize that, in pandemic era, having a diagnostic of one infection does not rule out the possibility of having another infection concomitantly. In addition, underscores the importance of an accurate and timely diagnosis to prevent the spread of COVID-19.
SARS-CoV-2, the novel coronavirus that causes Coronavirus Disease 2019 (COVID-19), was firstly detected in Brazil on February 25, 2020. Since then, 202,918 cases had been confirmed as of May 14, 2020.1 In the same period, the country was also facing a dengue virus (DENV) epidemic. According to the Brazilian Ministry of Health, the incidence of dengue cases showed an upward trend, resulting in 676,928 cases until now.2 Brazil’s Federal District, located in the Central-West region of the country, has a high incidence of DENV in 2020 so far (841.9 cases/100,000 inhabitants)2 and SARS-CoV-2 is co-circulating leading to a unique and distinct health scenario for the population (Fig. 1). Co-infection of SARS-CoV-2 and DENV have not been studied neither described in detail until now. Here, we describe the first case where both viruses infected the same person simultaneously.
Number of dengue and COVID-19 cases per epidemiological week, in Federal District, Brazil, 2020.1,3.
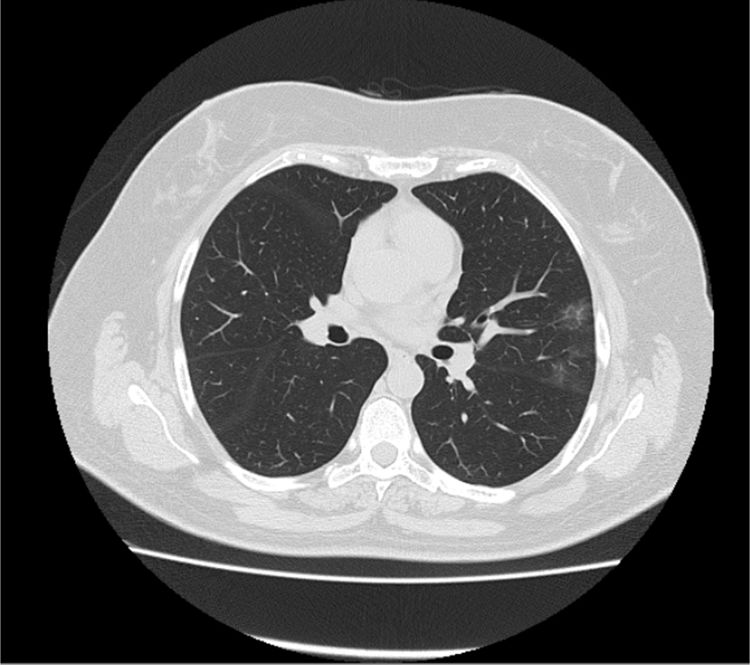
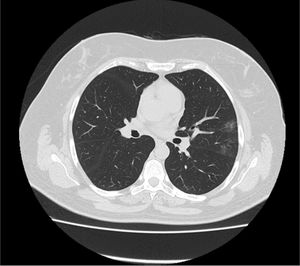
A previously healthy 56-year-old woman, with no travel history, resident in an urban area in Brasília city, Federal District, Brazil, was admitted to a local hospital on April 14, 2020. The patient complained of sore throat, anosmia and ageusia for the past 12 days, and frontal headache, fever, dry cough, mild dyspnea without need for supplementary oxygen and SpO₂ 94% on room air for five days. IgM and IgG antibody tests for DENV (SERION ELISA classic Dengue Virus IgM and IgG, Serion Inc., Brazil) were initially negative, whereas real-time reverse transcription – polymerase chain reaction (RT-qPCR) for SARS-CoV-2 (in-house laboratory developed test targeting N1 and E genes4 performed on a nasopharyngeal specimen) was positive. Blood samples showed leukopenia (2260/mm³), lymphopenia (497/mm³), thrombocytopenia (143,000/mm³), and elevated D-dimer (3986 ng/mL), C-Reactive Protein-CRP (16 mg/L), serum alanine aminotransferase (ALT 60 U/L), aspartate aminotransferase (AST 40 U/L), and ferritin (559 ng/mL). Chest computed tomography (CT) images demonstrated few bilateral, peripheral ground glass opacities (Fig. 2). The patient started therapy with chloroquine, azithromycin and anticoagulation.
Three days after hospitalization, the patient developed a diffuse itchy erythemato-papular rash, mainly located in the limbs and trunk regions (Fig. 3), gastrointestinal symptoms such as diarrhea and nausea, worsening of leukopenia (1820/mm³), new onset of atypical lymphocytes (9%), thrombocytopenia (92.000/mm³) and progressive elevation of aminotransferases (ALT 546 U/L, AST 433 U/L). A new laboratory investigation for dengue and COVID-19 was performed turning out positive for NS1 (SD BioLine Dengue NS1 Ag from Alere Inv., USA), DENV RT-qPCR (in-house laboratory developed test targeting UTR sequence common to all four dengue virus genotype5), and IgM and IgG antibody tests for dengue. SARS-CoV-2 RT-qPCR was again positive. Furthermore, dengue virus was confirmed as serotype DENV-1 (CDC DENV 1–4 genotyping protocol6). All medications were discontinued and the patient had progressive clinical improvement, without complications, and was discharged on day 6 of hospitalization. Once at home, she stayed isolated until two consecutive negative tests for SARS-CoV-2 at day 26 of onset of symptoms.
DiscussionThis was the first case report of a human co-infection of SARS-CoV-2 and DENV, in which both viruses were detected by RT-qPCR at the same time. We believe that the patient was first infected by SARS-CoV-2, presenting a mild disease, and one week later, during the illness of COVID-19, she was infected by DENV. Despite the co-infection, the patient did not have severe respiratory disease nor severe dengue. Recently, two patients diagnosed with COVID-19 by SARS-CoV-2 RT-PCR had positive serological antibody tests for dengue but negative DENV RT-PCR were described in Singapore, suggesting false-positive serological test results for dengue or cross-reaction.7
Dengue and COVID-19 could be difficult to distinguish because they have similar clinical symptoms and laboratory findings, such as fever, headache, myalgia and fatigue, making differential diagnosis challenging.8,9 Although infrequent, COVID-19 cases can present skin rash10 and low platelet count, meaning that one disease can be initially misdiagnosed as the other. Moreover, a positive dengue serology may appear on a false-positive test, also in co-infection with SARV-CoV-2 and DENV. The incorrect or delayed diagnosis can have serious consequences, because each disease has different clinical management, such as venous hydration, use of anticoagulants, corticosteroids, and early mechanical ventilation.11
ConclusionThis report confirm that, in pandemic era, diagnosing one infection does not rule out the possibility of having another infection concomitantly. In addition, it underscores the importance of an accurate and timely diagnosis, with a complete laboratory investigation for both dengue and COVID-19, in territories where there is a possibility of dengue infection, since each infection has different clinical management. Beyond that, we alert for this public health concern, especially highlighting the need in obtaining the correct contact and droplet precautions in health services and communities, helping reducing human-to-human transmission, prevent outbreaks and delay the spread of COVID-19 pandemic.
Conflicts of interestThe authors declare no conflicts of interest.
We thank Clara Wandenkolck Silva Aragão for the language help, Ticiane Henriques Santa Rita and Pedro Góes Mesquita for the laboratory contributions.