Ciguatera poisoning is the most common form of non-bacterial food-poisoning from fish worldwide. The incidence among Brazilians returning from high-risk regions is unclear because it is not a mandatory reportable disease. We describe a previously healthy 53-year-old Brazilian woman developed Ciguatera fish poisoning while traveling to Havana, Cuba. Physicians and health care professionals should advise travelers to avoid eating ciguatoxic fish species and potentially toxic fish species in the Caribbean islands. Despite the prognosis for most cases is good with a short duration of self-limited symptoms, early recognition of the identifying clinical features of ciguatera can result in improved patient care.
Ciguatera fish poisoning is a food-borne illness caused by the consumption of reef fish containing ciguatoxins.1,2 Although most ciguatera cases are seen in endemic tropical areas, there is an increasing potential for cases to be encountered in temperate regions. In this report, we describe a healthy 53-year-old Brazilian patient that acquired ciguatera poisoning following travel to Havana, Cuba, for one week on business. She stayed in a hotel and ate foods prepared in restaurants. Three nights before her departure to Brazil, she ate a portion of a fish identified by the host as red snapper. Approximately 10 h after her meal, she went to the emergency room complaining of severe headache accompanied by pain in the back and joints, particularly her knees, abdominal discomfort associated with nausea and vomiting. She also described paresthesia of mouth and extremities, extremity pruritus and cold allodynia. The diagnosis of ciguatera poisoning was made on the basis of the epidemiological data and the association of gastrointestinal and neurological symptoms. Management was supportive including oral hydratation, antiemetics and antihistamines, and non-steroidal anti-inflammatory drugs.
After returning to Brazil, her symptoms persisted, with noted weakness depressed mood despite avoiding heavy exercise, alcohol and caffeine consumption. By three months after onset, the symptoms had resolved entirely, and the patient returned to her normal life without diet restrictions.
Ciguatera is a food-borne illness that occurs in inhabitants, and visitors of islands surrounded by coral reefs. Surface microalgae attached to biodetritus and macroalgae on coral reefs are associated with the causative toxins.3 Certain strains of Gambierdicus toxicus and Ostreopsis lenticularis produce toxins that are modified in the stomach of fish. Ciguatoxins are predominately concentrated in the Caribbean. It has been estimated that less than 20% of ciguatera illnesses are reported, with the extent of underreporting likely to vary between countries. Tourist arrivals to Caribbean destinations reached 29.9 million tourist visits in 2018. Table 1 describes the case reports of patients with ciguatera poisoning acquired in the Caribbean.4–13 The incidence among Brazilians returning from high-risk regions is unclear because it is not a mandatory reportable illness. There has been a previous report of ciguatera poisoning in Brazilians travelers.8 Although the mortality rates from ciguatera poisoning are low, the morbidity is high. Gastrointestinal manifestations start 6–12 h after consumption of contaminated fish. Neurological and sometimes psychiatric symptoms appear 24–72 h later, with weakness of the limbs, perioral paresthesia, and sensation of hot/cold temperature reversal (paradoxical dysesthesia or cold allodynia). Myalgia, arthralgia, headache, ataxia, and dizziness can also be observed. Other manifestations include asthenia, pruritus, cutaneous rash, eye and dental pain, and dysuria. In severe cases, cardiovascular disorders (hypotension, bradycardia) can occur. There is currently no standard laboratory test to confirm ciguatera poisoning, however, there are assays that can qualitatively measure ciguatoxin in the fish fluid.1 Management includes avoidance of potential exacerbating triggers.2 Report of heavy exercises, consumption of caffeine, peanuts, seafood, and alcohol have all been associated with worsening of symptoms. Although there are no consistent studies, intravenous mannitol therapy had been proposed as the treatment of choice. The effect of mannitol is thought to be mediated by the reduction of neuronal edema through the modulation of sodium ion concentrations across cell membranes. Gabapentin and amitriptyline were used to treat pain, and paresthesias and fluoxetine for neuropsychiatric conditions such as anxiety and chronic fatigue. To prevent mass ciguatera fish poisoning, physicians and health care professionals should advise travellers to avoid eating ciguatoxic fish species and potentially toxic fish species in the Caribbean islands including large reef fish and ocean predators such as barracuda, grouper, and snapper.3
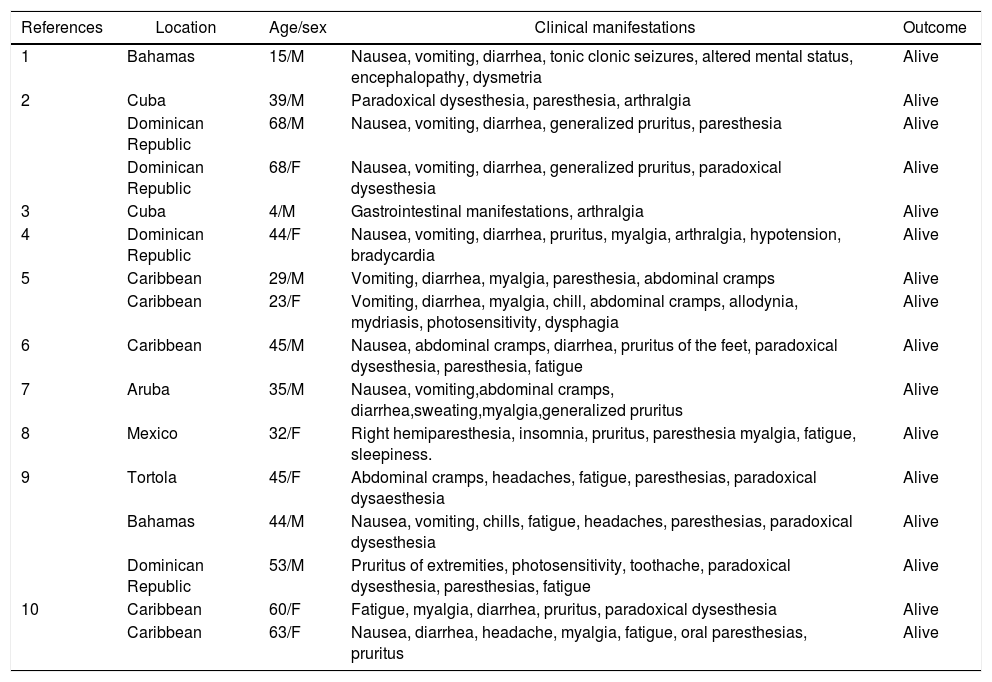
Case reports of ciguatera poisoning acquired in the Caribbean.
| References | Location | Age/sex | Clinical manifestations | Outcome |
|---|---|---|---|---|
| 1 | Bahamas | 15/M | Nausea, vomiting, diarrhea, tonic clonic seizures, altered mental status, encephalopathy, dysmetria | Alive |
| 2 | Cuba | 39/M | Paradoxical dysesthesia, paresthesia, arthralgia | Alive |
| Dominican Republic | 68/M | Nausea, vomiting, diarrhea, generalized pruritus, paresthesia | Alive | |
| Dominican Republic | 68/F | Nausea, vomiting, diarrhea, generalized pruritus, paradoxical dysesthesia | Alive | |
| 3 | Cuba | 4/M | Gastrointestinal manifestations, arthralgia | Alive |
| 4 | Dominican Republic | 44/F | Nausea, vomiting, diarrhea, pruritus, myalgia, arthralgia, hypotension, bradycardia | Alive |
| 5 | Caribbean | 29/M | Vomiting, diarrhea, myalgia, paresthesia, abdominal cramps | Alive |
| Caribbean | 23/F | Vomiting, diarrhea, myalgia, chill, abdominal cramps, allodynia, mydriasis, photosensitivity, dysphagia | Alive | |
| 6 | Caribbean | 45/M | Nausea, abdominal cramps, diarrhea, pruritus of the feet, paradoxical dysesthesia, paresthesia, fatigue | Alive |
| 7 | Aruba | 35/M | Nausea, vomiting,abdominal cramps, diarrhea,sweating,myalgia,generalized pruritus | Alive |
| 8 | Mexico | 32/F | Right hemiparesthesia, insomnia, pruritus, paresthesia myalgia, fatigue, sleepiness. | Alive |
| 9 | Tortola | 45/F | Abdominal cramps, headaches, fatigue, paresthesias, paradoxical dysaesthesia | Alive |
| Bahamas | 44/M | Nausea, vomiting, chills, fatigue, headaches, paresthesias, paradoxical dysesthesia | Alive | |
| Dominican Republic | 53/M | Pruritus of extremities, photosensitivity, toothache, paradoxical dysesthesia, paresthesias, fatigue | Alive | |
| 10 | Caribbean | 60/F | Fatigue, myalgia, diarrhea, pruritus, paradoxical dysesthesia | Alive |
| Caribbean | 63/F | Nausea, diarrhea, headache, myalgia, fatigue, oral paresthesias, pruritus | Alive |