Tuberculosis infection is a serious human health threat and the early 21st century has seen a remarkable increase in global tuberculosis activity. The pathogen responsible for tuberculosis is Mycobacterium tuberculosis, which adopts diverse strategies in order to survive in a variety of host lesions. These survival mechanisms make the pathogen resistant to currently available drugs, a major contributing factor in the failure to control the spread of tuberculosis. Multiple drugs are available for clinical use and several potential compounds are being screened, synthesized, or evaluated in preclinical or clinical studies. Lasting and effective achievements in the development of anti-tuberculosis drugs will depend largely on the proper understanding of the complex interactions between the pathogen and its human host. Ample evidence exists to explain the characteristics of tuberculosis. In this study, we highlighted the challenges for the development of novel drugs with potent bacteriostatic or bactericidal activity, which reduce the minimum time required to cure tuberculosis infection.
The pathogen responsible for tuberculosis (TB) infection, Mycobacterium tuberculosis, was first identified by Robert Koch in 1882. However, the global TB epidemic remains undiminished and is expected to reach 9,8 million new cases in 2010, more cases than in any previous year in history. About 80% of these new TB cases will be found in the 20–25 highest-burden countries, with more than one-third in India and China. A review of the TB cases reported by 134 countries between 1998 and 2007 found that only 35 had per capita rates of decline exceeding 5% per year.1 However, surveillance and mathematical modeling suggests that the total TB incidence per capita is falling at an estimated 1% per year, a finding that indicates that the global incidence rate will decrease by 2015. However, the world's population is growing at about 2% per year, and thus the total number of new TB cases remains on the rise.2 This finding reveals the relative failure of the existing management strategies for TB and the inadequate effectiveness of public health systems, mainly in underdeveloped countries. In spite of the availability of anti-TB drugs developed over the last five decades, one-third of the world's population retains a dormant or latent form of M. tuberculosis. These populations are generally asymptomatic but remain at lifelong risk of disease reactivation and represent a high risk factor for the spread of the disease (Fig. 1).
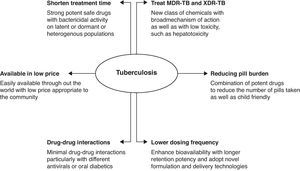
Currently, the TB epidemic is further exacerbated by the existence of multidrug resistant-TB (MDR-TB) and extremely drug resistant-TB (XDR-TB) strains and declining treatment options as least three effective drugs are required to be used in combination in order to successfully treat the disease while preventing the development of further drug resistance.3 The last drug therapy discovered and approved, which employs a new mechanism of action for treatment of TB, was combination dosing using isoniazid (INH) and rifampicin (RIF). However, MDR-TB is resistant to INH and RIF. Cases of MDR-TB and XDR-TB result from either primary infection with a drug-resistant bacteria strain or non-optimal treatment durations or regimens. In spite of the introduction throughout the world many years ago of concomitant chemicals for use in TB treatment, lower cure rates for MDR-TB have been observed, ranging from 50 to 70%.4 XDR-TB is resistant to INH and RIF, all fluoroquinolones, and at least one of the second-line anti-TB injectable drugs including amikacin, kanamycin and/or capreomycin. These types of resistance TB infections produce very high mortality rates.3 Furthermore, the occurrence of drug–drug interactions excludes the co-administration of some existing TB drugs with other medications used in chronic diseases.5 Multiple effective therapies need to be developed that produce multiple functions such as shortening of treatment time, efficacy against MDR-TB and XDR-TB strains, simpler treatment regimens including lower dosing frequencies, and therapies that can be co-administered with medications used in other chronic diseases. The challenge of meeting the spectrum of expectations for this desired target product profile complicates drug discovery efforts as many of the forthcoming compounds are either derivatives of presently used compounds or modulate the same cellular processes as drugs currently in use.5,6 In addition, the analogues and derivatives in development are far from translation into the clinic, may be subject to cross-resistance, and may be hampered by the unfavorable economics surrounding TB drug development and lack of proper policy incentives.
The aim of this study was to determine whether or not there are a sufficient number of promising compounds in the TB pipeline necessary in order to achieve global control of this epidemic. We presented a mechanism of action against TB infection, provided a perspective with the goal of improving the focus of discovery and development efforts, and identified the underlying knowledge gaps and scientific obstacles in TB drug development.
Drug resistance mechanisms in Mycobacterium tuberculosisThe existing situation surrounding the growing drug-resistant TB patient population is significantly disquieting and represents a significant weakness in the ability to control disease on a global scale.5,6 Any viral infection causing human immune system deficiency can reactivate the TB infection5 and generate the potential of producing new TB cases. In recent reports, the percentage of MDR cases demonstrating resistance to various classes of antibiotics ranged from 0 to 22.3%.6 Around 40.000 cases of XDR-TB are projected to emerge worldwide each year.5,7 It is of utmost importance to figure out the mechanisms through which the mycobacterial cells resist anti-tuberculosis drugs. Understanding the mechanism will enable the design of new anti-tuberculosis drugs as well as methods for interfering with the expression of such drug resistance.7
The resistance to TB drugs appeared very soon after the introduction of the first drug, streptomycin. Chromosomal mutations occurring at a frequency of 10−6 to 10−8 mycobacterial replications enable the development of genetic resistance to an antibacterial drug.5 The advantage of using a multidrug regimen lies in the fact that the chromosomal loci responsible for resistance to various drugs are not linked. Thus, the possibility of developing resistance to three drugs administered simultaneously becomes 10−18 to 10−20, an outcome whose probability is extremely low or almost negligible.8 Enormous efforts have been made to identify the molecular basis of drug action and resistance in the TB pathogen. The drug action and the bacterial resistance mechanism of a few commonly used drugs have been briefly summarized to highlight the need for novel drug design that could reduce treatment time and avoid the occurrence of drug resistance in the treatment of TB infections.
Resistance to anti-TB drugsIsoniazid (INH)Since its introduction as an anti-TB drug in 1951, INH has been the most widely used treatment for TB and its latent infections.9,10 INH penetrates into the cell as a pro-drug activated by katG, the gene encoding catalase-peroxidase. The peroxidase activity of this enzyme is essential in activating INH and enabling its interactions with various toxic reactive species in the bacterial cell.11 The reactive species usually consist of oxides, hydroxyl radicals, and organic moieties that deteriorate components of the cell wall which results in the loss of cellular integrity, and finally, bacterial death.12 The resistance frequency of 105,6 for INH is much higher than that for most anti-tuberculosis drugs.13 InhA enzyme (enoyl-acyl carrier protein reductase), involved in the elongation of fatty acids in mycolic acid synthesis, is considered the primary target of INH inhibition.14 The replacement of an amino acid in the NADH binding site of Inh A apparently results in INH resistance, preventing the inhibition of mycolic acid biosynthesis. Various genetic mutations have been observed to occur usually between codons 138 and 328; the Ser315Thr mutation is most frequent and found in about 40% of all INH-resistant strains.15–17 The mutation at Ser315Thr results in an enzyme lacking the ability to activate INH, but preserves approximately 50% of its catalase-peroxidase activity.18 Thus, the modified catalase-peroxidase offers high-level resistance to INH while maintaining a high level of oxidative protection sufficient to facilitate the organism in sustaining its detoxifying activity against host antibacterial free radicals.
Rifampicin (RIF)Rifampin, rifapentine, and rifabutin have been commonly used as first-line therapies in combination with other drugs for the treatment of TB infections. The use of RIF in combination with PZA/INH led to the establishment of short therapy courses, which reduced routine TB treatment from 1 year to 6 months. RIF is believed to inhibit bacterial DNA-dependent RNA polymerase. RNA polymerase is composed of four different subunits (α, β, β′, and σ), and the genetic loci coding for these subunits include the rpoA, rpoB, rpoC, and rpoD genes, respectively. RMP interferes with RNA synthesis by binding to the β subunit of the RNA polymerase, hindering transcription and thereby killing the organism. Resistance to RIF arises due to missense mutations in the gene. In M. tuberculosis, resistance to RIF occurs at a frequency of 10−7 to 10−8,5 The resistance in RIF develops due to mutations in a distinct, 81-base-pair (bp) (27-codon) central region of the gene that encodes the β-subunit of RNA polymerase.19 About 96% of all mutations are found in the 81-bp core region of the gene between codons 507 and 533, with the most common changes occurring in codons Ser531Leu, His526Tyr, and Asp516Val.20
Pyrazinamide (PZA)PZA is a vital first-line drug for the treatment of tuberculosis. PZA has an excellent sterilizing effect on semidormant tubercle bacilli. By killing semidormant bacilli in an acidic environment, PZA, along with INH and RIF, forms the cornerstone of modern TB treatment therapy. PZA has played an important role in reducing the duration of TB treatment from the previous 9–12 months to the current 6 months.21 PZA is a prodrug that is converted to its active form pyrazinoic acid (POA) by the mycobacterial enzyme pyrazinamidase/nicotinamidase. PZA, produced intracellularly, diffuses into the tuberculosis pathogen in a passive manner, and is converted into POA by pyrazinamidase within the cell. The inefficient efflux system of the mycobacterial cell enables massive accumulation of POA in the bacterial cytoplasm, leading to disruption of the membrane potential.22,23 The exact mechanism of PZA resistance remains unknown. However, it is known that PZA-resistant bacterial strains usually lose their pyrazinamidase activity.24 Cloning and sequencing studies of the gene that encodes pyrazinamidase revealed that 72–97% of all PZA-resistant clinically isolated specimens carry a mutation either in the structural gene or in the putative promoter region of the gene.25
Ethambutol (EMB)EMB is a first-line drug that is used in combination with INH, RIF, and PZA in order to prevent the emergence of drug resistance specific to mycobacterium. EMB is an active bacteriostatic agent for bacilli that are growing but has no effect on non-replicating bacilli. EMB interferes with the mycobacterial cell wall through a synthetic mechanism and inhibits arabinosyl-transferase, which is involved in cell wall biosynthesis.26 Encoded by arabinosyl-transferase and involved in the synthesis of arabinogalactan, arabinosyl-transferase has been proposed as the target of EMB action within the tuberculosis organism.27 Studies have shown that resistance to EMB is due to random spontaneous genetic mutations occurring at a rate of approximately 1 in 107 organisms; mutations most commonly result in increased production of the enzyme arabinosyl-transferase, which overwhelms the inhibitory effects of EMB. Studies have identified five mutations in codon 306 including ATG-GTG, ATG-CTG, ATG-ATA, ATG-ATC, and ATG-ATT that result in three different amino acid substitutions (Val, Leu, and Ile) in EMB-resistant strains.28,29 These five mutations are associated with 70–90% of all EMB resistant isolates.29
Current challenges in the TB treatmentThe current anti-TB drugs, discovered primarily in the 1950s to 1970s, were developed through a series of clinical trials that extended into the 1980s.30 The subsequent 30 years, until approximately 2000, represented a fallow period in TB drug research and development, a void contributing greatly to the significant challenges currently faced by the community of drug developers focused on markedly improving treatments for active MDR-TB and XDR-TB. At present, MDR-TB is treated using a combination of different drugs with therapies lasting 18–24 months, with only four of these drugs developed for the purpose of treating TB.31 Suboptimal therapy leads to almost 30% of MDR-TB patients experiencing treatment failure.32 The treatment options for XDR-TB are very limited because XDR-TB bacilli are resistant, not only to INH and RIF, but also to fluoroquinolones including injectable drugs such as aminoglycosides. In addition, there are serious side effects observed with most MDR-TB and XDR-TB drugs, including nephrotoxicity and ototoxicity with the use of aminoglycosides, hepatotoxicity with the use of ethionamide, and dysglycemia with the use of gatifloxacin.33
The vast majority of TB cases and deaths occur in poor countries and about one in four of the deaths occur among HIV-positive people. It has been reported that 9,4 million patients diagnosed with TB in 2009 (11–13%) were also HIV positive with approximately 80% of these morbidities confined to the African region.34 This is due to limited health care access as well as diminished compliance with therapeutic regimens associated with increased pill burden, drug–drug interactions, and overlapping toxic side effects. The primary interaction between HIV and anti-TB treatment agents is RIF-induced overexpression of the hepatic cytochrome (CYP P450) oxidase system.35 Studies have shown that CYP increased the pharmacokinetic rate and decreased the efficacy of several concomitant medications including HIV protease inhibitors.36 It is noted that with the use of CYP450 inhibitors, such as ritonavir, normal trench levels of various classes of protease inhibitors cannot be regained. Accordingly, they have been shown to compete with rifampicin in intracellular phosphorylation. Thus, these drugs should not be co-administered. However, the presence of ritonavir in a protease cocktail increases the serum concentration of rifabutin, thereby increasing its accompanying toxicity.37 Multiple drug interaction studies are few for most second-line TB drugs such as ethionamide, cycloserine, kanamycin, amikacin, capreomycin and para-amino salicylate, which have been in use since the last decade for treating HIV patients with MDR- or XDR-TB strain co-infections.38 Therefore, specific active case-finding strategies are needed to target HIV-infected individuals as well as the interaction of anti-retrovirals with currently available second-line TB drugs, as well as those currently in clinical development.
Like HIV, diabetes is also associated with the suppression of cell-mediated immunity and is known to increase the risk of developing active TB by three-fold.39 Studies in 2000 revealed that approximately 20% of smear-positive TB cases were attributed to concurrent diabetes in India.40 In the meantime, if the projected rise from 25 million diabetes cases in 2000 to 80 million in 2030 comes to fruition, and the risk ratio remains the same, then 42% of smear-positive TB cases in India will be attributable to diabetes by 2030. Each TB case caused by diabetes would also potentially lead to the infection of other people, adding to the overall TB burden in the community.41 The biological basis for the limited response of diabetics to anti-TB agents and for their increased risk of developing MDR-TB is poorly understood. But, it is believed that cell-mediated immunity is suppressed in diabetes and fosters higher TB infection rates.
Future clinical TB drugs to overcome drug resistanceDevelopment of drugs for the treatment of TB and other epidemic diseases has been lacking for decades. The conventional approach to TB drug development requires substituting each approved drug in the current multi-drug regimen, but only after the new drug has been approved for treatment as a single agent. TB control initiative program for the testing of new compounds simultaneously could drastically shorten the development timeline, but ethical implications should be considered in the identification of a practical way to implement such clinical trial designs.5,6
Adenosine triphosphate (ATP) synthase inhibitorsThe selection of new TB drug targets has been determined mainly by accessibility to the genome sequence of the TB pathogen. But studies dealing with the invention of new drugs have shown that genome-derived and target-based approaches generally have modest therapeutic effects in the area of antibacterials.42 Studies have also shown that changing the selection approach from single-enzyme targets to the whole bacterial cell level greatly improves the effects of TB drugs. However, the whole-cell screening approach is hindered by a lack of understanding of the mechanism of action as well as identification of the relevant ligands for internal infections.43 Current achievements utilizing the whole-cell approach are highlighted by the identification of new TB drug agents such as TMC207, a diarylquinoline that inhibits ATP synthesis, and BTZ043, a benzothiazine that blocks arabinan synthesis.44,45 TMC207 (R207910 or the ‘J’ compound) is active against drug-sensitive and drug-resistant M. tuberculosis isolates.46,47 Along with bactericidal characteristic against dormant (non-replicating) tubercle bacilli, it also has the potential to minimize the treatment duration.48 TMC207 has shown same inhibitory effects in murine model of tuberculosis likely shown by isoniazid, rifampin, and pyrazinamide in a combination. However, a significant increase in the rate of bacilli clearance was reported by using TMC207 along with triple-drug regimen and the synergistic interaction with pyrazinamide.49 Moreover, it has been reported that TMC207 in case of murine model of drug-sensitive enhances the effectiveness of second-line drug combination.50 TMC207 has also been evaluated in phase II dose ranging trial conducted for 7 days in patients with drug-susceptible tuberculosis. The results reveal that only at the highest dose (400mg) clinically relevant bactericidal activity was achieved with a delay in onset of response. This treatment was associated with acceptable adverse-events.51 Additionally, controlled trial having consisting of an (8 weeks) followed by a separate proof-of-efficacy stage (24 weeks), was conducted to evaluate TMC207 efficacy in patients with newly diagnosed, smear-positive pulmonary infection caused by multidrug-resistant M. tuberculosis. TMC207 reduced the time interval to conversion to a negative sputum culture.51 These examples demonstrate that multi-dimensional signaling pathway inhibition can be used as the basis for the identification of new TB treatment scaffolds.
Protein synthesis inhibitorsRemodeling of present regimens is also a viable strategy for fueling momentum in the antibiotic development pipeline and discovering new treatment scaffolds for use against resistant bacterial strains. Different members of each antibiotic class share a common core structure, and upon synthetic modification, the core of the antibiotic is left intact but its functional groups are rearranged to potentiate the drug's activity.
The tailored forms of oxazolidinones (linezolid against Gram-positive infections) have provided a platform for new structures such as PNU-100480 and AZD-5847, which have been found to enhance antibiotic activity.44 For the very first time, 4-amino-1,2-oxazolidin-3-one (cycloserine), a new class of antibacterial agent, was used. Cycloserine is a broad-spectrum antibiotic that has been used as a second-line antituberculosis drug since 1955.52,53 In the modern era when several bacterial strains are becoming resistant against antibiotics, linezolid (Zyvox) is the only agent approved by Food and Drug Administration (FDA) in the class and released in 2000 by Upjohn for the treatment of nosocomial pneumonia and skin and soft tissue infections caused by Gram-positive bacteria.52 Against MDR-TB, linezolid was the first oxazolidinone that has been used off-label, However, its long-term use has not been prescribed because of certain side effects associated with its continuous use, such as thrombocytopenia, anemia, and peripheral and optic neuropathy.54 For M. tuberculosis, minimum inhibitory concentration (MIC) is in the range of 0,125–1,0μg/mL; because of its severe side effects it was replaced by PNU-100480 (Sutezolid), an analogue of linezolid developed by Pizer with similar MICs for M. tuberculosis, for better in vivo activity and less toxicity.52,55,56 In a comparison study of the murine model of TB, PNU-100480 has shown more potent bactericidal activity compared with linezolid, even at lower drug exposures.44 Additionally, the introduction of PNU-100480 enhanced the bactericidal activities of regimens containing some first-line drugs to certain folds, giving a clue that it may be effective at minimizing the treatment duration for drug-susceptible TB by 1–2 months.57 An earlier study investigated its safety, tolerability, pharmacokinetics, and pharmacodynamics in humans by giving different doses, i.e., 100, 300, or 600mg twice daily or 1200mg once daily for 14 days, or 600mg twice daily for 28 days, to which PZA was added on days 27 and 28. A sixth cohort was given linezolid at 300mg daily for 4 days. None of the doses given showed any lethal effect and were well tolerated.58Cmax level was 0,94 or 2,01μg/mL, and half-life was 2,92 or 3,38h, respectively, in healthy volunteers receiving twice-daily 600mg or once-daily 1200mg of PNU. Trough concentrations were maintained at or above the MIC. An EBA analysis suggests daily testing of 600mg and 1200mg for 14 days. AZD-5847 (posizolid) is a lead-containing compound that is used to cure TB by AstraZeneca. It possesses an MIC analogous to that of linezolid and PNU-100480 for curing M. tuberculosis, and has shown profound effect in mouse model experiment of TB.53 At 600mg oral dosing, Cmax is 2,60μg/mL in fasting subjects and 5,66μg/mL in fed subjects, with a half-life close to 8h but it has caused nausea in the test organism.53 A daily oral dose of 800, 1600 and 2400mg for 14 days in healthy volunteers was well tolerated, and has caused an increased Cmax up to 10μg/mL; however, the increase was not in proportion to the dose.53 Similarly, cephalosporins such as cefaclor and ceftazidime are more impervious to destruction by the resistance enzyme β-lactamase, and enter the bacterial membrane more efficiently. Furthermore, new β-lactamases can cleave third-generation cephalosporins. Thus, fourth-generation molecules such as cefepime were developed that are less susceptible to cleavage by β-lactamase.45 Cephalosporins and other semi-synthetic antibiotics harbor 64% of the new chemical scaffolds that were filed between 1981 and 2005.59
Nitromidazole (PA-824), Delaminid (OPC 67683)PA-824 is a prodrug derived from metronidazole that has shown strong activity against anaerobic bacteria and protozoa (trichomoniasis, amoebiasis). PA-824 has demonstrated significant sterilizing and anti-tuberculosis activity, with an MIC90 of 0,125μg/mL against both drug-resistant and non-drug-resistant strains of M. tuberculosis.60 It is bactericidal against actively replicating and latent (non-replicating or slowly replicating) TB bacteria. Its bactericidal mechanism against replicating aerobic species involves the inhibition of synthesis of certain proteins and cell wall lipid components required for the survival and replication of bacterial species. The latent bacteria are killed by releasing nitric oxide gas during enzymatic nitro-reduction that poisons the respiratory machinery.61 In murine models of TB, PA-824 demonstrated bactericidal activity not only during initial phase but also in the continuation phase where it killed the bacteria that had survived for initial two months.62 The individual administration of PA-824 has shown bactericidal activities comparable to that of moxifloxacin and isoniazid.63 The evaluation of PA-824 in combined therapies with first-line drugs to shorten the treatment time produced encouraging results. Its daily intake in combination with moxifloxacin and PZA has contributed to an impressive sterilizing regimen, signifying the potential to shorten the treatment time.64 A study compiled by substituting isoniazid with PA-824 remarkably lower lungs CFU after 2 months treatment as well as led to a rapid culture-negative conversion when compared first-line combination of rifampin, INH and PZA.65 Its substitution with rifampin in first-line drug during intensive phase therapy is suggested to drastically reduce the treatment of multidrug-resistant tuberculosis.66 Different amounts of oral doses of PA-824 were given to TB patients in comparison to the control (standard first-line TB treatments). The results confirmed promising bactericidal activities of PA-824, signifying that soon it will be included in regimen for quick and effective treatment of drug-susceptible and drug-resistant TB.67
DNA gyrase inhibitorsFluoroquinolones are a group of antimicrobials that kill M. tuberculosis via double-stranded breaks in DNA, by binding to DNA gyrase. DNA gyrase consists of two A and two B subunits encoded by the gyrase A (gyrA) and gyrase B (gyrB) genes, respectively.68 Previously drugs such as ofloxacin and levofloxacin were in use rather than the nalidixic acid derivatives moxifloxacin and gatifloxacin, which are being developed currently for DS-TB. The gatifloxacin by the Oflotub Consortium (NCT00216385) and moxifloxacin by Bayer and the TB Alliance (NCT00864383) have been evaluated in Phase III trial, substituted with the first-line regimen for ethambutol (gatifloxacin, moxifloxacin) and isoniazid (moxifloxacin) to shorten treatment of DS-TB.69 Several studies have shown the potential of moxifloxacin and gatifloxacin in vitro and in mouse models of TB70,71 as well as in humans.72,69 Additionally, the potential toxicities of these drugs are mostly group related, but among them, gatifloxacin has been reported to disturb glucose metabolic state in diabetic and aged individuals.73 In contrast, this type of drawback was not associated with moxifloxacin treatment.74 Studies have also shown the reduced drug–drug interaction of gatifloxacin and moxifloxacin because these drugs are not strong inhibitors or inducers of the CYP enzyme system and also not metabolized to a great extent.75 RIF is first line TB drug, which reduced approximately 30% plasma concentrations of moxifloxacin but according to the pharmacokinetic and dynamic condition of moxifloxacin, RIF induce glucuronidation or sulphation which reduced moxifloxacin plasma level in 18 out of 19 patients.76,77 We hope that the Phase III trials will elaborate the safety and efficacy of a 4-month, fluoroquinolone-based treatment for drug susceptible-TB, which could be translated to the clinic for the treatment of TB by 2015.
ConclusionIn this report we provided examples of persistent TB transmission and of enhanced susceptibility of large populations to infection and disease. It is clear that all currently approved TB drugs are facing a certain level of resistance governed by specific genetic mutations in the disease-causing Mycobacterium. Long-term use of a specific drug results in the loss of its efficiency with increasing levels of bacterial resistance. Therefore, the right drug should be taken at the right time in order to avoid development of severe bacterial resistance problems. This study also highlighted some promising bactericidal agents for quick prevention and effective treatment of drug-susceptible and drug-resistant TB.
Another suggestion by WHO is to change the drug dosing at regular intervals within a prescribed format.78 Besides these approaches, it is important to develop novel drugs that avoid the manifestation of drug resistance in bacterial cells. We conclude that control programs have been less effective than expected in reducing the occurrence of TB transmission, mainly because patients are not diagnosed and cured quickly enough. We do hope that enhancing features of antibiotics will help in developing improved tools for TB control. These TB control efforts will need to be reinforced and redoubled if TB is to be eliminated as a global public health crisis. The priority now should be to maintain the basic principles of treatment using chemotherapy such as gatifloxacin and moxifloxacin but implement these efforts with greater vigor.
Conflict of interestAll authors declare to have no conflict of interest.