Sexual behavior is a key factor for susceptibility to sexually transmitted diseases. An evaluation of the sexual behavior of women at reproductive age was conducted in 1999. A replication of this study aims to evaluate the current situation and identify changes in sexual behavior, 13 years later. This is a population-based cross-sectional study, conducted with 1071 women in Pelotas, Brazil. Compared to the 1999 study, a 14% increase in early sexual debut and an 8% decrease in the non-use of condoms were observed in 2012. The proportion of women who reported anal sex doubled between these periods. There was no trend of increase or decrease in the prevalence of behaviors with distinct patterns being observed for each of them. Reduction of non-use of condoms may be an indicator of the effectiveness of campaigns to promote safe sex. However, the increased prevalence of early sexual debut and anal sex indicates the need for campaigns to continue and to expand their focus, especially among vulnerable groups.
Sexually transmitted diseases (STDs) constitute an important public health problem worldwide and are a major cause of acute illness, infertility, disability and death.1 From the economic point of view, they are among the top ten reasons for seeking health care and are responsible for 17% of economic losses caused by health problems in developing countries.2 In Brazil, in 2010, the Unified Health System (SUS) spent R$ 784 million just on the acquisition and distribution of drugs for the treatment of STDs.3
According to the World Health Organization (WHO), in 2008 there were about 499 million new cases of STDs among men and women aged 15–49 years, all over the world, due to Treponema pallidum (syphilis), Neisseria gonorrhoeae, Chlamydia trachomatis and Trichomonas vaginalis.1 Moreover, millions of other viral STD cases occur each year, mainly due to infection by human immunodeficiency virus (HIV), herpes virus, papillomavirus and hepatitis B.2 Regarding HIV, it was estimated that in 2012 there were 2.3 (1.9–2.7) million new cases of infections and 35.3 (32.2–38.8) million people living with the virus.4 In Brazil, the incidence rate of acquired immunodeficiency syndrome (AIDS) in 2012 was 20.2 cases per 100,000 inhabitants, which has remained stable over the last five years, and the prevalence of HIV was estimated at 0.6% among persons who were 15–49-year-old.5 Despite a 33% decline in the incidence rate in 2012 compared to 2001, the number of people living with HIV increased due to greater survival as a result of improved access to antiretroviral therapy.4
The relationship between sexual practices and STD acquisition is well established in the literature. Several studies have shown an association between STDs and risk behaviors, such as alcohol and drug use, multiple sexual partners, early sexual initiation, anal sex, and sex practice without condoms.6–9 Women, due to biological and social issues as unequal power relations between genders, are especially vulnerable to STDs.10–12 In recent years in Brazil, there has been a decrease in the gender ratio of HIV/AIDS cases over the years, from 26:1 men:women in 19805 to 1.4:1 in 2005. Since then this ratio has shown a slight increase to 1.7:1 in 2012.5
An evaluation of the sexual behavior of women at reproductive age was conducted in 1999.13,14 A replication of this study aims to evaluate the current situation and identify changes in the sexual behavior of women aged 13 years or more.
Materials and methodsThis is a temporal comparative evaluation of two population-based cross-sectional studies, conducted in 1999 and 2012. To ensure comparability, the study methodology used in 2012 was kept identical to that of 1999. As the methodological aspects of the 1999 study are available in other publications,13,14 we will describe in detail in this article only the methodology of the 2012 study.
Data collection was conducted between January and June 2012 in Pelotas, a city in southern Brazil, whose population is approximately 328,000 inhabitants.15 The target population were women aged 15–49 years living in the urban area of Pelotas, who had at some time or the other sexual intercourse. Institutionalized women or those with a disability that prevented them from providing the required information were excluded. A multistage and proportional-to-size sampling was performed. The primary sampling unit was the census tracts defined by the Brazilian Institute of Geography and Statistics (IBGE) in the 2010 census and the secondary sampling unit was the household. After a systematic selection 130 census tracts were included. We performed a systematic selection of the households according with the size of each tract, with 111 to 36 households being selected per tract, with a total of 1722 households included.
The selected households were visited by a trained interviewer who had at least a high school education. Because the questions dealt with intimate issues, information about sexual practices was obtained through a confidential self-applied questionnaire, which was handed out to the women by the interviewer. After completing the questionnaire, the respondent inserted it in an envelope, which was sealed with tape and placed in a sealed ballot box, thus ensuring confidentiality of the information. Data from this questionnaire were double-entered in the EpiData program.
Sexual risk behaviors for STD/HIV were assessed using the following questions: “At what age did you first have sex?” (early onset was considered to be at 17 years or less), “The last time you had sex, did your partner use a condom?” (yes, no), “The last time you had sex, did you use alcohol and/or any drug before?” (no, alcohol only, drugs only, both), “The last time you had sex, did you practice anal sex (from behind)?” (yes, no), “In the last three months with how many people have you had sex?”(multiple sexual partners were considered to be two or more), and “The last time you had sex, did your partner use alcohol and/or any drug?” (no, alcohol only, drugs only, both). Intercourse was considered to be any vaginal, anal or oral intercourse. Information on alcohol or drugs at the last sexual intercourse was analyzed as a dichotomous (yes, no) variable, due to the small proportion of women who reported drug use or both, either of their own or of their partner.
In addition, perception of vulnerability was assessed through the following question: “In your assessment, what is the chance of you getting AIDS or any other disease through sex?” (very possible, possible, quite possible, almost impossible, impossible). Independent variables were assessed through the following information: age (years), skin color observed by the interviewer (white, non-white), marital status (married/living with a partner, unmarried, divorced/separated, widowed), income per capita (in minimum wages), education (years of schooling), smoking (yes, no), and alcohol consumption in the past 30 days (yes, no). Information on perceptions of vulnerability and the independent variables was obtained through face-to-face interviews. All questions were pretested through a pilot study, conducted in a census tract not selected during the sampling process.
In order to verify concordance among answers and possible inconsistencies, as well as the field work, a quality control was conducted, through random selection of 10% of the sample. Those women selected received a visit from a field supervisor 15 days or less after the interview to reapply the questions about perception of vulnerability. Kappa concordance test was performed.
A descriptive analysis of the sample characteristics of both studies was carried out. Chi-square test was used to assess whether there were statistically significant changes in some characteristics of the sample. After that, Poisson regression was used to calculate the crude and adjusted prevalence for each risky sexual behavior. Adjustment was performed for sociodemographic and behavioral characteristics that were statistically different between the two surveys (marital status, income, education, and smoking). A significance level of 5% and a two-tailed p-value were used. Due to complex sampling, the analyses were carried out considering the sample design effect. All analyses were performed using Stata 12.0 (StataCorp, College Station, TX, USA).
This study was approved by the Ethics Committee of the Federal University of Pelotas on December 1, 2011 (protocol 77/11). All study participants signed the terms of informed consent.
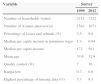
ResultsA total of 1543 eligible women were identified in 1999 and 1071 in 2012. The refusal rate was higher in 2012 (8.8%). Although the per capita income (in reais) had increased in 2012, the median income in minimum wage decreased. The mean age in both studies was approximately 33 years old, and the variable with the largest proportion of missing values was number of partners in the 2012 (9.1%) study. Comparison of characteristics of the two samples is presented in Table 1.
Comparison of descriptive characteristics of both surveys on sexual risk behaviors among women 15–49 years, in Pelotas, Southern Brazil.
| Variable | Survey | |
|---|---|---|
| 1999 | 2012 | |
| Number of households visited | 2112 | 1722 |
| Number of women interviewed | 1543 | 1071 |
| Percentage of losses and refusals (%) | 3.5 | 8.8 |
| Median per capita income in minimum wage | 1.3 | 0.94 |
| Median per capita income | 172 | 583 |
| Mean age | 33.6 | 32.9 |
| Quality control (%) | 7 | 10 |
| Kappa test | 0.7 | 0.6 |
| Highest percentage of missing data (%) | 5.3 | 9.1 |
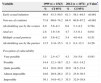
Socioeconomic, demographic and behavioral characteristics of the 1999 and 2012 samples are presented in Table 2. The age structure of the samples did not change significantly (p=0.6986). Close to 80% in both surveys were white (p=0.1549). In both periods, the majority of women were married or living with a partner, but in 2012 there was an increase in the proportion of single women and a decrease in those married/living with a partner, widowed and separated/divorced (p=0.0009). The proportion of women with a per capita income above one minimum wage decreased significantly in 2012, while the proportion of women with an income of at most one minimum wage increased (p=0.0061). A significant reduction in the proportion of women with less than nine years of schooling was observed (p<0.001). In the 2012 study, there was a significant decrease in the prevalence of smokers (p<0.001). The prevalence of alcohol use in the past 30 days also decreased, but this reduction was not statistically significant (p=0.1128).
Distribution of demographic, socioeconomic and behavioral characteristics of women aged 15–49 years, according to survey, in Southern Brazil.
| Variable | 1999 (n=1543)a | 2012 (n=1071)a | p-Value* | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age (y) | |||||
| 15–19 | 150 | 9.7 | 114 | 10.6 | 0.6986 |
| 20–24 | 240 | 15.5 | 163 | 15.2 | |
| 25–29 | 214 | 13.9 | 152 | 14.2 | |
| 30–34 | 212 | 13.8 | 161 | 15.0 | |
| 35–39 | 238 | 15.4 | 139 | 13.0 | |
| 40–44 | 240 | 15.6 | 172 | 16.1 | |
| 45–49 | 249 | 16.2 | 170 | 15.9 | |
| Skin color | |||||
| White | 1216 | 78.8 | 885 | 82.6 | 0.1549 |
| Other | 327 | 21.2 | 186 | 17.4 | |
| Marital status | |||||
| Married/consensual union | 937 | 60.7 | 601 | 56.1 | 0.0009 |
| Single | 422 | 27.4 | 381 | 35.6 | |
| Widowed | 150 | 2.2 | 75 | 1.3 | |
| Separated/divorced | 34 | 9.7 | 14 | 7.0 | |
| Per capita income (minimum wage) | |||||
| 0–0.5 | 280 | 18.5 | 244 | 23.5 | 0.0061 |
| 0.51–1.00 | 348 | 23.1 | 321 | 30.9 | |
| 1.01–2.00 | 395 | 26.2 | 254 | 24.5 | |
| >2.0 | 487 | 32.3 | 219 | 21.1 | |
| Schooling (y) | |||||
| 0–4 | 279 | 18.2 | 92 | 8.6 | <0.001 |
| 5–8 | 573 | 37.2 | 264 | 24.7 | |
| 9–11 | 406 | 26.4 | 370 | 34.6 | |
| >11 | 279 | 18.2 | 345 | 32.2 | |
| Smoking | |||||
| Yes | 1082 | 70.1 | 853 | 79.6 | <0.001 |
| No | 461 | 29.9 | 218 | 20.4 | |
| Alcohol use in the last 30 days | |||||
| No | 723 | 51.9 | 543 | 56.7 | 0.1128 |
| Yes | 668 | 48.1 | 414 | 43.3 | |
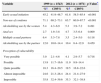
The crude prevalence of sexual risk behaviors for women aged 15–49 and their confidence intervals are presented in Table 3. Use of alcohol and/or drugs by women and by partners, as well as having had multiple sexual partners did not change significantly. The average age of first sexual intercourse dropped from 18.3 years (95% CI 18.1–18.5) in 1999 to 17.1 years (95% CI 16.9–17.2) in 2012 (data not shown on table). We observed an increase in prevalence of early sexual initiation from 47% in 1999 to 61% in 2012. The prevalence of non-use of condoms during the last sexual intercourse decreased significantly, from 72% in 1999 to 64% in 2012, and the prevalence of anal sex at the last intercourse increased from about 3% to 5% in the period. The perception of vulnerability did not differ significantly between the surveys. In both, over 60% of respondents claimed to believe it was impossible or almost impossible to get AIDS or any other STD.
Crude prevalence of sexual risk behaviors, among women aged 15–49 years, in Southern Brazil, according to survey.
| Variable | 1999 (n=1543) | 2012 (n=1071) | p-Value* | ||
|---|---|---|---|---|---|
| % | CI 95% | % | CI 95% | ||
| Early sexual initiation | 46.9 | 43.3–50.5 | 61.3 | 58.1–64.5 | <0.001 |
| Non-use of condoms | 71.9 | 69.6–74.2 | 64.0 | 60.8–67.2 | <0.001 |
| Alcohol/drug use by the women | 6.9 | 5.6–8.3 | 6.6 | 5.1–8.2 | 0.784 |
| Anal sex | 2.8 | 1.9–3.6 | 4.7 | 3.3–6.1 | 0.011 |
| Multiple sexual partners | 6.9 | 5.6–8.2 | 5.4 | 4.0–6.8 | 0.151 |
| Alcohol/drug use by the partner | 13.5 | 11.6–15.3 | 11.3 | 9.3–13.3 | 0.126 |
| Perception of vulnerability | |||||
| Very possible | 3.5 | 2.4–4.7 | 4.3 | 3.0–5.6 | 0.543 |
| Possible | 14.4 | 12.1–16.7 | 12.1 | 10.1–14.2 | |
| Quite possible | 18.4 | 16.0–20.9 | 20.9 | 18.5–23.4 | |
| Almost impossible | 24.6 | 20.9–28.2 | 27.2 | 23.9–30.5 | |
| Impossible | 39.1 | 34.8–43.3 | 35.5 | 32.0–38.8 | |
In the adjusted analysis, there was neither change in the magnitude of the prevalence of analyzed variables nor in the significance of the differences between surveys. The adjusted prevalence of behaviors is presented in Table 4.
Adjusted prevalence of sexual risk behaviors, among women aged 15–49 years, in Southern Brazil, according to survey.
| Variable | 1999 (n=1543) | 2012 (n=1071) | p-Value* | ||
|---|---|---|---|---|---|
| %a | CI95% | %a | CI95% | ||
| Early sexual initiation | 45.2 | 41.9–48.7 | 61.8 | 58.5–65.4 | <0.001 |
| Non-use of condoms | 71.1 | 69.2–73.1 | 63.7 | 60.0–67.7 | <0.001 |
| Alcohol/drug use by the women | 5.4 | 4.3–6.9 | 5.3 | 3.9–7.2 | 0.491 |
| Anal sex | 2.7 | 1.9–3.8 | 4.7 | 3.5–6.4 | 0.009 |
| Multiple sexual partners | 6.4 | 5.3–7.8 | 3.5 | 2.4–5.0 | 0.118 |
| Alcohol/drug use by the partner | 12.0 | 10.0–14.4 | 10.4 | 8.4–12.9 | 0.459 |
| Perception of vulnerability | |||||
| Very possible | 3.0 | 2.1–4.6 | 4.1 | 2.9–5.7 | 0.718 |
| Possible | 13.9 | 11.7–16.6 | 11.9 | 9.9–14.4 | |
| Quite possible | 18.3 | 16.4–20.5 | 19.5 | 16.8–22.6 | |
| Almost impossible | 24.6 | 21.3–28.4 | 24.4 | 21.4–27.9 | |
| Impossible | 35.8 | 32.4–39.6 | 35.3 | 32.1–38.8 | |
This study compared the prevalence of sexual risk behaviors among women of reproductive age, 13 years after the base study.13,14 There was not a consistent increase or decrease in the behaviors evaluated, with distinct patterns being verified for different behaviors, which will be discussed separately below.
Early sexual initiation is worrying because it increases the time of exposure to STDs, especially among young people, who may not be prepared to deal with the risks presented by sex. Furthermore, early sexual initiation is associated with greater number of lifetime sexual partners, which is also associated with the acquisition of STD.8,9 A case–control study conducted among women aged 15–49 years in southern Brazil, aiming to identify factors associated with HIV infection, showed that sexual initiation before the age of 15 was significantly more common among HIV-infected women (44%) than among uninfected controls (8%).16 The results of this study showed a decrease of about one year in the average age of first intercourse and an increase of approximately 14% points in the proportion of women who had early sexual initiation (≤17 years). In Brazil, results of the National Survey on Demography and Health of Children and Women (PNDS), conducted with women aged 15–49 across the country, showed similar results, with a decline in the average age of sexual debut from 18.6 years in 1996 to 17.9 years in 2006.17 However, in a global perspective, although many studies suggest a decrease in age at first sexual intercourse, this is not a global trend and regional differences should be considered.18
Anal sex is associated with the acquisition of STD,19 and is the sexual practice that offers the highest risk of infection by HIV.7 A study published by Barbosa and Koyama,20 with data from the study “Sexual Behavior and Perceptions of the Brazilian Population regarding HIV/AIDS” carried out in 1998 and 2005, investigated, among other behaviors, the practice of anal sex with the last sexual partner in the last 12 months before interview, in the Brazilian population aged between 16 and 65 years. The results showed, among women, an increase from 14.2% in 1998 to 16.1% in 2005, although this was not statistically significant.20 In the present study, although low, the proportion of women who reported anal sex significantly increased between the two periods.
The consumption of substances such as alcohol and drugs before sex is associated with STD6,21,22 and also other risky behaviors such as unprotected sex, greater number of sexual partners, and early sexual initiation.23,24 The use of alcohol and/or drugs before their last intercourse, either by the woman or by their partner, had a slight, but not significant, decrease in the period.
Regarding the occurrence of multiple sexual partners, Barbosa and Koyama20 found that both in 1998 and in 2005, the proportion of women who said to have had more than one sexual partner in the 12 months preceding the survey was approximately 5%, compatible with the result found in the current study, which found a non-significant decrease (from 6.9% to 5.4%) in the proportion of women who reported more than one partner in the three months preceding the survey. A study conducted by Herlitz and Steel25 with 11,000 Swedish individuals monitored for 10 years (1987–1997) for changes in sexual behavior and attitudes toward HIV in the country, also found similar results. The number of sexual partners, evaluated in the 12 months preceding the survey, remained constant, at about 7%.
The use of condoms during sexual intercourse is the most important form of protection against STD. The results presented in this study showed a reduction of about 8% points in the practice of unprotected sex. Another study using data from the study “Sexual Behavior and Perceptions of the Brazilian Population regarding HIV/AIDS” conducted by Berquó et al.26 investigated the use of condoms.26 The study showed, among women with a stable partner, an increase between the two periods from 19.9% to 34.2% in condom use in the last 12 months. Among women with casual partners, in both surveys, this percentage was 66%. Condom use at last intercourse, assessed only in 2005, was 23%. Data from the PNDS showed that the percentage of women between 15 and 24 years who reported condom use at first intercourse increased from 18% in 1996 to 63% in 2006. Herlitz and Steel25 found that condom use in at least one relationship, in the month before the interview, increased from 21% in 1987 to 23% in 1997.
Regarding the perception of vulnerability, about two-thirds of the sample in both surveys believed it was impossible or almost impossible to get an STD, with no significant difference between the periods.
Despite the differences in the magnitude of estimates due to various recall periods and cutoff points used to evaluate behaviors, the results of this study are similar to those of other national population based studies in terms of tendency of behaviors prevalence. Although being conducted in a specific region of Brazil, the consistency of the results improves the external validity of the present study and suggests that changes shown in these period may also have occurred in a national level and could be as a consequence of wide social changes and not only regional characteristics.
It is important to consider that the social, demographic and behavioral characteristics of the population, such as education, income, marital status and smoking, known to be associated with the occurrence of sexual risk behaviors, have changed significantly between 1999 and 2012. However, when the analyses performed were adjusted for these factors, there was no change in the significance and magnitude of the associations observed in the crude analyses and statistically significant differences remained in the prevalence of early sexual debut, condom use, and anal sex. This confirmed that the changes observed in this study are not a consequence of changes in the socioeconomic and demographic structure of the population, but of behavioral and cultural factors in women.
It is also necessary to consider the limitations of this study. The reported experiences of intimate experiences are subject to bias and there may be a tendency for respondents to provide socially acceptable answers. This problem was minimized by applying a confidential questionnaire to obtain information about sexual practices. Because information on vulnerability perception was collected through face-to-face interviews, it could have been subject to this bias. However, we believe that this possibility does not affect the purpose of the study since it touches both surveys equally. The Kappa coefficient for the question about perceived vulnerability was considered moderate. It is possible that after being questioned during the interview about their own risk of acquiring STD, the respondent has reflected on her condition, which may have altered their perception, so that in the quality control interview a different answer was provided. The highest percentage of missed responses was regarding the age at first sex in both surveys, which suggests a fair comparison.
Despite the limitations, it is important to note that this study was designed and conducted with the methodological rigor necessary to ensure comparability between surveys. The low percentage of non-respondents and the sampling process (population-based) ensured representativeness of the sample, making selection bias unlikely.
We conclude that the adoption of risky sexual behavior is common among women. Although some risk behaviors have remained unchanged between the two periods, early sexual initiation increased considerably and anal sex nearly doubled. Nonetheless, sexual intercourse without condom use decreased.
The decrease in non-condom use could be an indicator of the effectiveness of educational campaigns promoting safe sex through the use of this method, carried out in recent years. Considering that condom use is the main way to avoid STD and that it is a method with easy access, with free distribution on the network of primary health care of the Brazilian health system, the necessity and importance of primary prevention through continuing and strengthening educational campaigns and promoting sexual health, especially among young people is evident.
However, it is necessary that policies promoting sexual and reproductive health of women also focus on other aspects of sexual risk behaviors, such as sexual initiation in early ages, anal sex, and use of alcohol and drugs, neglected by current prevention policies.
Conflicts of interestThe authors declare no conflicts of interest.
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (grant no. 337/2010) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (grant no. 133847/2011-0).