Recent studies have shown that some drugs that are not routinely used to treat fungal infections have antifungal activity, such as protease inhibitor antiretroviral drugs. This study investigated the in vitro susceptibility of Histoplasma capsulatum var. capsulatum to saquinavir and ritonavir, and its combination with the antifungal itraconazole. The susceptibility assay was performed according to Clinical and Laboratory Standards Institute guidelines. All strains were inhibited by the protease inhibitor antiretroviral drugs. Saquinavir showed minimum inhibitory concentrations ranging from 0.125 to 1μgmL−1 for both phases, and ritonavir presented minimum inhibitory concentrations ranging from 0.0312 to 4μgmL−1and from 0.0625 to 1μgmL−1 for filamentous and yeast phase, respectively. Concerning the antifungal itraconazole, the minimum inhibitory concentration values ranged from 0.0019 to 0.125μgmL−1 and from 0.0039 to 0.0312μgmL−1 for the filamentous and yeast phase, respectively. The combination of saquinavir or ritonavir with itraconazole was synergistic against H. capsulatum, with a significant reduction in the minimum inhibitory concentrations of both drugs against the strains (p<0.05). These data show an important in vitro synergy between protease inhibitors and itraconazole against the fungus H. capsulatum.
Histoplasmosis is a systemic infection caused by the dimorphic fungus Histoplasma capsulatum. It is mainly associated with immunosuppression, especially in HIV patients.1,2 This disease is characterized by a broad spectrum of clinical manifestations ranging from asymptomatic to disseminated forms.3 Histoplasmosisis is widely distributed in the Americas.4 In Brazil, the number of cases has increased in several regions. Some outbreaks have been recorded in the country, involving the states of Rio de Janeiro, São Paulo, Minas Gerais, Espírito Santo, Mato Grosso, and Rio Grande do Sul.4–6 In Ceará state, a recent study reported 254 cases of histoplasmosis in patients with HIV in the period from 2006 to 2010, showing its high prevalence in this region.7
Treatment of histoplasmosis depends on the severity of infection, clinical manifestations and individual risk factors. The therapy indicated for mild to moderate cases is the administration of azoles, such as itraconazole. The use of amphotericin B is limited to severe cases because of its high toxicity. Due to the increase of histoplasmosis cases in recent years, particularly among HIV patients, associated with the occurrence of refractory and recurrent infections, there is a need to find new therapeutic approaches to control this mycosis.8,9 Some studies have shown that certain drugs not routinely used to treat fungal infections have significant antifungal activity.10 Among these, the antiretroviral drugs have demonstrated the ability to interfere with the viability and virulence of fungal cells. The protease inhibitors indinavir and ritonavir have shown in vitro and in vivo inhibitory effects against Candida albicans.11 Indinavir also has shown activity against the fungus Cryptococcus neoformans, reducing its virulence and making it more susceptible to the killing activity of natural effector cells of the immune system.12
Thus, this study aimed to evaluate the in vitro susceptibility of H. capsulatum var. capsulatum to the antiretroviral drugs saquinavir and ritonavir, as well as their combination with the azole antifungal itraconazole.
Materials and methodsMicroorganismsWe used a total of 20 clinical strains of H. capsulatum in the filamentous phase and 10 in the yeast phase, isolated from the Northeast and Southeast regions of Brazil. The samples came from the culture collection of the Specialized Medical Mycology Center, Federal University of Ceará, and were handled in a biosafety level 3 cabin.
Antifungal agentsStock solutions of the antiretroviral drugs saquinavir (Roche Holding AG, Basel, Switzerland) and ritonavir (Abbott Laboratories, Chicago, USA) and the antifungal itraconazole (Janssen Pharmaceutica, Beerse, Belgium) were prepared in dimethyl sulfoxide (DMSO). These solutions were stored at −20°C until use. Serial dilutions of each antimicrobial agent were prepared in RPMI 1640 (Sigma Chemical Corporation, St. Louis, MO, USA), supplemented with l-glutamine, buffered at a pH of 7.0 with MOPS 165mmoll−1 (Sigma Chemical Corporation, St. Louis, MO, USA).
Preparation of fungal inoculumTo prepare the inoculum, fungal suspensions were prepared in saline from stock cultures after seven days of incubation, maintained on BHI (brain heart infusion) agar and incubated at 28°C for the filamentous phase. The cultures were maintained on BHI agar supplemented with sheep blood at 10% and incubated at 35°C to obtain the yeast phase. The inoculum was adjusted to 90–95% by transmittance spectrophotometry at a wavelength of 530nm. After reading, the suspensions were diluted 1:10 in RPMI 1640 medium to obtain inoculums of approximately 0.5×103 to 2.5×104cfumL−1.13
Susceptibility testThe in vitro antifungal activity was determined by the broth microdilution method in accordance with the protocol described in document M27-A3 and standardized by the Clinical Laboratory Standards Institute.14 Initially, the minimum inhibitory concentration (MIC) was determined for each drug. Subsequently, the MIC values were used as the highest concentration to prepare drugs in combination. The concentration ranges of the drugs alone were: 0.0039–2μgmL−1 for saquinavir, 0.0156–8μgmL−1 for ritonavir, and 0.0009–0.5μgmL−1 for itraconazole. The concentration ranges of the drugs in combination were: 0.0002–1μgmL−1 for saquinavir, 0.00006–4μgmL−1 for ritonavir and 0.000003–0.0625μgmL−1 for itraconazole. The results were determined by visual readings after seven and four days of incubation at 35°C for strains in the filamentous and yeast phase, respectively. The MICs were defined as the lowest concentration of drug able to inhibit 80% of the fungal growth for antiretroviral drugs and itraconazole, as well as for the combination of both.13 Drug interaction was evaluated by calculating the fractional inhibitory concentration index (FICI), which was classified as synergistic (FICI≤0.5), indifferent (0.5<FICI<4), or antagonistic (FICI≥4).15 The FICI values obtained for each drug combination against H. capsulatum were compared through Wilcoxon test (p<0.05). The analysis was carried out using IBM SPSS ver. 21.0 software (IBM Co., Armonk, NY, USA). Standard strains of Candida parapsilosis ATCC 22019 and Candida krusei ATCC 6258 were included in each test as quality controls.
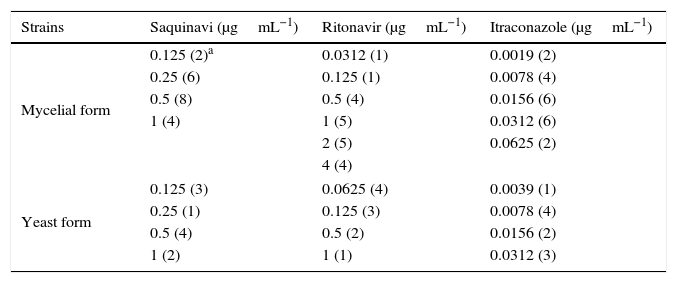
ResultsThe protease inhibitors saquinavir and ritonavir were capable of inhibiting the strains of H. capsulatum, with MIC values ranging from 0.125 to 1μgmL−1 for saquinavir in both filamentous and yeast phase; and from 0.0312 to 4μgmL−1 and from 0.0625 to 1μgmL−1 for ritonavir in filamentous and yeast phase, respectively (Table 1). Concerning itraconazole, the MIC ranged from 0.0019 to 0.0625μgmL−1 and from 0.0039 to 0.0312μgmL−1 for the filamentous and yeast phase, respectively (Table 1).
MICs of antiretroviral drugs and itraconazole against strains of Histoplasma capsulatum var. capsulatum in yeast-like and mycelial forms.
| Strains | Saquinavi (μgmL−1) | Ritonavir (μgmL−1) | Itraconazole (μgmL−1) |
|---|---|---|---|
| Mycelial form | 0.125 (2)a | 0.0312 (1) | 0.0019 (2) |
| 0.25 (6) | 0.125 (1) | 0.0078 (4) | |
| 0.5 (8) | 0.5 (4) | 0.0156 (6) | |
| 1 (4) | 1 (5) | 0.0312 (6) | |
| 2 (5) | 0.0625 (2) | ||
| 4 (4) | |||
| Yeast form | 0.125 (3) | 0.0625 (4) | 0.0039 (1) |
| 0.25 (1) | 0.125 (3) | 0.0078 (4) | |
| 0.5 (4) | 0.5 (2) | 0.0156 (2) | |
| 1 (2) | 1 (1) | 0.0312 (3) | |
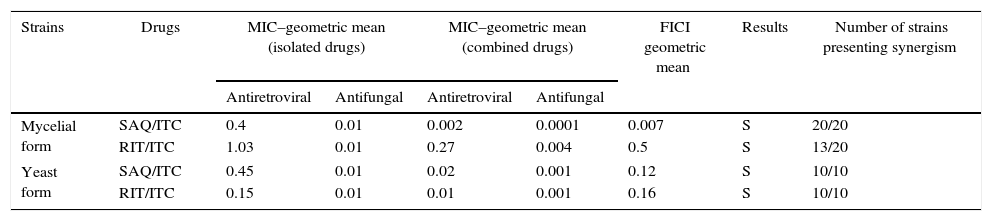
Synergistic interactions were observed for the combinations of saquinavir or ritonavir with itraconazole, and there was a significant reduction in the MIC of these drugs: saquinavir (p=0.0000) and itraconazole (p=0.0000) for filamentous and yeast phases; and ritonavir (p=0.0001) and itraconazole (p=0.0003) for filamentous phase and ritonavir (p=0.0297) and itraconazole (p=0.0015) for yeast phase (Table 2). No antagonistic interactions were observed.
Effects of the combination of antiretroviral drugs and itraconazole on strains of H. capsulatum var. capsulatum in yeast-like and mycelial forms.
| Strains | Drugs | MIC–geometric mean (isolated drugs) | MIC–geometric mean (combined drugs) | FICI geometric mean | Results | Number of strains presenting synergism | ||
|---|---|---|---|---|---|---|---|---|
| Antiretroviral | Antifungal | Antiretroviral | Antifungal | |||||
| Mycelial form | SAQ/ITC | 0.4 | 0.01 | 0.002 | 0.0001 | 0.007 | S | 20/20 |
| RIT/ITC | 1.03 | 0.01 | 0.27 | 0.004 | 0.5 | S | 13/20 | |
| Yeast form | SAQ/ITC | 0.45 | 0.01 | 0.02 | 0.001 | 0.12 | S | 10/10 |
| RIT/ITC | 0.15 | 0.01 | 0.01 | 0.001 | 0.16 | S | 10/10 | |
SAQ=saquinavir; RIT=ritonavir; ITC=itraconazole; S=synergistic interaction.
In recent years, studies have shown that HIV patients can have substantially longer life expectancy, depending on adherence to antiretroviral treatment and the evolution of the immune status. Also, the use of more effective therapy decreases the incidence of opportunistic infections, including histoplasmosis. Even though the use of protease inhibitors, including saquinavir, has been associated with the development of several side effects, recent studies have demonstrated that the use of liposome saquinavir formulations significantly decreases the levels of cytotoxicity, besides improving the bioavailability of this drug.16
Moreover, it has been observed that the protease inhibitors can have beneficial effects on some fungal infections, not only by modulating the immune system of the susceptible host, but also by exerting direct action against the pathogen.17 It has also been observed from in vitro and in vivo studies that protease inhibitors reduce the pathogenicity and growth of C. albicans probably because these drugs act directly on the production of the enzyme aspartyl-proteinases, which is secreted by this organism in the processes of invasion and colonization of host tissues.18–20 Additionally, it has been shown that ritonavir inhibits the in vitro hyphal growth rate of C. albicans,21 ritonavir and saquinavir inhibit the adherence of C. albicans to endothelial cells,22 and saquinavir, ritonavir, and indinavir attenuate the in vitro adherence of C. albicans to acrylic substances, which is a common component of oral appliances.23
More recently, it was observed that the protease inhibitors saquinavir, darunavir, ritonavir, and indinavir did not reduce the in vitro growth of C. neoformans, but reduced protease activity as well as capsule production, important virulence factors of C. neoformans.24 Although there are some studies on the action of protease inhibitors against fungi, no reports for H. capsulatum have been published so far.
In the present study, we observed that the protease inhibitors saquinavir and ritonavir alone inhibited H. capsulatum, and saquinavir and ritonavir interacted synergistically with itraconazole, as evidenced by the increased in vitro activity of the antifungal drug. The advantage of the synergistic effect of the combination of antiretroviral and antifungal drugs aims to attenuate toxic effects caused by them, especially in cases of long-term therapies, such as in HIV-infected patients presenting with histoplasmosis.2
Casolari et al.25 found that saquinavir alone did not show significant antifungal activity against the yeast forms of C. albicans and C. neoformans. However, when combined with the azole drug fluconazole, it was found to inhibit the growth of these fungal species, indicating the occurrence of synergism between the drugs. Similarly, Palmeira et al.26 described the effect of nelfinavir and saquinavir against the dematious fungus Fonsecaea pedrosoi and confirmed that these compounds alone were unable to inhibit the growth of this fungus. However, inhibition did occur when sub-inhibitory doses of these protease inhibitors were combined with amphotericin B. Mikus et al.27 noted that ritonavir prolongs the clearance of voriconazole, although the use of ritonavir with voriconazole is contraindicated because the former lowers the plasma levels of voriconazole.
Our data demonstrated an in vitro synergistic interaction between saquinavir or ritonavir with itraconazole against the dimorphic fungus H. capsulatum. The mechanism underlying the observed synergy remains unknown, but Crommentuyn et al.28 showed that the in vivo combination of antiretroviral lopinavir/ritonavir and itraconazole interacts through pharmacokinetic pathways, interfering with the metabolism of the antifungal drug, which increases the plasma level of the antifungal agent, thus, making it possible to reduce the dosage of itraconazole without impairing the treatment. Based on our findings, we believe that saquinavir or ritonavir with itraconazole interact probably through pharmacodynamic pathways.
These data show an important in vitro synergy between saquinavir or ritonavir and itraconazole against the fungus H. capsulatum, which is an important pathogen for AIDS patients.
Conflicts of interestThe authors declare no conflicts of interest.
This research was supported by CNPq process (303396/2014-8; 552161/2011-0) and CAPES (AE1 – 0052-000630100/11).