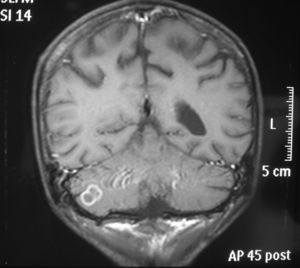
A 29-year-old male patient was admitted at the hospital with complaints of diarrhea and weight loss that had started two months ago. In his physical examination and laboratory tests, HIV positivity was detected (CD4 cell count 175mL–1, HIV RNA 9,800,000copies/mL). At the end of the first month of antiretroviral therapy he was admitted to the hospital again with deterioration in his general medical condition, respiratory distress and loss of consciousness. Massive pleural effusion in the right hemithorax, and diffuse bilateral micronodular infiltration in both lungs were detected by thoracic computerized tomographic (CT) examination (Fig. 1). A lesion (tuberculoma) was observed in the cranial magnetic resonance imaging (MRI) (Fig. 2). There were hypodense nodular lesions in the liver and spleen, and mesenchymal multiple lymphadenopathy (LAP) in the abdominal CT (Fig. 3). Mycobacterium tuberculosis grew on the 35th day after pleural fluid culture in Löwenstein Jensen culture media. Treatment with antituberculosis agents and 60mg prednisolone was started. Bilateral distal motor and sensory neuropathy developed during follow-up. Multiple nodular lesions (tuberculomas) were detected in the spine in spinal MRI (Fig. 4).1 The patient was discharged on the second month of treatment with partial recovery.
Initiation of antiretroviral therapy (ART) in HIV-infected patients leads to restoration of the immune functions. On the other hand, dysregulated immune response after initiation of ART leads to the phenomenon of Immune Reconstitution Inflammatory Syndrome (IRIS). IRIS is paradoxical worsening of an existing infection or appearance of a new infection soon after initiation of ART.2,3
Conflicts of interestThe authors declare no conflicts of interest.