The elderly population is increasingly benefiting from recent technological advances. In this scenario, geolocation-based dating applications provide a viable alternative for finding partners in a practical and timely manner, but may be accompanied by certain risk behaviors for HIV infection. Although there are considerable number of users over 50 on these applications, no studies have addressed this problem. The aim of the present study was to analyze factors of vulnerability to HIV/Aids among the population of men who have sex with men (MSM) age 50 years or older who use dating apps.
MethodsThis was a cross-sectional, population-survey-based, analytical study, conducted exclusively online with a sample of 412 MSM. The data was collected from the following apps: Grindr®, Hornet®, Scruff® and Daddy Hunter®.
ResultsFactors associated with a higher chance of having HIV were: sexual relations with an HIV-infected partner (ORa=5.53; 95%CI=2.23–13.73); chemsex (ORa=3.97; 95%CI=1.72–8.92); and, above all, having an HIV-infected partner (ORa=8.02; 95%CI=2.01–32.01). The belief that apps increase protection against sexually transmitted infections (ORa=0.43; 95%CI=0.19–0.95) and not being familiar with post-exposure prophylaxis (ORa=0.43; 95%CI=0.19–0.95) were associated with decreased chances of having HIV.
ConclusionsWe highlight some important factors that structure the vulnerability of the MSM surveyed in relation to HIV infection. The findings should be used to customize care for this population, which could bring them in more for health care services.
In recent decades, the population of middle-aged and older men (50 years or older) has enjoyed the benefits of improved quality of life, which has increased their life expectancy. Furthermore, technological advances in the field of medicine, especially those relative to hormone replacement treatment and erectile dysfunction medications, have allowed these men to continue to be sexually active.1
Aging and the expression of sexuality commonly refer to the confluence between body and culture and are considered mutually exclusive in Western societies, especially because of the loss of physical activity and the sense of asexuality experienced in old age. However, nowadays, these ideas are constantly challenged. This conflict reaches its apex when considering male gay culture, which is marked by complacent hedonism associated with being obsessed with physical attributes capable of eliciting attraction and desire.2,3
As part of this rediscovery of their own bodies and sexuality, middle-aged and older men who have sex with men (MSM) have gradually freed themselves of the social restrictions and norms historically imposed on people of this age regarding sexuality, recreating and remodeling norms to better suit their experiences, sexual needs, and desires.4
The use of online digital social media, especially geosocial dating apps for sexual purposes, helps meet the demand of this male population, providing an effective and convenient mechanism to quickly locate sexual partners, in comparison with other, more traditional or offline methods.5,6
These mobile apps allow users to filter possible partners according to their preferences (age, sex positions, race, and physical attributes, among others), streamlining the creation of partnerships, especially sexual.5,6 This agility in establishing partnerships, however, can contribute to condomless anal sex and other practices that can increase exposure to sexually transmitted infections (STIs), especially the human immunodeficiency virus (HIV).7,8 Furthermore, lack of discussions about the sexual health of MSM aged 50 years or older contributes to this scenario, because it reinforces the invisibility of the LGBT community and the sexuality of older persons.9
The literature about factors related to HIV infection among middle-aged and older MSM is scarce, especially when considering the use of social media, even though data from international offices, such as the US Centers for Disease Control, show that the incidence of the infection has grown considerably among the MSM population.9–12 The contextual factors that could explain this population’s greater vulnerability to HIV are still unknown. The objective of the present study was to analyze factors of vulnerability to HIV/Aids among the population of MSM aged 50 years or older who use dating apps.
The concept of vulnerability adopted here consists of three fundamental aspects or dimensions—individual, social, and programmatic—that are used to describe the susceptibility of population groups to important health problems. In the context of the HIV/Aids epidemic, vulnerability is related to the idea that people’s chances of being exposed to the virus (and of developing Aids) are the result of a set of individual, collective, and contextual aspects, which together lead to greater susceptibility to infection and disease.13
Individual vulnerability is of a cognitive nature and includes biological, emotional, cognitive and attitudinal aspects relative to social relationships, understood as the quantity and quality of the information available to individuals, in association with their ability to process it. The social aspect of vulnerability is defined by cultural, social, and economic aspects that determine people’s opportunities to access goods and services. Programmatic (healthcare) vulnerability refers to the necessary social resources to protect individuals from risks to their physical, psychological, and social integrity and well-being. Any study of vulnerability depends on the analysis of the combination of the three domains.14
MethodsThis article is part of a multicenter study called “Behaviors, practices, and vulnerabilities among men who have sex with men and use geolocation (geosocial) dating apps in Brazil”. It was a cross-sectional, population-survey-based, analytical study carried out with MSM aged 50 years or older who use dating apps, conducted exclusively online in all the regions of Brazil.
SampleFor sample definition we used a modification of time location sampling (TLS). This technique seeks to approach probabilistic sampling by mapping the universe of places where the target population can be found in large numbers and then randomly selecting a specific day, time and place for recruitment and systematically selecting participants from that location.15 Volunteers who were specifically approached through the applications and who agreed to respond to the online questionnaire were considered. The inclusion criteria were: identified as a cisgender male; being 50 years or older; and being online at the time of data collection. Users who did not reside in Brazil were excluded.
Specific proceduresTo find participants, four apps commonly used by MSM were selected: Grindr®, Hornet®, Scruff® and Daddy Hunter®.8 The computer-assisted self-interview (CASI) technique was used for data gathering.15 The participants were approached through the selected apps for four consecutive months (February to May of 2017), in the afternoon, evening and at night. The participants were informed about the research objectives and the importance of their participation. After gaining consent, the researchers shared the hyperlink to the survey form, where the participants answered specific questions of interest to this study.
To cover the participants’ social and demographic characteristics, sexual behavior, and health information, the questionnaire was divided into four sections, which included both mandatory and optional questions: personal information; sociocultural information; health issues; and sexual practices. The system only allowed participants to proceed to the next section if all the mandatory questions were answered. Furthermore, the questionnaires were only computed if, at the end, all the conditions were met. Incomplete surveys were not saved by the system.
To answer the questionnaire, participants provided their email address, preventing duplicated entries. If a participant was unwilling to participate, the next online user was approached. Recruitment was conducted by two adult cisgender male researchers who are experts in the studied field. They created accounts with public profiles (open, with a photo) in the apps to gain access to the users.
The analysis of the data was based on the adopted vulnerability framework.13,14 The research variables were grouped according to the three domains of vulnerability:
- 1)
Individual: age, marital status, living situation, number of partners, type of sexual partnership established, sexual practices (sex positions, consistent use of condoms, bareback sex, group sex), forms of prevention (condoms, withdrawal, no penetration), chemsex (using drugs during sexual relations), use of erectile dysfunction drugs, and the presence of STIs;
- 2)
Social: educational level, sexual orientation, religion and going to saunas; and
- 3)
Health care (programmatic): being familiar with post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP); going to healthcare services; and prior testing for HIV.
Variables that allowed more than one response, such as prevention and sexual position, were presented to the participants in multiple-choice format.
Data analysisDescriptive analysis was employed to describe the vulnerability factors and other factors of interest, for both the numerical and categorical variables. The data were analyzed using IBM® SPSS version 23.0. Associations between positive serological status for HIV and the categorized vulnerability factors were assessed using the Pearson’s chi-squared test and Fisher’s exact test, with a 0.05 significance level. To construct the confidence interval, the reliability was set at 95%. The outcome of interest was positive HIV status, which was assessed using the question: Do you know your HIV status? The answer options were: "I am HIV positive", "I am HIV negative", and "I do not know/I'm not sure".
Multivariate logistic model was adopted to produce the adjusted odds ratios (ORa), considering the factors that presented statistical significance in univariate analysis.
Ethical aspectsThe study was approved by the CEP/CONEP system (no. 1.523.003) and strictly complied with all the ethical precepts that guide research with human subjects. The participants read the free and informed consent form and then signed it, indicating their agreement with the proposed objectives and willingness to participate in the study. This consent was applied and obtained online.
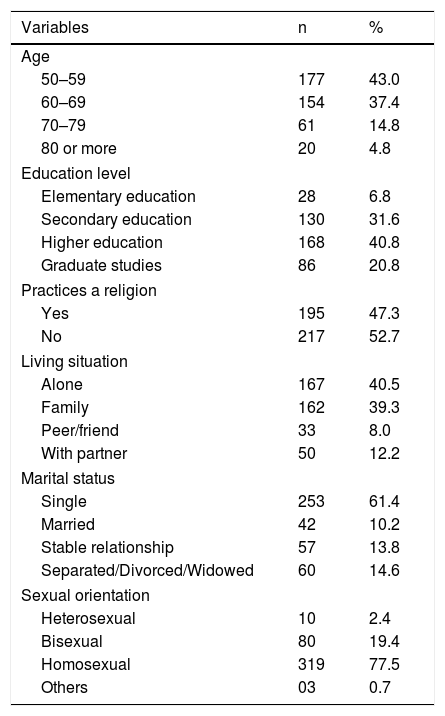
ResultsIn all, 412 participants were recruited; Table 1 shows their sociodemographic characteristics. There was a predominance of individuals between 50 and 59 years old (42%), mean age of 61.6 years (ranging between 50 and 97, SD=9.2). Most had a higher education (61.7%) and did not practice any religion (52.7%). Most were single (61.4%), had not been in a relationship in the last 30 days (71.1%), identified themselves as homosexuals (77.4%), and lived alone (40.5%).
Sociodemographic characteristics of men aged 50 years or older who have sex with men (MSM) and use dating apps. Brazil, 2017.
| Variables | n | % |
|---|---|---|
| Age | ||
| 50–59 | 177 | 43.0 |
| 60–69 | 154 | 37.4 |
| 70–79 | 61 | 14.8 |
| 80 or more | 20 | 4.8 |
| Education level | ||
| Elementary education | 28 | 6.8 |
| Secondary education | 130 | 31.6 |
| Higher education | 168 | 40.8 |
| Graduate studies | 86 | 20.8 |
| Practices a religion | ||
| Yes | 195 | 47.3 |
| No | 217 | 52.7 |
| Living situation | ||
| Alone | 167 | 40.5 |
| Family | 162 | 39.3 |
| Peer/friend | 33 | 8.0 |
| With partner | 50 | 12.2 |
| Marital status | ||
| Single | 253 | 61.4 |
| Married | 42 | 10.2 |
| Stable relationship | 57 | 13.8 |
| Separated/Divorced/Widowed | 60 | 14.6 |
| Sexual orientation | ||
| Heterosexual | 10 | 2.4 |
| Bisexual | 80 | 19.4 |
| Homosexual | 319 | 77.5 |
| Others | 03 | 0.7 |
The most common type of sexual partnership established was casual (63.1%), which resulted in a mean of 2.7 sexual partnerships via the apps in the 30 days prior to the survey. The most popular apps were Grindr (59.7%) and Hornet (45.1%), which were used primarily to facilitate sexual encounters (88%).
Regarding frequency of use, emphasis goes to the daily use of the apps (60%), especially in the evening (63%) and on weekdays (64.8%). In terms of the presence of STIs, 22.1% reported at least one in the year prior to the survey, with emphasis on infection by HIV (11.7%) and syphilis (10.2%).
The most common form of prevention was condoms (86.2%). However, it is worth noting that 38% opted for withdrawal. Furthermore, 31.3% of the participants chose the insertive sexual position exclusively, 27.7%, the receptive sexual position exclusively, and 33.5%, both (versatile). Among those who had receptive intercourse, 25.7% had done so condomless at least once in the 30 days prior to the survey. HIV prevalence was 11.7% (48), and 30.8% (127) did not know their serological status. Also noteworthy is the fact that 47.3% (195) of the subjects had not had HIV testing recently (in the previous 12 months).
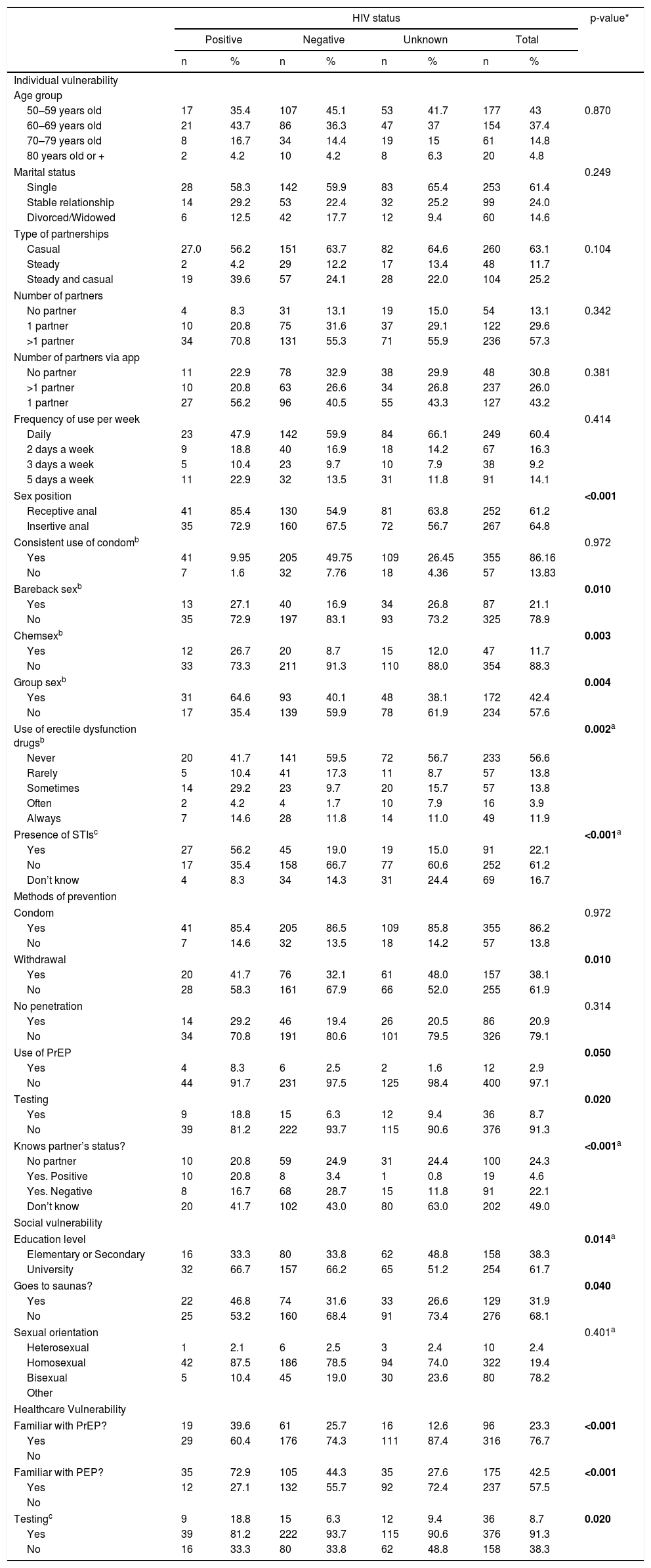
Univariate analysis of positive serological status for HIV showed associations with the following factors: educational level (p=0.039); sex position (p<0.001); HIV testing (p=0.020); bareback practice (p=0.010); chemsex (p=0.003); group sex (p=0.004); use of erectile dysfunction drugs (p=0.002); presence of STIs (p<0.001); knowledge of PEP (p<0.001) and PrEP (p<0.001); going to saunas (p=0.040); using withdrawal (p=0.010) as a form of prevention; use of PrEP (p=0.050) and testing (p=0.020); and knowing the partners’ status (p<0.001) (Table 2).
HIV serological status according to vulnerability factors. Brazil, 2017.
| HIV status | p-value* | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Unknown | Total | ||||||
| n | % | n | % | n | % | n | % | ||
| Individual vulnerability | |||||||||
| Age group | |||||||||
| 50–59 years old | 17 | 35.4 | 107 | 45.1 | 53 | 41.7 | 177 | 43 | 0.870 |
| 60–69 years old | 21 | 43.7 | 86 | 36.3 | 47 | 37 | 154 | 37.4 | |
| 70–79 years old | 8 | 16.7 | 34 | 14.4 | 19 | 15 | 61 | 14.8 | |
| 80 years old or + | 2 | 4.2 | 10 | 4.2 | 8 | 6.3 | 20 | 4.8 | |
| Marital status | 0.249 | ||||||||
| Single | 28 | 58.3 | 142 | 59.9 | 83 | 65.4 | 253 | 61.4 | |
| Stable relationship | 14 | 29.2 | 53 | 22.4 | 32 | 25.2 | 99 | 24.0 | |
| Divorced/Widowed | 6 | 12.5 | 42 | 17.7 | 12 | 9.4 | 60 | 14.6 | |
| Type of partnerships | |||||||||
| Casual | 27.0 | 56.2 | 151 | 63.7 | 82 | 64.6 | 260 | 63.1 | 0.104 |
| Steady | 2 | 4.2 | 29 | 12.2 | 17 | 13.4 | 48 | 11.7 | |
| Steady and casual | 19 | 39.6 | 57 | 24.1 | 28 | 22.0 | 104 | 25.2 | |
| Number of partners | |||||||||
| No partner | 4 | 8.3 | 31 | 13.1 | 19 | 15.0 | 54 | 13.1 | 0.342 |
| 1 partner | 10 | 20.8 | 75 | 31.6 | 37 | 29.1 | 122 | 29.6 | |
| >1 partner | 34 | 70.8 | 131 | 55.3 | 71 | 55.9 | 236 | 57.3 | |
| Number of partners via app | |||||||||
| No partner | 11 | 22.9 | 78 | 32.9 | 38 | 29.9 | 48 | 30.8 | 0.381 |
| >1 partner | 10 | 20.8 | 63 | 26.6 | 34 | 26.8 | 237 | 26.0 | |
| 1 partner | 27 | 56.2 | 96 | 40.5 | 55 | 43.3 | 127 | 43.2 | |
| Frequency of use per week | 0.414 | ||||||||
| Daily | 23 | 47.9 | 142 | 59.9 | 84 | 66.1 | 249 | 60.4 | |
| 2 days a week | 9 | 18.8 | 40 | 16.9 | 18 | 14.2 | 67 | 16.3 | |
| 3 days a week | 5 | 10.4 | 23 | 9.7 | 10 | 7.9 | 38 | 9.2 | |
| 5 days a week | 11 | 22.9 | 32 | 13.5 | 31 | 11.8 | 91 | 14.1 | |
| Sex position | <0.001 | ||||||||
| Receptive anal | 41 | 85.4 | 130 | 54.9 | 81 | 63.8 | 252 | 61.2 | |
| Insertive anal | 35 | 72.9 | 160 | 67.5 | 72 | 56.7 | 267 | 64.8 | |
| Consistent use of condomb | 0.972 | ||||||||
| Yes | 41 | 9.95 | 205 | 49.75 | 109 | 26.45 | 355 | 86.16 | |
| No | 7 | 1.6 | 32 | 7.76 | 18 | 4.36 | 57 | 13.83 | |
| Bareback sexb | 0.010 | ||||||||
| Yes | 13 | 27.1 | 40 | 16.9 | 34 | 26.8 | 87 | 21.1 | |
| No | 35 | 72.9 | 197 | 83.1 | 93 | 73.2 | 325 | 78.9 | |
| Chemsexb | 0.003 | ||||||||
| Yes | 12 | 26.7 | 20 | 8.7 | 15 | 12.0 | 47 | 11.7 | |
| No | 33 | 73.3 | 211 | 91.3 | 110 | 88.0 | 354 | 88.3 | |
| Group sexb | 0.004 | ||||||||
| Yes | 31 | 64.6 | 93 | 40.1 | 48 | 38.1 | 172 | 42.4 | |
| No | 17 | 35.4 | 139 | 59.9 | 78 | 61.9 | 234 | 57.6 | |
| Use of erectile dysfunction drugsb | 0.002a | ||||||||
| Never | 20 | 41.7 | 141 | 59.5 | 72 | 56.7 | 233 | 56.6 | |
| Rarely | 5 | 10.4 | 41 | 17.3 | 11 | 8.7 | 57 | 13.8 | |
| Sometimes | 14 | 29.2 | 23 | 9.7 | 20 | 15.7 | 57 | 13.8 | |
| Often | 2 | 4.2 | 4 | 1.7 | 10 | 7.9 | 16 | 3.9 | |
| Always | 7 | 14.6 | 28 | 11.8 | 14 | 11.0 | 49 | 11.9 | |
| Presence of STIsc | <0.001a | ||||||||
| Yes | 27 | 56.2 | 45 | 19.0 | 19 | 15.0 | 91 | 22.1 | |
| No | 17 | 35.4 | 158 | 66.7 | 77 | 60.6 | 252 | 61.2 | |
| Don’t know | 4 | 8.3 | 34 | 14.3 | 31 | 24.4 | 69 | 16.7 | |
| Methods of prevention | |||||||||
| Condom | 0.972 | ||||||||
| Yes | 41 | 85.4 | 205 | 86.5 | 109 | 85.8 | 355 | 86.2 | |
| No | 7 | 14.6 | 32 | 13.5 | 18 | 14.2 | 57 | 13.8 | |
| Withdrawal | 0.010 | ||||||||
| Yes | 20 | 41.7 | 76 | 32.1 | 61 | 48.0 | 157 | 38.1 | |
| No | 28 | 58.3 | 161 | 67.9 | 66 | 52.0 | 255 | 61.9 | |
| No penetration | 0.314 | ||||||||
| Yes | 14 | 29.2 | 46 | 19.4 | 26 | 20.5 | 86 | 20.9 | |
| No | 34 | 70.8 | 191 | 80.6 | 101 | 79.5 | 326 | 79.1 | |
| Use of PrEP | 0.050 | ||||||||
| Yes | 4 | 8.3 | 6 | 2.5 | 2 | 1.6 | 12 | 2.9 | |
| No | 44 | 91.7 | 231 | 97.5 | 125 | 98.4 | 400 | 97.1 | |
| Testing | 0.020 | ||||||||
| Yes | 9 | 18.8 | 15 | 6.3 | 12 | 9.4 | 36 | 8.7 | |
| No | 39 | 81.2 | 222 | 93.7 | 115 | 90.6 | 376 | 91.3 | |
| Knows partner’s status? | <0.001a | ||||||||
| No partner | 10 | 20.8 | 59 | 24.9 | 31 | 24.4 | 100 | 24.3 | |
| Yes. Positive | 10 | 20.8 | 8 | 3.4 | 1 | 0.8 | 19 | 4.6 | |
| Yes. Negative | 8 | 16.7 | 68 | 28.7 | 15 | 11.8 | 91 | 22.1 | |
| Don’t know | 20 | 41.7 | 102 | 43.0 | 80 | 63.0 | 202 | 49.0 | |
| Social vulnerability | |||||||||
| Education level | 0.014a | ||||||||
| Elementary or Secondary | 16 | 33.3 | 80 | 33.8 | 62 | 48.8 | 158 | 38.3 | |
| University | 32 | 66.7 | 157 | 66.2 | 65 | 51.2 | 254 | 61.7 | |
| Goes to saunas? | 0.040 | ||||||||
| Yes | 22 | 46.8 | 74 | 31.6 | 33 | 26.6 | 129 | 31.9 | |
| No | 25 | 53.2 | 160 | 68.4 | 91 | 73.4 | 276 | 68.1 | |
| Sexual orientation | 0.401a | ||||||||
| Heterosexual | 1 | 2.1 | 6 | 2.5 | 3 | 2.4 | 10 | 2.4 | |
| Homosexual | 42 | 87.5 | 186 | 78.5 | 94 | 74.0 | 322 | 19.4 | |
| Bisexual | 5 | 10.4 | 45 | 19.0 | 30 | 23.6 | 80 | 78.2 | |
| Other | |||||||||
| Healthcare Vulnerability | |||||||||
| Familiar with PrEP? | 19 | 39.6 | 61 | 25.7 | 16 | 12.6 | 96 | 23.3 | <0.001 |
| Yes | 29 | 60.4 | 176 | 74.3 | 111 | 87.4 | 316 | 76.7 | |
| No | |||||||||
| Familiar with PEP? | 35 | 72.9 | 105 | 44.3 | 35 | 27.6 | 175 | 42.5 | <0.001 |
| Yes | 12 | 27.1 | 132 | 55.7 | 92 | 72.4 | 237 | 57.5 | |
| No | |||||||||
| Testingc | 9 | 18.8 | 15 | 6.3 | 12 | 9.4 | 36 | 8.7 | 0.020 |
| Yes | 39 | 81.2 | 222 | 93.7 | 115 | 90.6 | 376 | 91.3 | |
| No | 16 | 33.3 | 80 | 33.8 | 62 | 48.8 | 158 | 38.3 | |
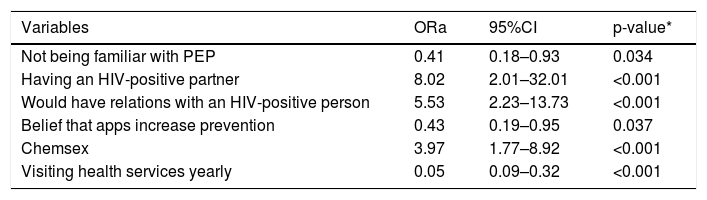
Multivariate analysis revealed that the following variables were independently associated with increased chances of having HIV: having relations with someone with HIV (ORa=5.53; 95%CI=2.23–13.73); chemsex (ORa=3.97; 95%CI=1.72–8.92); and, especially, having a partner with HIV (ORa=8.02; 95%CI=2.01–32.01). The belief that apps increase protection against STIs (ORa=0.43; 95%CI=0.19–0.95) and not being familiar with PEP (ORa=0.43; 95%CI=0.19–0.95) were associated with reduced chances of having HIV (Table 3).
Multivariate analysis of factors associated with vulnerability to HIV infection by MSM aged 50 years or older and who use dating apps. Brazil, 2017.
| Variables | ORa | 95%CI | p-value* |
|---|---|---|---|
| Not being familiar with PEP | 0.41 | 0.18–0.93 | 0.034 |
| Having an HIV-positive partner | 8.02 | 2.01–32.01 | <0.001 |
| Would have relations with an HIV-positive person | 5.53 | 2.23–13.73 | <0.001 |
| Belief that apps increase prevention | 0.43 | 0.19–0.95 | 0.037 |
| Chemsex | 3.97 | 1.77–8.92 | <0.001 |
| Visiting health services yearly | 0.05 | 0.09–0.32 | <0.001 |
The results showed a high prevalence of HIV among MSM aged 50 years or older (11.7%) who are users of dating apps in Brazil, especially when compared with the general Brazilian population (0.39%).16 However, this prevalence is still lower than that found in a recent study with MSM in 12 Brazilian cities, which reported a prevalence of 18.4%.17 It is worth noting that these studies used different methodological approaches to estimate prevalence rates.
The prevalence in our study was also lower than in other studies conducted with MSM in Latin America. A study conducted in large urban centers in Colombia revealed a prevalence of 15%,18 while another carried out in Mexico showed a prevalence of 16.9%.19However, these two studies addressed young MSM, with mean ages of 29.7 and 25 years, respectively. These rates are quite elevated when compared to HIV prevalence among MSM in European countries (6.0%).20
In Brazil, there is little information about the HIV epidemic and risk and vulnerability factors for STIs and HIV infection among MSM over 50 years old. The most recent studies have found prevalence rates and other information about the general population of MSM, with a small representation of men in older age groups.8,15,17
In the international literature there are also few studies that focus on this MSM subgroup, which limits knowledge about the specific characteristics of these men and makes their vulnerability and health conditions invisible.21–23 To our knowledge, this is the first study to provide original data focusing on the vulnerability factors for HIV infection among MSM aged 50 and older who are users of geosocial dating applications. Studies previously carried out on this subject have concentrated on the general MSM population (young/adult).5
The sociodemographic profile of the study participants revealed that most were homosexual and presented high educational levels (university degree), a finding similar to that in a recent literature review.5 This profile can help MSM better manage their vulnerabilities, because when equipped with knowledge and other resources, they are able to select the prevention strategies that better fit their lifestyle.15 There was also a predominance of participants who lived alone or who were not in a stable relationship, a factor that can influence their social support.20
App use profile – social vulnerabilityAlthough most of the social vulnerability factors related to app use did not present statistical significance in the multivariate analysis, it is important to discuss these findings, since they differed from other studies24 and have direct implications for the sexual practices of MSM. Analysis of app use showed characteristics that clearly defined differences between the consumption of different generations of MSM, which can contribute to the understanding of some aspects of these men’s vulnerability. For example, in relation to reasons for using these apps, younger MSM used them for sexual purposes (64.7%),8 a lower rate than that found among MSM aged 50 years or older (88.0%). This may reflect the importance of this tool in the daily lives of the participants and corroborates other studies indicating that older adults tend to better adopt technologies that serve specific objectives.25,26
These factors can affect the sexual behavior of users because the more an app is used, the greater the familiarity with its tools, and the greater the ease and speed of finding partners, as evidenced by previous studies.5,27,28 This familiarity can influence the speed and ability of establishing partnerships. A study revealed that the average time of use of these apps among youths was 50% less than among participants of the present study (12 months and 27 months, respectively).5 Accordingly, the number of partnerships established through the apps was also higher in the present study (2.7 partners in the last 30 days) when compared with other studies with younger MSM who used apps in the United States (2.03 and 1.9).29,30
It is important to highlight that the safety that comes from the anonymity and discretion provided by the apps is useful for some MSM, especially those who identify themselves as heterosexual or bisexual and who do not choose to disclose their affective and sexual behavior to protect themselves against violence, stigma, discrimination, homophobia and family rejection.31,32 The use of new digital technologies makes it easier to contact friends and establish new relationships (affective and sexual), and this is constantly being updated. Consequently, new issues emerge, such as relationships between older and younger MSM.33
It is worth remembering that “believing that apps help prevent HIV infection,” that is, believing that using apps to establish partnerships can somehow help prevent HIV infection, was statistically associated with being a protecting factor against HIV infection. In other words, the participants perceived that this form of digital interaction mediated by social media can somehow help prevent infections.
Individual vulnerabilityThe sex position preferred by men, whether insertive or receptive, is an important factor in the sexual experience of MSM. Preference for the insertive position (insertive-only or versatile-insertive position) is associated with an image of greater masculinity, which is highly valued in gay sociability,34–36 and also presents a lower risk of infection by HIV and STIs.20,37
Even though the participants in the present study reported preferring the insertive position, other risk factors for HIV (Table 2) presented high frequency, which can increase the chances of transmission of HIV.38 These results were similar to those found in the literature, where many of the findings of the present study (erection difficulties, using condoms only with casual partners and not with steady partners or when engaging in chemsex) are factors associated with HIV infection among MSM.39,40
However, there is also evidence that people with undetectable HIV viral load, or who use PrEP, can maintain safe sexual relations even with serodiscordant partners.41 The repertoire of sexual practices involves factors from the individual dimension of vulnerability, issues that must be addressed to prevent HIV and STIs,42 because “not being familiar with PEP,” “having a partner with HIV,” and openness to “having relations with someone with HIV” and “chemsex” emerged as significantly associated with HIV infection in this study.
Chemsex is a differentiated, non-unitary and intentional sexual behavior that combines sexual activity and consumption of psychoactive substances. This is an important factor associated with positive HIV status, and has recently been addressed by the literature, which has identified an increase in this behavior among MSM.43 Among the reasons for this increase are growing capacity for engaging in the desired form of sex (increased arousal and libido, sexual confidence and increased sexual stamina), coupled with the improvement of qualities valued in sex, such as intensified sensation, reduced inhibitions, and greater ease of having sexual adventures.44
These effects are due to the substances used in chemsex, which provide men with the ability to improve their performance and sexual experiences, increasing arousal, endurance, and pleasure. For older men, the invigorating effect of these substances seems to be the main motivation for their use, enabling improved sexual performance that corresponds to the ideals of masculinity shared by the gay community, especially when having relations with younger partners.45
Programmatic vulnerabilityIn Brazil, MSM face difficulties when accessing health services because of issues relative to stigma and social violence, in addition to discrimination suffered in health services.46 Even though a set of national health policies is directed toward the LGBT community,47 effective implementation of these services and reducing discrimination are still a challenge for the Brazilian Unified Health System.48 The results of the present study showed that “visiting health services at least once a year” was a protective factor against HIV infection, which reinforces the importance of improving access to health services for these men.
One of the important issues in the context of the HIV epidemic that still need to be addressed is late diagnosis of HIV infection among MSM,46 especially those over 50 years old,49,50 since this is an important marker for access to HIV and STI prevention strategies in health services.46,51 Programmatic vulnerability is associated with barriers to access to health services, which are still discriminatory environments for MSM, in addition to flaws in prevention policies, since dissemination of and access to these services and supplies for MSM is still notably limited.
It is imperative that Brazilian society and public health managers face the reality of the vulnerability of MSM presented by various studies in terms of the HIV and Aids epidemics. It is urgent that existing health policies be implemented, and efforts be made to strengthen prevention and intervention actions that effectively reduce the spread of HIV and Aids in Brazil.
The present study has some limitations: a convenience sample consisting of MSM aged 50 years or older was used; a portion of the key variables for the study (testing and HIV status) were self-reported; incomplete responses were not saved in Google Forms; and the finding that the majority of participants in this study had a high level of education.
Furthermore, the study was limited to reporting findings for a specific population who used mobile social networks for given purposes, which can influence results and hinder generalizations about the MSM population over 50 years who do not use these apps. Much of the discussion was based on research involving younger MSM, due to lack of research with MSM 50 years old or older who are users of dating apps.
Despite these limitations, the results effectively reflect important aspects of individual, social and healthcare vulnerabilities of MSM aged 50 years and older in Brazil.
ConclusionA high prevalence of HIV was observed among MSM 50 years old and older who use dating apps. Furthermore, some of the factors that affect vulnerability of MSM regarding HIV infection were: types of partnership established; partner’s serological status; knowledge of prevention measures; chemsex; educational levels; sex position; group sex; presence of STIs and the use of PrEP; use of erectile dysfunction drugs; going to saunas; prevention through withdrawal; and frequency of visits to health services and HIV testing.
Authors’ contributionsAAFLNQ and AFLS contributed to design and execution of the study. TMEA, SB and RKR contributed to execution of the study. All authors contributed to the interpretation of findings, read and approved the final version of the article for submission.
Conflicts of interestThe authors declare no conflicts of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.