An interesting case of pyogenic vertebral osteomyelitis with multiple epidural abscesses caused by non-pigmented Prevotella oralis is reported. The patient was a 68-year-old female who presented to the emergency room (ER) with severe pain and tenderness in her lower back with fever. She had recently undergone esophagogastroduodensoscopy (EGD) for complaints of esophageal reflux, which showed submucosal cyst in the esophagus. Magnetic resonance imaging (MRI) of the thoracic spine revealed multiple spinal epidural abscesses with signal enhancement at the level of T6 and T7, suggestive of vertebral osteomyelitis. Two blood cultures drawn one hour apart grew Prevotella oralis. The body fluid aspirated from the abscesses was also positive for the anaerobic commensal P. oralis. Necrosis associated with the submucosal cyst was implicated as the cause of sepsis and osteomyelitis due to this organism.
Vertebral osteomyelitis is a rare cause of back pain in adults. The usual implicated organisms are Staphylococcus aureus, beta hemolytic Streptococcus, and Viridans Streptococci.1 Anaerobic Gram-negative bacilli (AGNB) are a rare cause of vertebral osteomyelitis and amongst the AGNB, Prevotella is an extremely rare etiological agent. The Prevotella genus is further classified into pigmented and non-pigmented species, based on production of pigmented colonies on blood agar.2 Here, an interesting case of pyogenic vertebral osteomyelitis with multiple epidural abscesses caused by non-pigmented Prevotella oralis is reported. To the authors’ knowledge, this is the first reported case of pyogenic vertebral osteomyelitis caused by non-pigmented P. oralis.
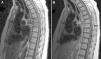
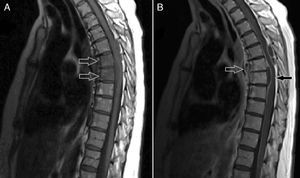
Case presentationA 68-year-old female was referred by her primary physician to the ER for evaluation and management of severe pain in her back along the rib cage, which radiated towards the anterior abdominal wall. She reported that the pain was 10/10 in intensity, sharp in quality, continuous, and increased with movements. She also complained of mild fever with lethargy. She denied weakness of the limbs and fecal or urinary incontinences. The patient had past medical history of hypertension and gastroesophageal reflux disease (GERD). She had undergone esophagogastroduodensoscopy (EGD) two weeks prior, which was positive for submucosal cyst. She had diffuse tenderness over her back, which was more significant over the lower thoracic vertebrae. Laboratory data showed a WBC count of 18,000, with neutrophilic predominance of 91.4%. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level were 120mm/hour and 207.5mg/L respectively. Magnetic resonance imaging (MRI) of the thoracic spine (Fig. 1A and B) was performed, which revealed an abscess on the posterior aspect of the spinal cord displacing the spinal cord anteriorly at the level of T5 and T6. Another abscess anterior to the spinal cord, which was displacing the spinal cord posteriorly at the level of T6 and T7 extending to T8, was also observed. There was signal abnormality of the bodies of T6 and T7 vertebrae consistent with osteomyelitis. The patient was started empirically on intravenous vancomycin and doripenem, with pending blood cultures. Two blood cultures isolated from the patient one hour apart at the time of admission grew Gram-negative rods positive for anaerobic bacteria, P. oralis. The body fluid aspirated from the abscess was also positive for P. oralis. The API® 20A anaerobic system (bioMérieux Inc.) was used in identification of bacteria. Antibiotics were changed to ampicillin-sulbactam and metronidazole after the availability of culture reports. The patient was later transferred to a skilled nursing facility with a long-term intravenous access, and later responded well to the treatment after antibiotic therapy for eight weeks.
DiscussionP. oralis was first described as Bacteroides oralis as a new species isolated from the oral cavity of a man which was distinguished in many ways from Bacteoirdes fragilis by Loesche et al.3 It was later reclassified and the new genus Prevotella was suggested by Shah and Collins.2 In most studies of osteomyelitis caused by anaerobic bacteria, the common implicated organisms are Bacteroides spp., Fusobacterium spp., and Clostridium spp. On review of the PubMed database, with the search words ‘Prevotella and osteomyelitis’, ‘Prevotella and vertebral’, and ‘Prevotella and spondylodiscitis’, eight cases of human vertebral osteomyelitis were retrieved that were caused by different species of Prevotella; however, none of them was caused by P. oralis.4–11 Clinical characteristics of these patients are summarized in Table 1.
Clinical characteristics of the patients with vertebral osteomyelitis caused by Prevotella spp. previously described in the literature.
| Authors | Patient characteristics | |||||
|---|---|---|---|---|---|---|
| Age | Gender | Prevotella species | Site of osteomyelitis | Risk factors | Treatment outcome | |
| Surbled et al.4 | 44 | M | P. melaninogenica | L5-S1 | None | Favorable |
| Salavert et al.5 | 27 | F | P. melaninogenica | L2-L3 | IV drug use | Favorable |
| Fukuoka et al.6 | 60 | M | P. intermedia | T7-T8 | Age | Favorable |
| Schöber et al.7 | 45 | F | P. intermedia | L1-L2 | None | Favorable |
| Mukhopadhyay et al.8 | 35 | F | P. melaninogenica | S1 | Dental cleaning | Favorable |
| Salliot et al.9 | 62 | M | Prevotella spp. (the species could not be identified) | L5-S1 | Age, steroids, spodyloarthropathy | Favorable |
| Purushothaman et al.10 | 74 | F | Prevotella spp. (the species could not be identified) | L3-L4 | Age, ovarian malignancy | Favorable |
| Huang et al.11 | 73 | F | P. melaninogenica | T12-L3 | Age, diabetes | Patient died |
P. oralis as an isolated microbiologic agent in vertebral osteomyelitis is an unknown entity. P. oralis is a major commensal on the mucosal surfaces of the body such as the oral cavity, gastrointestinal tract, and vagina. Previously, it has been reported to cause periodontal infections, urinary tract infections, and rarely intra-abdominal abscesses. The source of sepsis in this patient could have been the breech in mucocutaneous barrier during the EGD, which displaced the oral flora into the blood stream. The possibility of necrosis associated with the submucosal cyst could also be implicated in the septicemia caused by P. oralis, which ultimately led to seeding of the organism in the bones and subsequent development of osteomyelitis. The present case highlights the importance of therapy directed against anaerobic pathogens in appropriate clinical settings.
Conflict of interestAll authors declare to have no conflict of interest.
The authors sincerely thank Monica Chiang, MD, for translation of reference No. 5 from Spanish to English.