Human immunodeficiency virus (HIV) positive patients may develop vasculitis, either mediated by immunological factors or by direct vascular injury. We describe a patient who developed manifestations suggestive of extremities vasculitis with no identifiable risk factors other than HIV, Epstein Barr and Herpes Simplex Virus (HSV) type 1 co-infection. Physicians should be aware that vasculitis may have a heterogeneous presentation and occur associated with HIV infection. Although unusual, this association should be recognized for early proper treatment and prevention of ischemia.
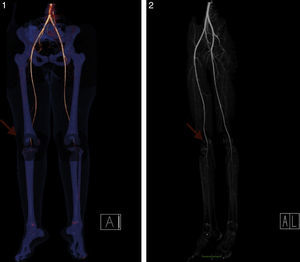
A 30-year-old black female was referred from a primary center with a history of a 2-week intermittent claudication with paresthesias and hypothermia in extremities, most intense in the lower limbs. She was a non-smoker HIV-infected patient on irregular highly active antiretroviral therapy (HAART) with efavirenz, emitricitabine and tenofovir. She denied fever, diabetes mellitus and prior peripheral vascular disease. Examination revealed dehydration, temperature 36.7°C, respiratory rate 20/min, pulse rate 50/min, and immeasurable BP in all four limbs. Brachial, radial and femoral pulses were symmetrical with decreased amplitude. Popliteal, tibial and dorsalis pulses were not palpable bilaterally. The extremities were pale, cold and cyanotic with capillary filling time of 6s. Remaining exam without changes. Initial investigations revealed CD4T lymphocytes 460cells/mL, normal sedimentation rate, C reactive protein, and lipid profile; absence of leukocytosis and thrombocytopenia. Positive Epstein Barr and HSV type 1 IgG antibodies. Venereal disease research laboratory, serology for hepatitis B and C, cytomegalovirus, HSV type 2, antinuclear antibodies, anticytoplasmic antibodies, anticardiolipin antibodies, and antineutrophil cytoplasmic antibodies were negative. ECG, chest X-ray, Doppler echocardiogram, and abdominal-pelvic ultrasound were normal. CT angiography revealed normal aorta, iliac, femoral, and popliteal arteries with no atherosclerotic plaques; bilateral and symmetrical absence of vascular lumen opacification distally to popliteal trifurcations; absence of thrombi, areas of stenosis or atherosclerotic calcification. The evidence of impaired peripheral perfusion, in the absence of atherosclerotic/thrombotic lesions and drug use (besides those included on HAART) led us to assume the diagnosis of vasculitis of medium and small vessels of the extremities in the context of HIV, Epstein Barr, and HSV type 1 co-infection. The patient was treated with HAART, steroids, vasodilators, and anti-platelet aggregation agents. Eight months after discharge and on regular HAART, the viral load was undetectable, CD4T lymphocytes 536cells/μL, and the patient was asymptomatic (Figs. 1 and 2).
DiscussionThis report describes the occurrence of a suspected vasculitis of the extremities in a patient with HIV infection and positive IgG antibodies for Epstein–Barr virus and HSV type 1. The remarkable feature in the patient's presentation was the occurrence of the described events in the context HIV infection without severe immunosuppression (CD4 <200cells/mL). Vasculitis is characterized by injury of the blood vessels that induces vascular lumens reduction and tissular ischemia. There is great heterogeneity in clinical presentation and its pathogenesis is not fully understood.1 In the reported patient the signs of poor peripheral perfusion discordant with the neurological status and cardiac function suggested the diagnosis of vasculitis. HIV-related vasculitis has been described by several authors, has an occurrence estimated at 1% and is therefore considered rare.2–6 It may be caused by direct vascular injury or be mediated by immunological factors.2–5 It especially occurs in severe immunosuppressed cases, with CD4T lymphocytes below 200cells/mL, in the context of opportunistic infections or in the absence of identifiable agents.2,3,7 According to the literature, when the immune system is compromised, even ubiquitous agents such as Epstein Barr Virus and HSV can cause vasculitis.5,6 Some predisposing factors, which may be an independent cause of vasculitis are tuberculosis, parasitic and autoimmune diseases; however, the patient had neither manifestations of these diseases nor laboratory evidence. Another confounding factor was the patient's normal inflammatory markers, which delayed the diagnosis of vasculitis until admission to the ward. Interestingly, a study by Borg and Dasgupta reported normal inflammatory markers in 30% of patients with vasculitis later revealed by imaging techniques.8 Some imaging findings may suggest the diagnosis: on ultrasound, hypoechoic areas along the arterial wall also described as pearl necklace; on angiography, increased vascular wall thickness and reduced vascular lumen opacity.8,9 The gold-standard for the diagnosis of vasculitis is the histopathological study. Unfortunately, we were not able to perform it because the patient did not consent. It would contribute to a better understanding of the subclinical vascular abnormalities and their etiology. We should also point out that this is a limitation of our report. Treatment is HAART, plasma exchanges, and corticosteroids. Vasculopathy in the context of HIV-infected patients on HAART may be caused by drug-related toxicity. Although HAART has changed the pattern of HIV infection and the course of AIDS, it may cause adverse reactions such as endothelial dysfunction, vasculitis, and coagulation disorders leading to thromboembolism, systemic arterial hypertension, coronary artery disease, and peripheral vascular disease. There is evidence that some HAART regimens, such as those including zidovudine, efavirenz and protease inhibitors, interrupt endothelial cell junctions and cytoskeleton action of the endothelial cells leading to endothelial dysfunction.8 Drug induced hypersensitivity vasculitis typically involves small vessels and its pathologic mechanisms include T-cell recognition of proteins or deposition of immune complexes in blood-vessel walls. Hypersensitivity reactions should be considered as a possible etiology of vasculitis in HIV-infected patients on HAART. It is plausible to consider that in this report, vasculitis could have been associated with drug related toxicity given that the patient referred multiple interruptions of an efavirenz, emitricitabine and tenofovir based HAART. However, against this hypothesis, the patient remained on the same previously used HAART regimen with no interruptions and the vasculitis regressed. According to Lo and Plutzky,9 HIV drug treatment interruptions have also been associated with increased cardiovascular event rates. Data from the Strategies for Management of Anti-Retroviral Therapy (SMART) trial suggest that activation of inflammatory and coagulation pathways induced by HIV infection may be further worsened by treatment interruption and thus further increase the risk of death among HIV infected patients.9 According to Guillevin, HIV-related vasculitis do not appear to recur.10 In conclusion, physicians should be aware that vasculitis may have a heterogeneous presentation and can occur in association to HIV infection. Although unusual, this association should be recognized for proper early treatment and prevention of extremity ischemia.
Conflicts of interestThe authors declare no conflicts of interest.
Ethical approvalThe ethical approval and informed consent of the patient for publication of the case were obtained.
To the Study Gabinet of Girassol Clinic.