Adherence, which is crucial to the success of antiretroviral therapy (HAART), is currently a major challenge in the care of children and adolescents living with HIV/AIDS.
ObjectiveTo evaluate the prevalence of nonadherence to HAART using complementary instruments in a cohort of children and adolescents with HIV/AIDS followed in a reference service in Campinas, Brazil.
MethodsThe level of adherence of 108 patients and caregivers was evaluated by an adapted standardized questionnaire and pharmacy dispensing records (PDR). Non-adherence was defined as a drug intake lower than 95% (on 24-hour or seven-day questionnaires), or as an interval of 38 days or more for pharmacy refills. The association between adherence and clinical, immunological, virological, and psychosocial characteristics was assessed by multivariate analysis.
ResultsNon-adherence prevalence varied from 11.1% (non-adherent in three instruments), 15.8% (24-hour self-report), 27.8% (seven-day self-report), 45.4% (PDR), and 56.3% (at least one of the outcomes). 24-hour and seven-day self-reports, when compared to PDR, showed low sensitivity (29% and 43%, respectively) but high specificity (95% and 85%, respectively). In multivariate analysis, medication intolerance, difficulty of administration by caregiver, HAART intake by the patient, lower socioeconomical class, lack of virological control, missed appointments in the past six months, and lack of religious practice by caregiver were significantly associated with non-adherence.
ConclusionA high prevalence of HAART non-adherence was observed in the study population, and PDR was the most sensitive of the tested instruments. The instruments employed were complementary in the identification of non-adherence.
Upon the beginning of the fourth decade of the acquired immunodeficiency syndrome (AIDS) pandemic, the proportion of children and families affected by human immunodeficiency virus (HIV) infection remains an increasingly important global public health problem. It is estimated that there are more than 33 million people living with the disease across the world.1 In Brazil every year, around 35,000 new cases are reported, with an estimate of 635,000 people (0.33% of the general population) living with HIV.2 Since the beginning of the epidemic, around 18,000 AIDS cases were reported in Brazilian children younger than 13 years old, approximately 95% of which were vertically acquired. Around 16,600 children born to HIV-infected mothers were yearly reported, and 815 new pediatric cases were reported in 2010 alone, for a vertical transmission rate of 4.9%. Such a rate is higher than the targeted goal, since a national protocol for prevention of vertical transmission began to be implemented in 1999.3,4
The introduction of highly active antiretroviral therapy (HAART) led to a significant reduction in mortality and increase in the quality of life of people affected by the disease.4,5 According to data from the World Health Organization, more than five million people are now receiving treatment, but this is estimated to be only 35% of people who need therapy.6 In Brazil, as a part of a public health policy coordinated by the Department of Sexually Transmitted Diseases, AIDS, and Viral Hepatitis of the Ministry of Health, access to antiretroviral therapy is universal and free of charge, currently benefiting around 200,000 patients.7
In the current scenario, a major challenge faced by health services is to ensure proper adherence to therapy, indispensable for adequate control of the disease. Studies show that children and adolescents comprise a group with increased vulnerability in adherence to treatment, who require effective monitoring to maintain the sustainability of a lifelong therapy.8,9 Inappropriate adherence to antiretroviral therapy causes serious consequences to people living with HIV/AIDS, with increased risk of viral resistance, immune deterioration, opportunistic infections and death, since the aims of the treatment are the control of virus replication, and preservation or recovery of immunocompetence.10,11
Several studies analyzing the factors associated with non-adherence, using different assessment methods, individually or in association, are found in the literature. In most of the reports adherence of patients or caregivers was ascertained by means of response to questionnaires, either by self-report or by interviews led by health professionals.12–16 Other resources include data from pharmacy dispensing records (PDR);17,18 electronic drug monitoring (EDM);19–21 subjective assessment by health professionals;22 counting of pills returned by patients, in the patient's home or by telephone;23,24 and serum drug level determination.25 Overall, the results from the above studies demonstrate a high degree of heterogeneity in adherence outcomes, suggesting the potential usefulness of complementary approaches.
The objective of this study was to assess adherence to HAART and the factors associated with non-adherence, using complementary methods, in a population of HIV-infected Brazilian children and adolescents attending a reference center.
Materials and methodsAn observational, cross-sectional study was performed at the Pediatric Immunodeficiency Clinic at the Hospital da Universidade Estadual de Campinas, which is responsible for the care of HIV-infected children and adolescents from the metropolitan area of the city of Campinas, state of São Paulo, Brazil. All 129 children and adolescents followed at this reference center, aged 7 to 19 years-old, were initially selected to participate in the study. Patients with mental retardation, implying cognitive impairment and neurological diseases, which hindered the understanding of the issues proposed, were excluded. A total of 108 patients (60 males) were evaluated during the period from November, 2008, to December, 2009.
Adherence was assessed using an adapted standardized questionnaire,26 and by PDR for antiretrovirals, using data from the Logistic Antiretroviral Medicines Control System (Sistema de Controle Logístico de Medicamentos–SICLOM), a centralized pharmacy dispensing system with nationwide coverage. Interviewed patients and/or their caregivers were asked about the administration of prescribed medication in the last 24hours and also in the last seven days. The questionnaire format provided a result in terms of percent of adherence, from 0% to 100%. Patients were considered non-adherent if, in response to the questionnaire, they reported receiving less than 95% of prescribed doses in the previous 24hours or seven days. The cutoff value of 95% was chosen due to its association with the effective control of viral replication and prevention of resistance to HAART.27 In the analysis of SICLOM records, patients were considered non-adherent if an interval of 38 days or more had elapsed from the last refill of antiretrovirals, according to recommendations issued by the Brazilian Ministry of Health.28 Due to the characteristic of the SICLOM records, which are independent both from the patient's report and the examiner's records, PDR data were used as standards for the evaluation of the accuracy of 24-hour and seven-day questionnaire data. Sensitivity, specificity, and positive and negative predictive values were thus calculated for 24-hour and seven-day questionnaire outcomes.
Data were also collected on the following independent variables, related to demographical, social, clinical, immunological and virological conditions: gender, age, socioeconomic status,29 patient and caregiver schooling, caregiver employment status, family income, knowledge of the diagnosis by the patient, HIV caregiver status, HAART use by caregiver, illicit drug use by caregiver, quality of life scores (using the PedsQL 4.0™ inventory),30 orphaned state of patient, adoptive caregivers, missed clinic appointments, religious practice by patient or caregiver, difficulties in the administration of medicines, person in charge for administering medicines, medication intolerance, clinical and immunological classification,31 HAART complexity, number of previous antiretroviral regimens, protease inhibitor usage, recent HIV viral load and lymphocyte subpopulation counts, and HIV resistance.
All interviews were conducted by the first author of the study, in a designated room, for approximately 30minutes.
All patients and/or caregivers were informed of the details of the study, and those, or their legal representatives, who agreed to participate were asked to sign an informed consent. The study was approved by the local Committee of Ethics in Research (statement 711/2008).
Study data were stored and analyzed with the Statistical Package for the Social Sciences (SPSS) for Windows, version 16.0 (SPSS Inc., Chicago–IL, USA). Risk was assessed by calculation of odds ratios (OR) and 95% confidence intervals. Raw OR values were determined by univariate logistic regression, by the “Enter” method. Adjusted OR and 95% confidence intervals were obtained by multivariate logistic regression, “forward Wald” method, with inclusion p-values of 0.05 and exclusion p-values of 0.10.
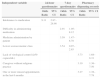
ResultsA total of 108 patient-caregiver dyads were interviewed. The main clinical and demographic characteristics of the study population are shown in Table 1.
Clinical and demographic characteristics of 108 study subjects.
| Variable | Values |
|---|---|
| Male gender* | 60 (55.5%) |
| Age in years† | 13.22 (7.9–19.6) |
| Socioeconomic level* | |
| A+B | 25 (23.1%) |
| C+D | 83 (76.9%) |
| Caregiver education level* | |
| High School or higher | 30 (27.8%) |
| Elementary School or lower | 78 (72.2%) |
| Patient education level* | |
| High School or higher | 24 (22.2%) |
| Elementary School or lower | 84 (77.8%) |
| Monthly per capita income (US dollars)† | 185.18 (11.1–1.296.27) |
| Knowledge of diagnosis by patient* | 65 (60.2%) |
| HIV-infected primary caregiver* | 57 (52.8%) |
| Use of HAART by caregiver* | 52 (48.1%) |
| Employed caregiver* | 52 (48.1%) |
| Illicit drug use by the caregiver* | 1 (0.9%) |
| PedsQL 4.0 score - caregiver† | 85.8 (9.78–98.9) |
| PedsQL 4.0 score - patient† | 84.7 (34.7–100) |
| Orphanhood in relation to at least one biological parent* | 61 (56.5%) |
| Foster or institutional caregiver* | 44 (40.7%) |
| One or more missed appointments in the last 6 months* | 32 (29.6%) |
| Practice of religion by the caregiver | 60 (55.6%) |
| Practice of religion by the patient* | 59 (54.6%) |
| Difficulty in drug administration by caregiver* | 19 (17.6%) |
| HAART administered by caregiver* | 76 (70.4%) |
| CDC clinical classification* | |
| N, A or B | 77 (71.3%) |
| C | 31 (28.7%) |
| Therapeutic regimen* | |
| Low complexity (less than 4 ARVs) | 72 (66.7%) |
| High complexity (4 or more ARVs) | 36 (33.3%) |
| Number of prior ART regimens* | |
| Four or more | 59 (54.6%) |
| Less than 4 | 49 (45.4%) |
| Use of a protease inhibitor* | 66 (61.1%) |
| Intolerance to medication* | 19 (17.6%) |
| CD4+lymphocyte count<500/mm3* | 24 (22.2%) |
| CD4/CD8 ratio≥1* | 22 (20.4%) |
| Controlled viral replication (<50copies/mL)* | 54 (50%) |
| Resistance to ARVs (34 subjects)† | |
| Classes | 3 (0–4) |
| NRTI | 5 (0–6) |
| NNRTI | 2 (0–2) |
| PI | 3 (0–8) |
| Total ARV | 10 (0–16) |
*proportions; †median and extreme; CDC, Centers for Disease Control and Prevention/Ministry of Health; HAART, highly active antiretroviral therapy; NRTI, reverse transcriptase inhibitors, nucleoside analog; NNRTI, reverse transcriptase inhibitors, non-nucleoside; IP, protease inhibitor.
The prevalence of non-adherence varied from 15.8% (24-hour questionnaire), and 27.8% (seven-day questionnaire) to 45.4%, according to PDR. A total of 11.1% of patients were considered non-adherent in all three instruments, and 54.6% were considered non-adherent in at least one of them. Statistically significant non-adherence risk factors for complementary instruments after multivariate analysis were: difficulty of medicine administration by the caregiver, delegation of responsibility of medicine administration to the child or adolescent patient, lower socioeconomic class, lack of virological control, lack of religious practice by the caregiver, missed clinic appointments, and medication intolerance (Table 2).
Comparison of complementary adherence outcomes after multivariate analysis.
| Independent variable | 24-hour questionnaire | 7-day questionnaire | Pharmacy dispensing records | |||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Intolerance to medication | 9.11 | 2.87–28.98 | ||||
| Difficulty in administering medication | 2.91 | 1.05–8.12 | ||||
| Medicine administration by patient | 3.59 | 1.47–8.78 | ||||
| Lower socioeconomic class | 3.54 | 0.97–2.85 | ||||
| Lack of virological control (≥50 copies/mL) | 3.73 | 1.68–8.31 | ||||
| Caregiver without religious practice | 3.19 | 1.36–7.50 | ||||
| One or more missed appointments in the last 6 months | 3.27 | 1.38–7.78 | ||||
In relation to PDR, data from 24-hour and seven-day questionnaires showed low sensitivity, but good specificity and positive predictive values (Table 3).
DiscussionIn the population studied, the evaluation of PDR proved to be an instrument capable of detecting a higher prevalence of failure to adhere to ART (45.4%), when compared to standardized questionnaires (15.8% for 24-hour recall and 27.8% for seven-day recall). The lowest prevalence of non-adherence was observed when considering the three simultaneous instruments (11.1%), and the highest prevalence (56.3%) when individuals were considered non-adherent by at least one of the instruments. To the authors’ knowledge, this is the first study to make such comparison in Latin America. Several pediatric studies have shown, similarly, the usefulness of PDR analysis as an indicator of adherence with ART, highlighting its direct association with control of viral replication, in both developed and developing countries.15,20,32–34
The usefulness of PDR analysis was also emphasized by Grossberg et al.17 in a study with adults in the U.S., which observed a higher sensitivity and better association with the virologic response of PDR, when compared to self-report. Bisson et al.,35 and Rougemont et al.,36 also with adults, observed PDR to be more sensitive than the CD4+ T-lymphocyte count as a predictor of virologic failure. In contrast, Acri et al.,21 reported low correlation between EDM and PDR in a study in adults. However, the authors pointed out that the PDR data in that report were obtained retrospectively from commercial pharmacies, rather than from a centralized PDR, which was the case in the present study.
In a recent review, Bangsberg37 highlighted the practicality of using PDR, with the advantage of not relying on expensive devices, and also, in relation to self-report, of its independence from patient cooperation. The characteristics of such pharmacy registry in the health services of hospitals of the present study, with universal distribution of antiretrovirals and centralized dispensation with physical proximity to the outpatient service, plus the 30-day provision limits and computerized control, make this quite simple procedure a practical and feasible instrument for adherence control. Due to these characteristics, PDR monitoring has been recommended by the Ministry of Health.31
The 45.4% non-adherence rate detected in the present study by PDR appears to be higher than usually reported. Systematic reviews of international pediatric studies related variability in the prevalence of adherence between 49% and 100%, with 76% of studies reporting adherence above 75%, with a trend towards greater adherence in developing countries.32,34 These contrasting results are probably mainly due to the usually higher sensitivity of PDR, when compared to the most commonly used self-report or interview methods.37
In order to identify not only the prevalence of adherence failure, but also the associated risk factors, providing a foundation for successful interventions, there is a tendency in the literature to recommend the combination of methods, as used in this study. The results of several studies with different scenarios reinforce these recommendations.23,38 Noteworthy are the data obtained by Llabre et al.39 that, in a longitudinal study, used different methods for measuring adherence (self-report, interviews and EDM), on multiple occasions. Consistently, the use of at least two methods was significantly associated with control of viral replication.
Among the independent variables analyzed in the present study, multivariate analysis found seven risk factors for non-adherence: difficulty of medicine administration by the caregiver, delegation of responsibility of medicine administration to the child or adolescent patient, lower socioeconomic class, lack of virological control, lack of religious practice by the caregiver, missed clinic appointments, and medication intolerance.
The difficulty of administration of medication was reported as a non-adherence risk factor, associated with higher viral loads, by Allison et al.,40 in a study with caregiver interviews. In contrast with the present study, Biadgilign et al.41 reported that 97.4% of participants had positive attitudes regarding the administration of antiretroviral drugs, despite 22.3% reporting particular difficulties, such as children spitting the medication, resistance and refusal, and the need for simultaneous administration of several drugs.
Although this analysis reveals the delegation of responsibility of administration of ART to pediatric patients as a risk factor for adherence failure, no other reports in the literature that have directly addressed this important association were found. An analogous situation, however, is reported by Williams et al.,42 who identified improved adherence in situations of care provided by caregivers without a biological connection, or in cases of social support systems aimed at helping adolescents to remember the timing of medication doses. In the authors’ interpretation, delegating to adolescents their own care in situations of chronic disease, without close supervision, may constitute an excessive responsibility burden.
An association between lower socioeconomic class and risk of non-adherence was observed. Similar findings were also reported by Cupsa et al.,43 in a pediatric adherence study in Romania. In the authors’ view, lower family income may act as a social stress feature, with potential harmful consequences to a succesful therapy.
The group of patients whose caregivers reported regular religious practice showed a significantly lower prevalence of non-adherence. These results are consistent with those observed by Park and Nachman,44 who analyzed the patterns of adherence to ART in relation to religious beliefs in an adolescent HIV-infected population. Individuals with excellent adherence had significantly higher scores of religious beliefs than those who had low adherence. No specific data about caregivers was found in the literature, but it is possible that religious practice provides stronger community support, which may be helpful in the setting of a chronic disease.
The association of missed appointments with adherence failure is straightforward. Absentees are at greater risk of failing to follow the treatment properly. Vreeman et al.32 reported that more than half of the children have lost at least a monthly consultation, but these authors did not approach the association with treatment adherence.
Intolerance to antiretrovirals was significantly associated with lower adherence, according to the evaluation measures in the 24hours preceding the interview. A qualitative analysis in order to obtain a deeper understanding of the factors that influence adherence to antiretroviral therapy in a pediatric population in Southern India described factors related to the drugs that influence adherence, showing comparable results. The difficulty of adherence was associated with side effects, size and arrangements of the tablets, and flavor and taste of pediatric formulations.45
Viral load, as a frequent clinical analysis procedure, of utmost importance in its relationship to a successful treatment, appears as an important adherence factor in most studies related to ART. The present study revealed a significant direct association between virological control and adherence to treatment, as measured by pharmacy data. Similar results were presented by several other reports.15,17,20,24,25,33,40,42
The main limitation of this study is its cross-sectional design, causing susceptibility to confounding factors. Also, none of the adherence instruments used is flawless. The use of questionnaires in interviews involves subjective factors such as memory difficulties and embarrassment of the patient or caregiver, who may fear the judgment on the part of the health professional.46 PDR, which is considered to be a preferred instrument, is also susceptible to errors. It is not possible to prove whether the dispensed drug was effectively ingested, at the right schedule, and that it reached therapeutic levels. There is a risk of overestimating adherence failures, especially in short-term approaches in the case of patients who have small stocks of medicines at home. The authors believe, however, that most of these deficiencies are overcome in this country, by the centralization of dispensing and the computerized control of refills.
ConclusionsIn the population studied there was a high prevalence of failure of adherence to ART, with higher detection sensitivity when using pharmacy dispensation records. The instruments used were complementary in identifying risk factors for non-adherence.
Adherence failure can result in catastrophic consequences for the patient and the community, potentially resulting in higher morbidity and even death. In a scenario of universal access to treatment, as in Brazil, a public health initiative whose merit is internationally recognized, such an outcome should not be accepted. These facts highlight the importance of encouraging health services to adopt a proactive stance to prevent uncontrolled viral replication, assuring better survival and quality of life for patients who need a lifelong course of therapy. To achieve this goal, the risk factors associated with non-adherence, as identified in this study, should be routinely considered during the follow-up of patients and their caregivers in order to plan specific interventions. Due to its sensitivity and feasibility, adherence assessment by PDR should be included in the routine preparation of patient visits.
Conflict of interestAll authors declare to have no conflict of interest.
This study was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), scholarship No. 2009/06948-0, and by the Fundo de Apoio ao Ensino, Pesquisa e Extensão (FAEPEX) UNICAMP, grant No. 0449/08.