Since numerous tropical pathogens lead to opportunistic infections in the context of the human immunodeficiency virus (HIV), coinfection could have significant effects on the course of HIV infection.1
In this article we report two cases coinfected with HIV and Trypanosoma cruzi presenting unfavorable evolution despite correct treatment. Both patients were infected with both pathogens by mother-to-child transmission (MTCT) route, and both died due to a Klebsiella pneumoniae sepsis.
Case 1: Child 1 was admitted to the Central Children's Hospital in La Plata at age 1 month with respiratory difficulty and diarrhea. The patient was a preterm newborn with good weight for the gestational age, with no prenatal care. Both parents were illiterate, and were living with HIV for a year but without treatment, including during pregnancy. The father was an intravenous drug abuser, and had been incarcerated; a 2- year-old brother was HIV-negative but an elder sister had died of HIV/acquired immunodeficiency syndrome (AIDS). Chagas infection in the mother was probably congenital, since her mother emigrated from a high endemic zone. The child presented severe malnutrition and congenital heart disease (interventricular communication).
The child started with shortness of breath and diarrhea with a 48-hour evolution, and also presented bilateral inguinal and cervical micropoliadenopaty, splenomegaly, thrush, hypoxemia, and opisthotonus position. Disturbances in the cerebrospinal fluid cell count became apparent and Streptococcus pneumoniae was cultivated. Therefore, the patient was received ceftriaxone at appropriate doses for meningitis treatment for ten days, and an erythrocyte transfusion was performed. Vaccination with DPT-HB-Hib and Salk was indicated. During hospitalization, he presented two episodes of seizures related with fever. Serologies for several pathogens were performed, and antibodies for T. cruzi, Toxoplasma gondii, Epstein-Barr virus (EBV), and HIV were detected. HIV infection was confirmed by polymerase chain reaction (PCR), and T. cruzi infection, by Microstrout (both infections were confirmed in at least two separate samples). Electroencephalography (EEG) and cerebral computed tomography (CT) were abnormal, with muscular hypertonia and opisthostonus, both bilateral clonus and positive Babinsky. The symptoms were interpreted as brain damage due to pneumococcocal meningoencephalitis.
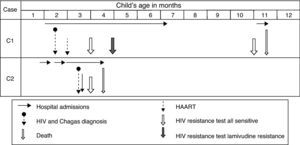
At the age of six months, he was released after 155 days in hospital. Then, at the age of 22 months, he presented with diarrhea and sepsis by K. pneumoniae with secondary dehydration. The patient died ten days later; he had been treated with zidovudine since delivery and for two months with combined HAART (lamivudine, stavudine, nelfinavir) and benzonidazol. Three resistance tests were performed: two of them showed full sensitivity, while the second test showed lamivudine resistance (Fig. 1).
Case 2: Child 2 was admitted twice at a provincial hospital presenting fever with pneumonia, thrush, and anaemia, and was later referred to the Central Children's Hospital. The patient had been born by normal vaginal delivery, without complications, after a full-term gestation. His mother, aged 33, from Paraguay, had received prenatal care; her serology was positive for both HIV and for Chagas disease. His father was also HIV-infected. The mother was treated with lamivudine and nevirapine from the age of 17 and received zidovudine late in her pregnancy. In the last admission, the child had an unfavorable evolution with hepatitis and progressive liver failure. Serologies were positive for T. cruzi, cytomegalovirus (CMV), and HIV. HIV infection was confirmed by PCR, and T. cruzi infection, by Microstrout (both infections were confirmed in at least two separate samples). Treatment with zidovudine, nevirapine, and lamivudine was started.
The child received zidovudine for the first six weeks and was treated with interrupted HAART after three months due to severe organic failure. After 39 days at the ICU, the child died with sepsis by K. pneumoniae.
Data from HIV and T. cruzi coinfected patients indicated reactivation of the parasite infection with exacerbation of clinical signs and unusual clinical manifestations,2 as well as MTCT with severe outcome for the child.3–5 In the two presented cases, there was a clear loss of opportunities for prevention of HIV MTCT. Despite the provision of treatment and free follow-up provided by the government, effective antiretroviral (ARV) treatment did not reach these two mothers. In Case 1, this was probably due to the social status of the parents, who did not receive any ARV treatment; in Case 2, ARV treatment might have been insufficient with only ZDV in the last trimester. The oldest sibling of Case 1 may have also died of undiagnosed coinfection. Further, T. cruzi infection was not diagnosed by the physicians working in the provincial hospital in Case 2. This delay in the treatment, initiated only at the Children's Hospital, may have further compromised the course of coinfection.
Conflict of interestAll authors declare to have no conflict of interest.
This research has been partially funded by a Fogarty International Center/NIH grant through the AIDS International Training and Research Program at Mount Sinai School of Medicine -Argentina Program (Grant # 5D43 TW0010137), and grants from the Universidad de Buenos Aires (M043) to Liliana Martínez Peralta. This study was approved by the Independent Ethics Committee, School of Medicine, Universidad de Buenos Aires.