Tuberculosis (TB) is a rare cause of chronic suppurative otitis media and mastoiditis, therefore it is usually not considered in the differential diagnosis of chronic infections of this area, especially when evidence of pulmonary tuberculosis is absent.1 This diagnosis should be considered in patients that do not respond to empirical therapy.
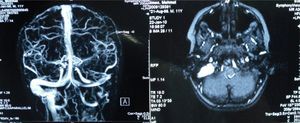
An 11-year-old previously healthy male was admitted to our hospital with swelling in the mastoid area. Left ear discharge and otalgia had started two months prior. Empirical antibiotic therapy had been prescribed by a pediatrician. Symptoms had persisted despite appropriate antibacterial treatment. Temporal MRI revealed inflammatory swelling in the left middle ear and the mastoid air cells (Fig. 1). The patient was treated with surgery, metronidazole, and cefazolin. The pathological specimen showed granulomatous tissue with necrosis and Langhans giant cells. Acid-resistant bacilli was positive in the tissue. The patient's history was reviewed. His grandfather had received treatment for tuberculosis one year prior, thus our patient had taken prophylaxis, but for an inadequate period and improperly. The 48-hour tuberculin test (PPD) measured 21mm (positive), one BCG scar was observed, and the chest X-ray was normal. Acid-resistant bacilli was not found in the gastric aspirate for three days. Antituberculous treatment with three drugs (isoniazide, rifampicin, and pyrazinamide) was started. Cranial MRI venography showed thrombosis in the left sigmoid and jugular vein (Fig. 1). Hematological studies confirmed the diagnosis of prothrombin mutation 20210; the patient was treated with anticoagulant therapy without sequelae.
The diagnosis of extrapulmonary TB depends on the physician suspecting of the possibility of TB in patients at risk, and referring material for mycobacterial culture and pathological examination. The pathogenesis of tuberculous otitis media is likely related to three distinct mechanisms: spread to the middle ear via the Eustachian tube; hematogenous spread from another tuberculous focus; and, rarely, direct implantation through the external auditory canal and a tympanic membrane perforation.2 In our patient, hematogenic transmission appears to be the possible route of infection, because he had been given prophylaxis for TB one year prior, which was insufficient and improperly administered. Abnormal chest radiography consistent with pulmonary tuberculosis associated with tuberculous otitis media occurred in 58% of the 74 chest radiographies available for analysis.3 Concomitant pulmonary tuberculosis should suggest the etiology in a patient with chronic otitis media. Despite the absence of a pulmonary finding, tuberculous otitis media should not be ruled out in the presence of otorrhea.3,4 Our patient's chest X-ray was normal, and he did not show any sign of pulmonary tuberculosis.
Hypercoagulable state, which may be either inherited or acquired, is suggested to induce sinus thrombosis in presence of acute or chronic otitis media and mastoiditis5. In our patient, the Prothrombin 20210 mutation was held accountable for thrombosis in the jugular vein and sigmoid sinuses in the presence of otomastoiditis.
We must consider Mycobacterium tuberculosis as a possible origin of otomastoiditis, especially in patients who do not respond to empirical antibiotherapy; if sinus thrombosis progresses in a patient with otomastoiditis, hypercoagulable state must be investigated.
Conflict of interestAll authors declare to have no conflict of interest.