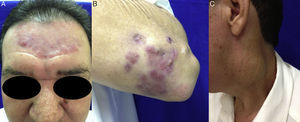
A 50-year-old heterosexual, HIV seronegative, male patient presented at the Dermatology Service with asymptomatic erythematous lesions on his left elbow and forehead for four months. He denied previous treatment, comorbidities and had no systemic symptoms. The dermatological examination showed erythematous purplish tuberous circinate plaque on his forehead (Fig. 1A), reddish purplish tubers, some ulcerated on the left elbow (Fig. 1B), and bulky lymphadenopathy in the neck (Fig. 1C); absence of mucosal lesions; preserved skin sensitivity and peripheral nerves without changes. Test results: VDRL 1/64, TPHA reagent, and anti-HIV nonreactive. The diagnosis of tertiary syphilis was established and treatment with penicillin benzathine 7,200,000IU in three weekly intramuscular doses of 2,400,000IU was administered. Reduction of the lesion was observed one week thereafter and clinical cure was achieved after the end of treatment (Fig. 2).
Syphilis is a millenarian disease but still remains rather prevalent, especially in some high-risk behavior individuals.1,2 In contrast to the increasing incidence of early syphilis (primary and secondary), cases of classic late syphilis (tertiary) as a result of untreated syphilis are rarely seen.3,4 Approximately half of patients with tertiary syphilis presents “benign” late syphilis with gums emergence.4,5 Around a quarter develop cardiovascular manifestations and another quarter develop neurological symptoms.4,6 Gums are locally destructive lesions in the skin, liver, bones, and other organs.4,7 Skin gums are nodular or nodular ulcerative lesions, with an arciform pattern.3,4
Conflicts of interestThe authors declare no conflicts of interest.