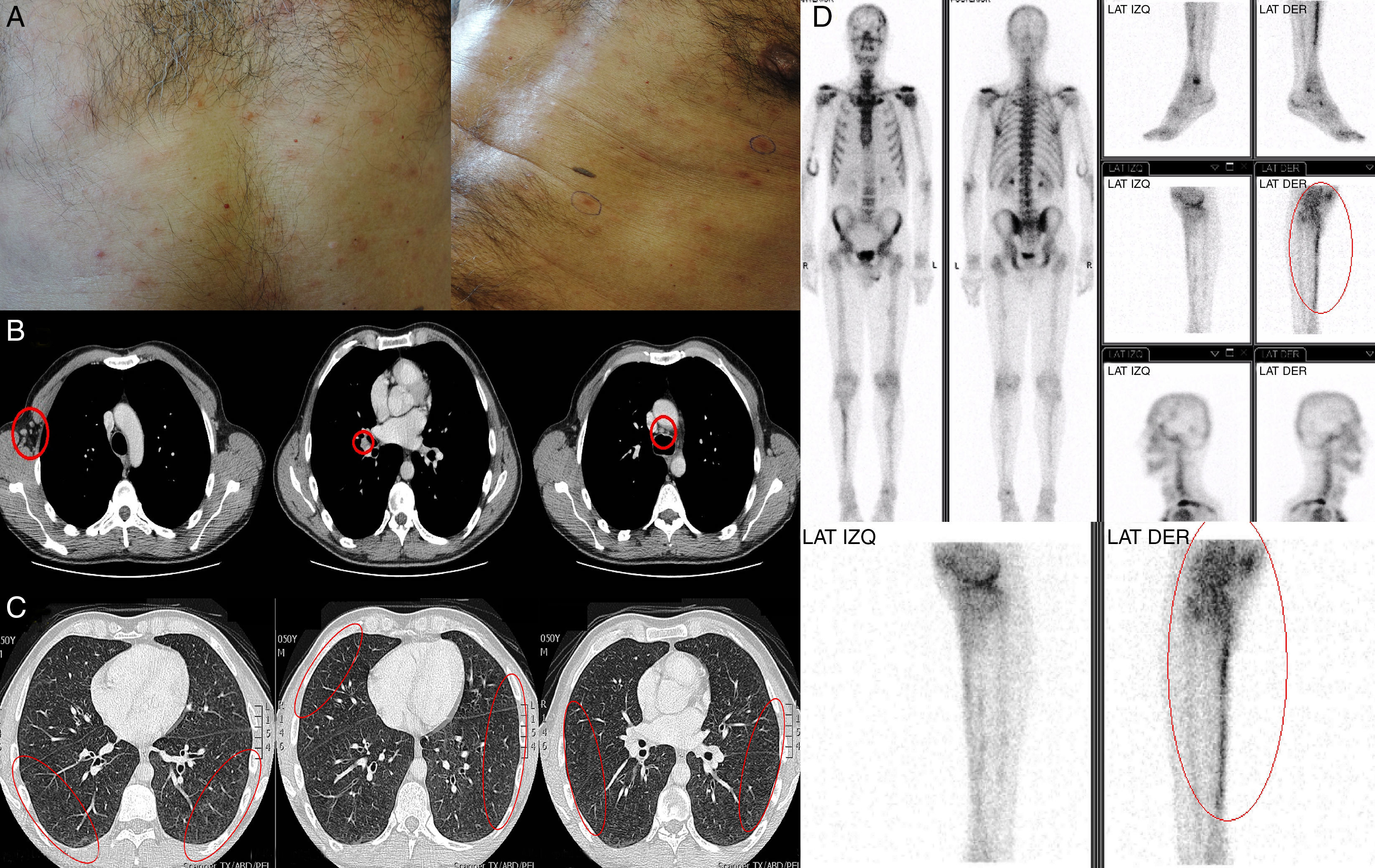
A 50-year-old healthy male was seen for a 6-week history of right leg pain, occasional dyspnea and extensive non-pruritic skin rash in trunk and extremities (Fig. 1A). Physical examination revealed tachypnea with normal breath sounds and a non-confluent maculo-papular rash in the trunk and extremities. No adenopathies, mucosal or palmo-plantar lesions were evident.
(A) Non-confluent maculo-papular rash in the trunk. (B) Contrast-enhanced CT scan showing multiple axillary, hilar and mediastinal lymphadenopathy. (C) Contrast-enhanced CT scan showing bilateral and diffusely distributed pulmonary nodules with ground-glass density. (D) Bone scintigraphy showing increased uptake on the right tibia.
A contrast-enhanced CT scan showed presence of multiple axillary, hilar, and mediastinal lymphadenopathy (Fig. 1B), and bilateral and diffusely distributed pulmonary nodules with ground-glass density (Fig. 1C). Bone scintigraphy showed increased uptake of isotope on the right tibia (Fig. 1D). The Rapid Plasma Reagin test (RPR) was positive in 128 dilutions, with a positive Treponema pallidum microhemagglutination assay. Human immunodeficiency virus and serology of other sexually transmitted diseases were negative. Additional laboratory investigation revealed negative antinuclear antibodies, as well as negative anti-double-stranded DNA, anti-Smith, anti-Ro, anti-La, and anti-neutrophil cytoplasmic antibodies. Complement C3 and C4 levels were within normal ranges. Skin biopsy revealed epidermal orthokeratosis and dermis with perivascular and periadnexal infiltrate composed by lymphocytes, neutrophils and plasma cells. Immunohistochemistry was positive for T. pallidum using monoclonal antibodies.
Considering the above mentioned data a diagnosis of secondary syphilis affecting skin, bone (periostitis), and pulmonary was established. The patient was successfully treated with three-weekly doses of 2.4 million units of intramuscular benzathine-penicillin. Secondary syphilis is characterized by multisystem involvement: skin rash, mucosal lesions, and generalized lymphadenopathy. Simultaneous skin, lung, and skeletal involvement are extremely infrequent, with no cases reported until now.
Conflicts of interestThe authors declare no conflicts of interest.