Fluoroquinolone (FQ)-associated tendinopathy and myopathy are uncommon but well recognized complications of the use of this class of antibacterial agents. The case of a 63-year-old previously asymptomatic female patient who developed severe left shoulder tendinopathy after surreptitiously doubling the prescribed dose of levofloxacin for the treatment of community-acquired pneumonia is reported here. Surgical stabilization with suture anchors and subacromial decompression were needed.
Fluoroquinolone (FQ)-associated tendinopathy, including tendon rupture, myopathy, and arthropathy, is an uncommon but potentially devastating complication of this class of antibacterial agents. It has been described with most representatives of the class, but ofloxacin and ciprofloxacin seem to be the most common agents. Symptoms of tendon injury are reported after a median of eight days of initiation of treatment, but they may appear as early as two hours after the first dose and as late as six months after treatment.1 The first published case report was of a 56-year-old renal transplant patient from New Zealand, in 1983, who developed Achilles tendinopathy after being treated with norfloxacin for urinary tract infection and septicemia.2 The Achilles tendon is the most commonly affected, but any tendon appears to be vulnerable, including tendinitis of extraocular muscles leading to diplopia.3 The case of a female patient who developed severe shoulder tendinopathy after surreptitiously doubling the prescribed dose of a FQ agent for the treatment of community-acquired pneumonia is reported here.
Case presentationA previously asymptomatic 63-year-old female patient from the city of Rio de Janeiro presented with fever, malaise, rigors, and a productive cough of one-week duration. She reported that these signs and symptoms developed soon after returning from a weekend trip to a rural area in the highlands of the state of Rio de Janeiro, where she was exposed to cold weather during outdoor activities. Physical examination showed an acutely ill febrile patient (38.5°C) with coarse crackles on auscultation of the left hemithorax. She was an otherwise healthy elderly patient who reported being physically active through daily regular aerobic and anaerobic activity at a gym. A chest x-ray study showed ill-defined patchy airspace infiltrates in the lingular portion of the left upper lobe, consistent with the diagnosis of acute lower respiratory tract infection. A decision was made to empirically initiate an outpatient treatment with levofloxacin 500mg orally once a day for 10 days.
Two weeks later the patient presented with abrupt onset of diffuse myalgia and severe left shoulder pain. She also complained of pain in the right shoulder, biceps brachii, elbow, bilateral patellar tendon, and hip. Left shoulder swelling and pain on palpation were evident on examination. She informed that the prescribed dose of levofloxacin had been surreptitiously doubled to 500mg bid due to the persistence of fever as of the second treatment day. Laboratory evaluation was remarkable for increased creatine phosphokinase (488U/L; normal value <167U/L). A magnetic resonance imaging (MRI) study of the left shoulder rotator cuff performed one week later showed areas of increased T2 signal intensity on subscapular and supraspinatus tendons and a large gleno-umeral joint effusion with distension of the articular bursa.
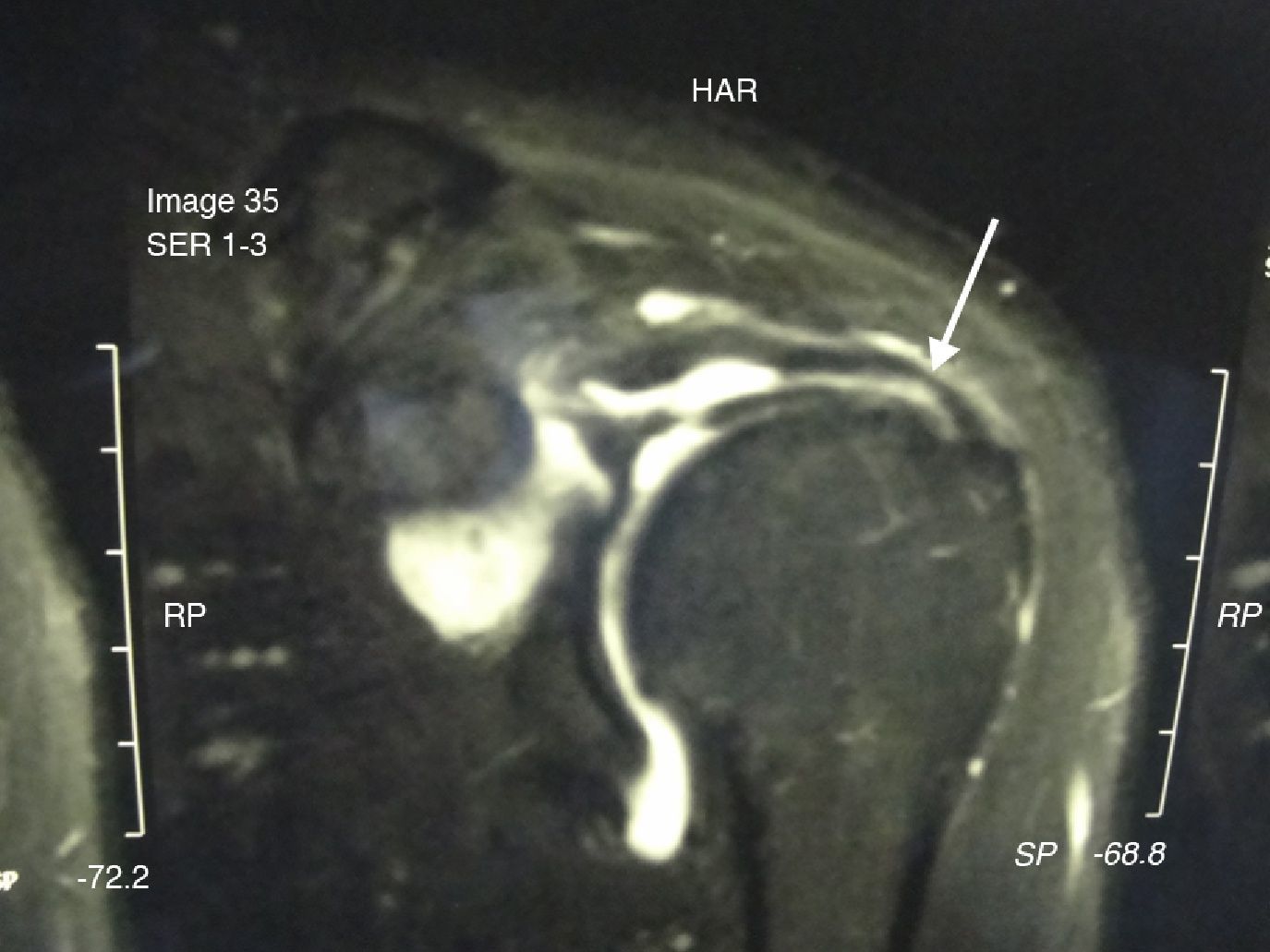
The patient was treated with strict physical rest, nonsteroidal anti-inflammatory agents, shoulder splinting for joint stabilization, and physiotherapy. She gradually improved over the ensuing weeks, except for the left shoulder pain. An MRI study performed three months later showed a partial tear (40%–50% thinning) of the left supraspinatus tendon (Fig. 1). Surgical intervention was then indicated. Arthroscopy exploration revealed a rotator cuff injury with subacromial impingement. Arthroscopic stabilization with suture anchors and subacromial decompression was performed successfully. The patient remains well six months after surgical intervention.
DiscussionIn spite of the FDA warning alert released in August 2008,4 FQ-associated tendinopathy and tendon rupture seem not to be widely known among health care professionals. Proposed pathogenic mechanisms include a direct toxic effect5 and ischemic injury.6 FQ toxicity also includes damage to cartilage, muscle, and bone tissue.7 It has also been associated with acute severe myalgia requiring emergency care treatment.8 In children and pregnant women, the use of FQs is avoided since these agents can cause lesions of articular-epiphyseal cartilage complexes in several species of juvenile animals.9
Major risk factors for FQ-induced tendinopathy include age over 60, concurrent corticosteroid use, high FQ dose, previous musculoskeletal disease, renal failure, and diabetes mellitus. Immediate discontinuation of FQ is warranted, but lack of knowledge on this syndrome has led to inappropriate advice to complete the antibacterial course.10 Van der Linden et al.11 have found that approximately 2% to 6% of all Achilles tendon ruptures in people older than 60 years can be attributed to FQ use. Imaging studies such as ultrasound and MRI are useful in identifying tendon tears.
The present case report highlights the importance of judicious use of FQ agents among those with risk factors for FQ-related tendinopathy, especially older patients. The potential benefits and risks of prescribing a FQ agent should be weighed individually. Patients receiving a FQ agent should be advised to seek medical attention as soon as any sign or symptom of tendinopathy or myopathy develops. The offending drug should be immediately withdrawn and measures of joint rest and expert orthopedic advice instituted. It is also important to avoid corticosteroids since these drugs may worsen the tendinopathy.
Conflict of interestAll authors declare to have no conflict of interest.