The present study evaluated patients with diagnosis of surgical site infection (SSI) following cesarean section and their controls to determinate risk factors and impact of antibiotic prophylaxis on this condition.
MethodsAll cesareans performed from January 2009 to December 2012 were evaluated for SSI, based on criteria established by CDC/NHSN. Control patients were determined after inclusion of case patients. Medical records of case and control patients were reviewed and compared regarding sociodemographic and clinical characteristics.
ResultsOur study demonstrated an association following univariate analysis between post-cesarean SSI and number of internal vaginal examinations, time of membrane rupture, emergency cesarean and improper use of antibiotic prophylaxis. This same situation did not repeat itself in multivariate analysis with adjustment for risk factors, especially with regard to antibiotic prophylaxis, considering the emergency cesarean factor only.
ConclusionThe authors of the present study not only question surgical antimicrobial prophylaxis use based on data presented here and in literature, but suggest that the prophylaxis is perhaps indicated primarily in selected groups of patients undergoing cesarean section. Further research with greater number of patients and evaluated risk factors are fundamental for better understanding of the causes and evolution of surgical site infection after cesarean delivery.
Surgical site infection (SSI) following cesarean delivery is a major cause of morbidity and mortality, increasing both the duration of patient hospitalization and hospital costs.1–4 SSI rates after cesarean range from 3% to 5%, varying according to the population being studied, the methods used to monitor and identify cases, and the use of appropriate antibiotic prophylaxis.5–7
Among the risk factors described for post-cesarean SSI are prolonged labor, premature rupture of membranes, excess vaginal manipulation, manual extraction of the placenta, and premature birth.8–11 Comorbidities such as HIV, severe anemia and gestational diabetes are also associated with higher rates of puerperal infection, particularly surgical wound infection.12,13
The beneficial effect of antibiotic prophylaxis in reducing occurrences of infection associated with elective or emergency cesarean section is already well established.14,15 In many institutions the antibiotic administration is performed after the umbilical cord has been clamped, justified by the neonatal impact of antimicrobial use.15,16 Although antimicrobial prophylaxis reduces the risk of endometritis and incisional SSI when administered correctly, much has been discussed about its real impact due to the small number of studies and their limitations.15,17,18
The present study evaluated patients who underwent a cesarean section and presented with and without SSI after surgery with the aim of determining risk factors and assessing the impact of antibiotic prophylaxis on this condition.
Subjects and methodsThe present manuscript is a retrospective case-control observational study performed at the Hospital Fêmina, a hospital specialized in women's health located in the city of Porto Alegre, Brazil. The department of prevention and infection control of the Hospital Fêmina evaluated all cesarean deliveries performed from January 2009 to December 2012 for SSI (superficial incisional infection, deep incisional infection, and organ/space infection), based on criteria established by the Centers for Disease Control and Prevention's National Healthcare Safety Network (CDC/NHSN).19
The inclusion criteria for enrollment on the study as a case were pregnant patients who underwent cesarean section and having a diagnosis of SSI within 30 days of the obstetric procedure. The routine of the department of prevention and infection control is to evaluate all patients who had cesarean section up till day 30 from the procedure. Control patients were determined after the inclusion of case patients and adhered to the following inclusion criteria: similar age (±2 years), cesarean section, procedure performed on the same day as the case patient, no history of post-cesarean infectious complication up to the 13th day, taking into account the CDC/NHSN criteria.19 Cases were excluded if a control patient meeting the inclusion requirements could not be identified or if patient records were not available.
The medical records of the case and control patients were reviewed with respect to sociodemographic characteristics, elective or emergency cesarean, comorbidities, duration of labor, use of appropriate antibiotic prophylaxis with 2g of intravenous cefazolin, duration of membrane rupture, number of internal vaginal examinations, and length of hospitalization. Appropriate prophylaxis was defined as the antibiotic administered 30–60min before the procedure.20
Statistical analysis was performed using descriptive evaluation with the mean±standard deviation for continuous variables and frequency and percentage for categorical variables. The Student's t-test for independent samples was used for comparing the means between groups and a chi-square test to compare categorical variables. Those variables associated with the outcome in univariate analysis with a significance level below 0.2 were included in a multivariate logistic regression model. The odds ratios between factors and outcomes of their respective 95% confidence intervals were calculated. Also, stepwise backward multiple regression was performed to reveal the best set of predictors of SSI. Microsoft Excel software was used for the data storing and analyses were performed using SPSS for Windows (Statistical Package for Social Sciences), version 18 (IBM, Armonk, NY, USA).
The study was approved by the Research Ethics Committee of the Hospital Conceição Group, Porto Alegre, Brazil, on August 27th, 2012 under registration number 04189412.3.0000.5530.
ResultsA total of 8180 patients underwent cesarean at the Hospital Fêmina over the four-year study period, of which 118 (1.44%) were diagnosed with SSI after cesarean delivery. Ultimately, 79 case patients with an SSI and 79 control patients conforming to the inclusion criteria were identified. Thirty-nine patients (33%) were excluded as control patients could not be matched with them in accordance with the study design. Fifty-six patients (70.9%) of the 79 cases had a superficial incisional SSI, 10 (12.6%) had a deep incisional SSI, and 14 (17.7%) had an organ/space SSI.
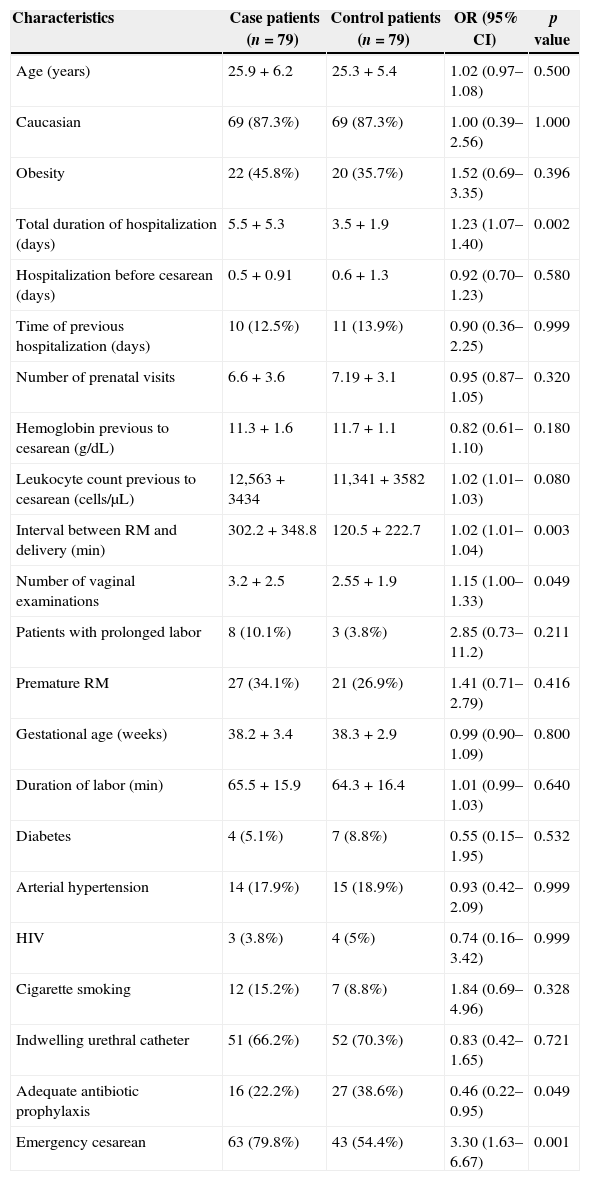
The characteristics of the 79 case patients and 79 control patients are described in Table 1. In addition to the inclusion criteria, the patients from both groups had comparatively similar demographic characteristics, such as age, race, gestational age, body mass index (BMI) and comorbidities. The factors that differentiated case from control patients in the univariate analysis were emergency cesarean, number of internal vaginal examinations, time of membrane rupture, duration of hospitalization, and inappropriate administration of antibiotic prophylaxis (Table 1).
Characteristics of patients undergoing cesarean section in Hospital Fêmina from January 2009 to December 2012.
| Characteristics | Case patients (n=79) | Control patients (n=79) | OR (95% CI) | p value |
|---|---|---|---|---|
| Age (years) | 25.9+6.2 | 25.3+5.4 | 1.02 (0.97–1.08) | 0.500 |
| Caucasian | 69 (87.3%) | 69 (87.3%) | 1.00 (0.39–2.56) | 1.000 |
| Obesity | 22 (45.8%) | 20 (35.7%) | 1.52 (0.69–3.35) | 0.396 |
| Total duration of hospitalization (days) | 5.5+5.3 | 3.5+1.9 | 1.23 (1.07–1.40) | 0.002 |
| Hospitalization before cesarean (days) | 0.5+0.91 | 0.6+1.3 | 0.92 (0.70–1.23) | 0.580 |
| Time of previous hospitalization (days) | 10 (12.5%) | 11 (13.9%) | 0.90 (0.36–2.25) | 0.999 |
| Number of prenatal visits | 6.6+3.6 | 7.19+3.1 | 0.95 (0.87–1.05) | 0.320 |
| Hemoglobin previous to cesarean (g/dL) | 11.3+1.6 | 11.7+1.1 | 0.82 (0.61–1.10) | 0.180 |
| Leukocyte count previous to cesarean (cells/μL) | 12,563+3434 | 11,341+3582 | 1.02 (1.01–1.03) | 0.080 |
| Interval between RM and delivery (min) | 302.2+348.8 | 120.5+222.7 | 1.02 (1.01–1.04) | 0.003 |
| Number of vaginal examinations | 3.2+2.5 | 2.55+1.9 | 1.15 (1.00–1.33) | 0.049 |
| Patients with prolonged labor | 8 (10.1%) | 3 (3.8%) | 2.85 (0.73–11.2) | 0.211 |
| Premature RM | 27 (34.1%) | 21 (26.9%) | 1.41 (0.71–2.79) | 0.416 |
| Gestational age (weeks) | 38.2+3.4 | 38.3+2.9 | 0.99 (0.90–1.09) | 0.800 |
| Duration of labor (min) | 65.5+15.9 | 64.3+16.4 | 1.01 (0.99–1.03) | 0.640 |
| Diabetes | 4 (5.1%) | 7 (8.8%) | 0.55 (0.15–1.95) | 0.532 |
| Arterial hypertension | 14 (17.9%) | 15 (18.9%) | 0.93 (0.42–2.09) | 0.999 |
| HIV | 3 (3.8%) | 4 (5%) | 0.74 (0.16–3.42) | 0.999 |
| Cigarette smoking | 12 (15.2%) | 7 (8.8%) | 1.84 (0.69–4.96) | 0.328 |
| Indwelling urethral catheter | 51 (66.2%) | 52 (70.3%) | 0.83 (0.42–1.65) | 0.721 |
| Adequate antibiotic prophylaxis | 16 (22.2%) | 27 (38.6%) | 0.46 (0.22–0.95) | 0.049 |
| Emergency cesarean | 63 (79.8%) | 43 (54.4%) | 3.30 (1.63–6.67) | 0.001 |
RM, rupture of membranes; min, minutes.
Other factors such as ethnicity, education, number of pregnancies, preeclampsia, and illicit drugs use showed no significant difference between cases and controls. Manual extraction of the placenta was not reported in any cesarean delivery.
The moment when antibiotic prophylaxis was given was recorded for 72 (91%) cases and 70 (88%) controls. Antibiotic prophylaxis was not administered in 8 (11%) case patients compared to 3 (4.3%) control patients, with no statistical difference. Appropriate provision of the antimicrobial prior to cesarean occurred in 16 (22.2%) case patients and 27 (38.6%) control patients.
Antibiotic prophylaxis administered on a timely basis was associated with a lower risk of SSI in univariate analysis [OR 0.46 (0.22–0.95), p=0.049]. However, when a multivariate-adjusted odds ratio analysis was performed the use of prophylaxis at the recommended time was not associated with the risk of developing an SSI after cesarean delivery.
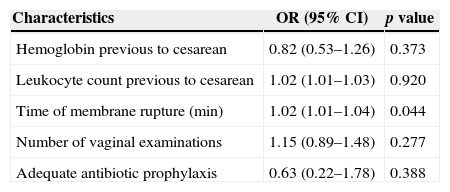
Multivariate analysis to identify independent risk factors associated with SSI (Table 2) was carried out including variables that had p<0.20 in the univariate analysis. Only duration of membrane rupture was considered an independent risk factor for SSI. The remaining risk factors such as hemoglobin level and leukocyte count prior to the obstetric procedure, number of internal vaginal examinations and the correct use of antibiotic prophylaxis were not associated with SSI.
Multivariate analysis to identify independent risk factors associated with surgical site infection.
| Characteristics | OR (95% CI) | p value |
|---|---|---|
| Hemoglobin previous to cesarean | 0.82 (0.53–1.26) | 0.373 |
| Leukocyte count previous to cesarean | 1.02 (1.01–1.03) | 0.920 |
| Time of membrane rupture (min) | 1.02 (1.01–1.04) | 0.044 |
| Number of vaginal examinations | 1.15 (0.89–1.48) | 0.277 |
| Adequate antibiotic prophylaxis | 0.63 (0.22–1.78) | 0.388 |
Using backward stepwise regression analysis to all risk factors evaluated for SSI showed no new result when compared to multivariate analysis of risk factors with p<0.20 in the univariate analysis.
Appropriate prophylaxis was given in 24 (22.6%) of the 106 emergency cesarean deliveries and of these, 11/24 (45.8%) patients had an SSI. The remaining 82 patients from this group have not received suitable prophylaxis and of these, 46/82 (56.1%) had an SSI. There was no statistically significant difference (p=0.099). Appropriate prophylaxis was given in 19 (36.5%) of the 52 elective cesarean delivery patients and of these, 5/19 (26.3%) patients had an SSI. Adequate prophylaxis was not given to 33 patients and of these, 10/33 (30.3%) had an SSI. There was no statistically significant difference (p=0.899).
No significant difference was found when evaluating the subgroups according to type of SSI (superficial, deep and organ/space) for the risk factors assessed, except for those already noted in the group as a whole, especially the duration of the rupture of membranes.
DiscussionIndependent risk factors for post-cesarean SSI, as described in the scientific literature that included multivariate analysis, are young age, obesity, hypertension or preeclampsia, diabetes mellitus, chorioamnionitis, nulliparity, less than seven prenatal visits, extended time from rupture of membranes until cesarean, emergency cesarean delivery, lack of appropriate antibiotic prophylaxis, increased surgical time, and birth of twins.3,14,6,21
It can be quite difficult to estimate the protective effect of antibiotic prophylaxis correctly administered 30–60min prior to the cesarean incision, as antimicrobials are used both prophylactically and therapeutically, with many patients continuing antimicrobial therapy after cesarean delivery.3,15 We tried to eliminate this bias to the maximum in the present study by including in the control group only those patients with no history of infection or antibiotics use until the 30th day postpartum, other than the prophylaxis. Of the 158 study patients, 146 (89%) at the time of prophylaxis had been administered with 2g of intravenous cefazolin noted in their medical records. Univariate analysis showed that the appropriate use of antibiotic prophylaxis was a protective factor for the occurrence of SSI (Table 1), reducing the risk by 54% for any type of SSI, a finding consistent with the literature.22,23 On the other hand, this same protective effect situation did not hold true in the multivariate-adjusted odds ratio analysis (Table 2), suggesting that other variables may have contributed to this result, such as the extended time for ruptured membranes or any comorbidities.
The strength of this study includes the number of participating patients, the evaluated risk factors, and the representative nature of the studied group, given that the Hospital Fêmina is a free and unrestricted tertiary care center serving a large proportion of female patients of the city of Porto Alegre and its metropolitan regions.
The evaluated patients also had a similar demographic profile to the Brazilian pregnant population. The rate of SSI after cesarean delivery during the four-year study period was 1.44%, which is consistent with the data published by the CDC/NHSN (1.46%).24
Limitations of the present research include the lack of evaluation of the indication for a cesarean delivery (elective or emergency) and the absence of data in some medical records, such as the exact time of antimicrobial prophylaxis administration and BMI values. Another important limitation of the study is to have evaluated the patient records in a period in which the recommendation was to perform antibiotic prophylaxis only at the time of cord clamping, rather than 30–60min before the cesarean section incision.
It is important to highlight that patients who had an emergency cesarean had a 3.3-fold greater risk of SSI when compared with the controls. Additionally, no association was found between the administration of antibiotic prophylaxis and SSI neither in patients who underwent emergency cesarean nor in those with elective cesarean.
The present study demonstrated an association on univariate analysis between post-cesarean SSI and number of internal vaginal examinations, time of membrane rupture, emergency cesarean and improper use of antibiotic prophylaxis. However, this same situation did not hold true in the multivariate analysis that adjusts for the other risk factors. Many publications have questioned the use of antenatal antibiotic prophylaxis and the risks it could possibly carry to the mother and fetus, due to both the limited number of adequately powered consistent studies and the small number of post-cesarean complications in specific situations.15,18,25 The authors of the present study not only question its use as a prophylactic agent based on the data presented here and in the literature, but also suggest that prophylaxis perhaps must be indicated in selected groups of patients undergoing cesarean section. Well documented risk factors in the literature, such as emergency cesarean, duration of ruptured membranes, duration of surgery, excessive vaginal manipulation, obesity, and surgical risk must form a part of this decision.18,25 This is a preliminary conclusion and must be reinforced by subsequent studies.
Further research with bigger sample sizes and evaluating additional risk factors are fundamental for a better understanding of the causes and evolution of SSI after cesarean delivery, and in particular the role of antibiotic prophylaxis in its prevention.
Conflicts of interestThe authors declare no conflicts of interest