Syndemic psychosocial and reproductive factors affecting women's retention in HIV care remain understudied. We analyzed correlates of non-retention in a cohort of women with HIV in Brazil from 2000‒2015. Participants self-reported exposure to physical/sexual violence, illicit drug use, adolescent pregnancy, or induced abortion. Lifetime history of these psychosocial stressors were used to create a syndemic score based on the presence or absence of these conditions. All dichotomous variables were summed (range 0 to 4), with greater scores indicating more syndemic factors experienced. Logistic regression models identified predictors of non-retention, defined as < 2 HIV viral load or CD4 results within the first year of enrollment. Of 915 women, non-retention was observed for 18%. Prevalence of syndemic factors was adolescent pregnancy (53.2%), physical/sexual violence (38.3%), induced abortion (27.3%), and illicit drug use (17.2%); 41.2% experienced ≥ 2 syndemic conditions. Syndemic scores of 2 and 3 were associated with non-retention, as well as low education, years with HIV and seroprevalent syphilis. Psychosocial and reproductive syndemics can limit women's retention in HIV care. Syphilis infection predicted non-retention and could be explored as a syndemic factor in future studies.
Retention in HIV care has been associated with virologic suppression, improved survival, and reduced HIV transmission risk at the population level.1-3 As women comprise more than half of adults living with HIV worldwide, strategies to improve retention in care among women are fundamental to achieving the UNAIDS 95-95-95 goals.4,5 Analysis of a large Latin American cohort between 2003‒2012 found that female sex was significantly associated with lower retention compared to males.6 While qualitative studies have explored factors like gender-based violence and child care responsibilities as potential barriers,7,8 our understanding of sex-specific and reproductive factors impacting women's engagement in the HIV care continuum remain limited.
Considering the sociocultural and structural vulnerability of women living with HIV, syndemic theory can provide a useful framework to explore health-related behaviors in this population. Syndemics are defined as mutually-reinforcing, psychosocial conditions that interact synergistically to enhance disease transmission and worsen health outcomes.9 The first and most well-researched syndemic of Substance Abuse, Violence, and AIDS (SAVA) described the interconnectedness of these conditions in impoverished urban environments.10 More recently, syndemics have been associated with poor HIV care outcomes, including Antiretroviral Therapy (ART) non-adherence, higher viral loads, and reduced engagement in care.11,12 However, inclusion of women living with HIV and individuals living outside the United States (U.S.) has been limited in these analyses.13
In the present study, our objective was to assess syndemic prevalence and correlates of non-retention in HIV care among women enrolled in the Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz (INI-Fiocruz) women's cohort in Rio de Janeiro, Brazil. Improved characterization of barriers and facilitators of retention in care for women living with HIV has implications for enhancing health care service delivery in this population and making progress toward the UNAIDS 95-95-95 targets.
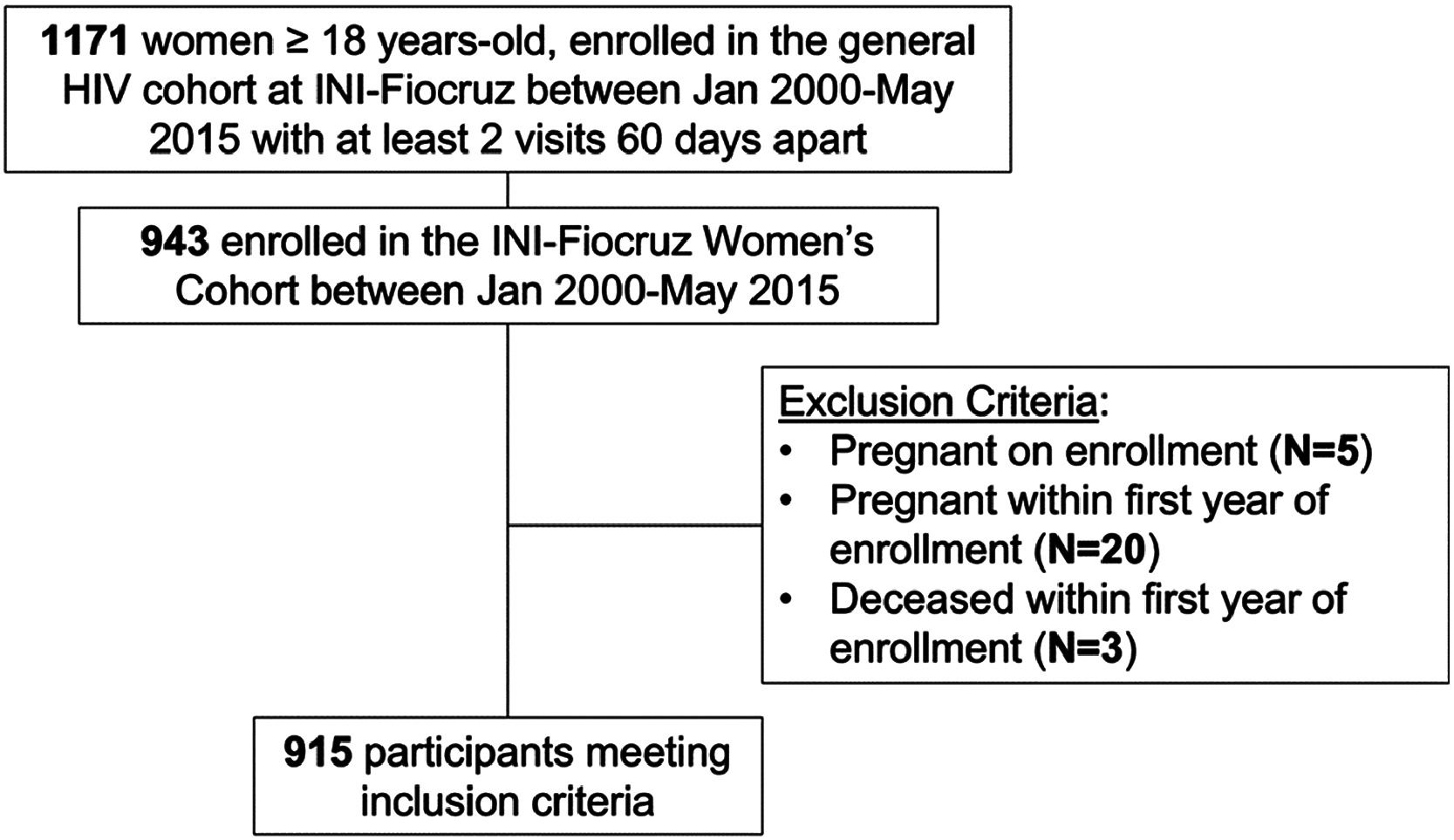
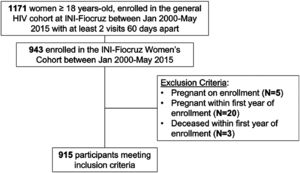
MethodsStudy population and proceduresThe INI-Fiocruz women's cohort is a clinic-based, gynecologic cohort of women living with HIV in Rio de Janeiro, Brazil. Participants undergo study visits every 6‒12 months consisting of face-to-face interviews, clinical and laboratory assessments, and physical exam.14,15 Women with documented HIV infection, who were ≥18 years-old, and who enrolled in the INI-Fiocruz women's cohort between January 2000 and June 2015 were eligible for this analysis. Of note, the cohort ceased enrolling new participants in 2015, therefore additional results were not available beyond this point. Participants were excluded if they were pregnant on enrollment, became pregnant within one year of enrollment, or died within one year of enrollment. Participants were enrolled in the cohort on the first study visit date. The cohort study was approved by the ethics review board at INI-Fiocruz.
Study definitionsDemographic characteristics were self-reported. Race/skin color was categorized as white, black, or mixed, and participants who identified as “other” race (n = 24) were included in the mixed category. Education was dichotomized into ≥ 9 or < 9 years. Year of enrollment was categorized into three time periods (2000‒2004, 2005‒2009, or 2010‒2015). CD4+T-lymphocyte count and HIV-1 RNA baseline values were the measurements recorded closest to the enrollment date, with a window of up to one year before enrollment. ART use was defined as initiating therapy before the cohort enrollment date with a regimen end date occurring after enrollment; time on ART was calculated from the first regimen start date until date of cohort enrollment. AIDS-Defining Illnesses (ADI) were classified according to 1993 Centers for Disease Control and Prevention (CDC) definitions,16 and prior ADI included any diagnosis before women's cohort enrollment and up to 30 days after enrollment. Years living with HIV were calculated based on date of diagnosis until date of cohort enrollment.
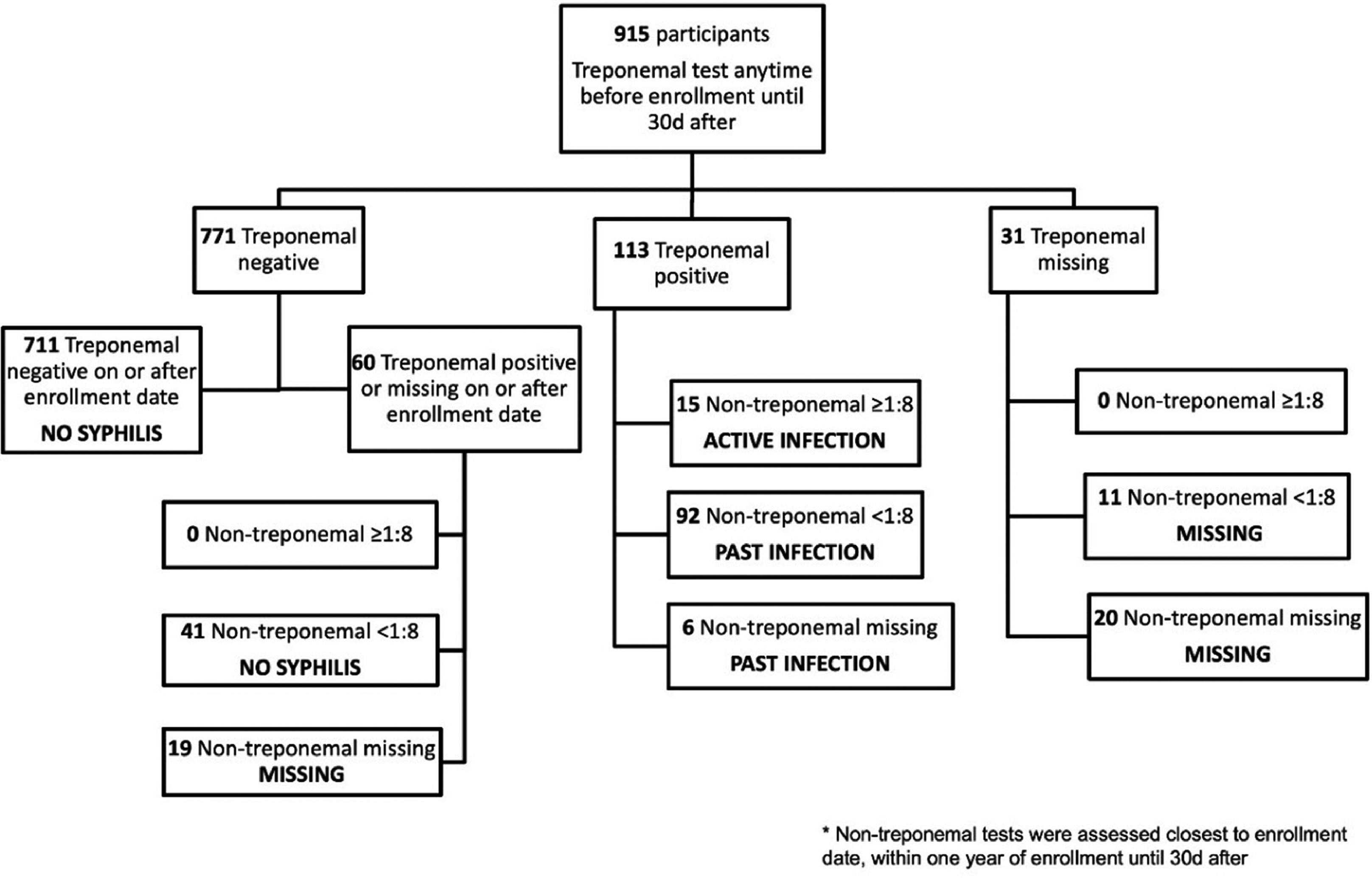
Age at sexual debut was dichotomized into < 15 and ≥ 15 years old. Participants self-reported whether they had a child living with HIV/AIDS; those without any prior births were categorized as a “no” response for this variable. Positive treponemal antibody tests measured any time before cohort enrollment until 30 days after enrollment were used to diagnose seroprevalent syphilis, which included both active and past cases. Active syphilis was defined as a reactive non-treponemal test >1:8 within one year prior to cohort enrollment until 30 days after with positive confirmatory treponemal test. Participants were categorized based on history of prior syphilis testing and treatment as active infection, past infection, or no syphilis infection.
Syndemics were defined as lifetime history of: sexual or physical violence, illicit drug use, adolescent pregnancy, or induced abortion.9,10,17 History of sexual violence was assessed by asking about any prior instances of non-consensual sex; participants were asked about physical violence via the question “Have you suffered any physical aggression not directly related to a sexual practice?”. A positive history of violence was defined as a “yes” response to either question. Participants were asked about lifetime use of each of the following substances: marijuana, intravenous cocaine, intranasal cocaine, and inhalants. A positive response to any of these items was defined as prior illicit drug use. Participants provided their age at first pregnancy to assess prevalence of adolescent pregnancy, which was defined as pregnancy between 10‒19 years of age.18 Participants were asked the total number of prior induced abortions; any response >0 was classified as a lifetime history of induced abortion. Spontaneous abortions were assessed separately and were not included in the induced abortion variable. Women without a prior pregnancy (n = 89) were classified as a “no” response for both the adolescent pregnancy and induced abortion variables. A syndemic score was created by summing the presence or absence of each of the four dichotomous variables: physical/sexual violence, illicit drug use, adolescent pregnancy, induced abortion. One point was assigned to each positive response; therefore, the higher numbers in the sum score indicate greater exposure to syndemic variables. Participants with missing responses for any syndemic variable were classified as a “no” response for the sum score calculation.
Retention in HIV care was defined as completing HIV monitoring laboratory tests (CD4+ T-lymphocyte count or HIV-1 RNA PCR) on two or more visits at least 90 days apart within the first year of enrollment in the women's cohort.19
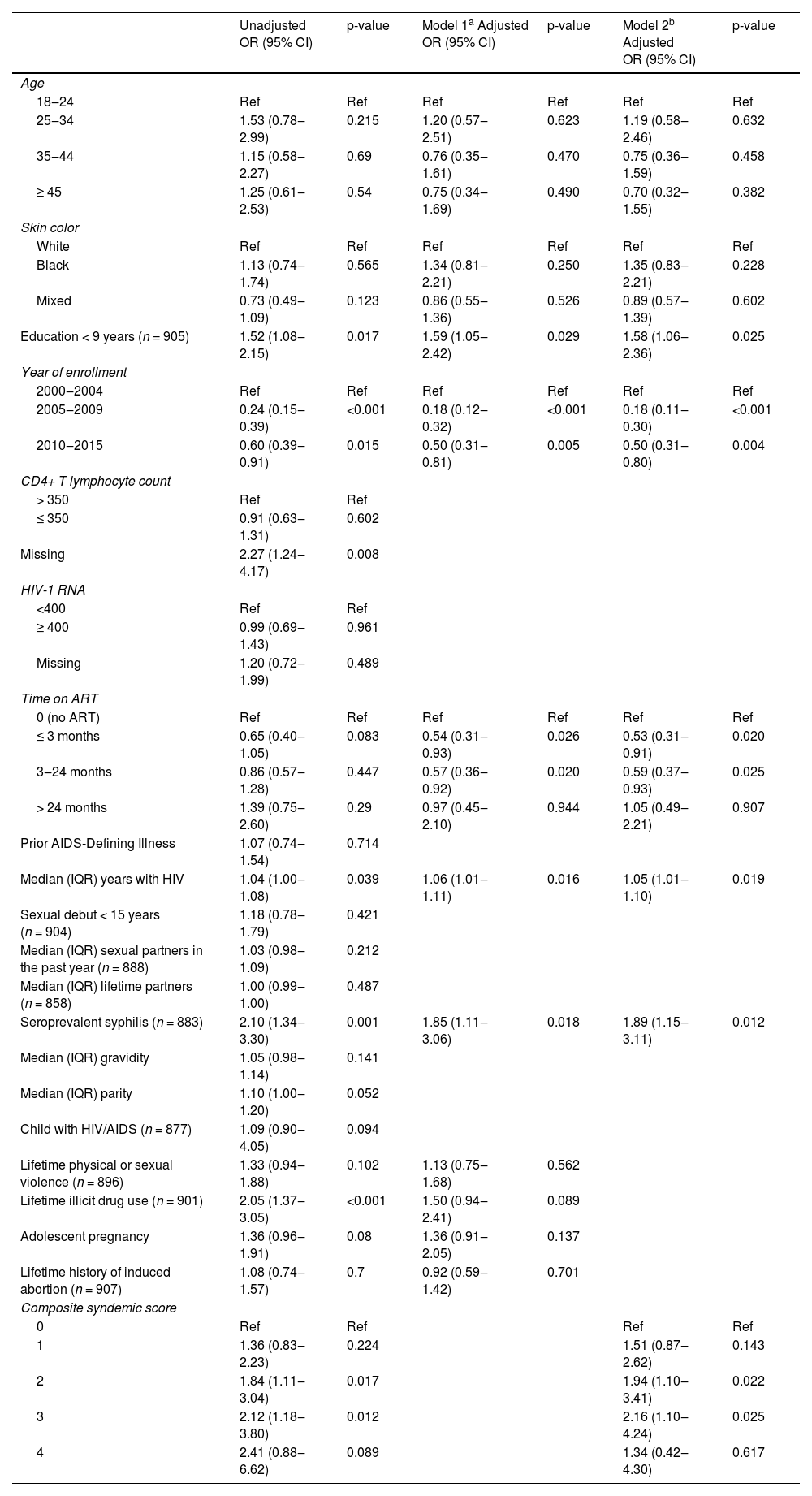
Statistical analysisWe performed descriptive analyses of baseline demographic, psychosocial, behavioral, and clinical characteristics, stratified by retention status. Comparisons between retained and non-retained groups were conducted using Chi-Squared tests for categorical variables and Rank-sum tests for continuous variables. Bivariate logistic regressions were performed to test associations between the four syndemic variables, as proposed by Stall et al.20
Unadjusted logistic regression models were used to identify variables associated with non-retention. Stepwise backward logistic regression was performed, whereby all variables with p-value <0.20 were included in the adjusted model. Variables with p-value >0.05 were removed and a final model was reached for all variables with p-value < 0.05. Age and race were forced into the models due to previous associations with retention in the literature.21,22 The association between syndemics and non-retention was tested using two multivariate logistic regression models: Model 1 incorporated individual syndemic variables, and Model 2 used the syndemic sum score. Variables included in the regression models are outlined in Table 3.
Interaction effects among syndemic variables were tested using multiplicative models and via calculation of the unadjusted and adjusted Relative Excess Risk due to Interaction (RERI).23 Additionally, baseline characteristics were stratified by syphilis status at cohort entry. Participants with missing treponemal or non-treponemal tests at baseline (n = 50) were excluded from these analyses. Differences were assessed using chi-square or Fisher's exact tests for categorical variables and Kruskal-Wallis tests for continuous variables. Bivariate regressions were performed to test associations between seroprevalent syphilis and all syndemic variables. R (version 3.3.1) was used for all analyses.
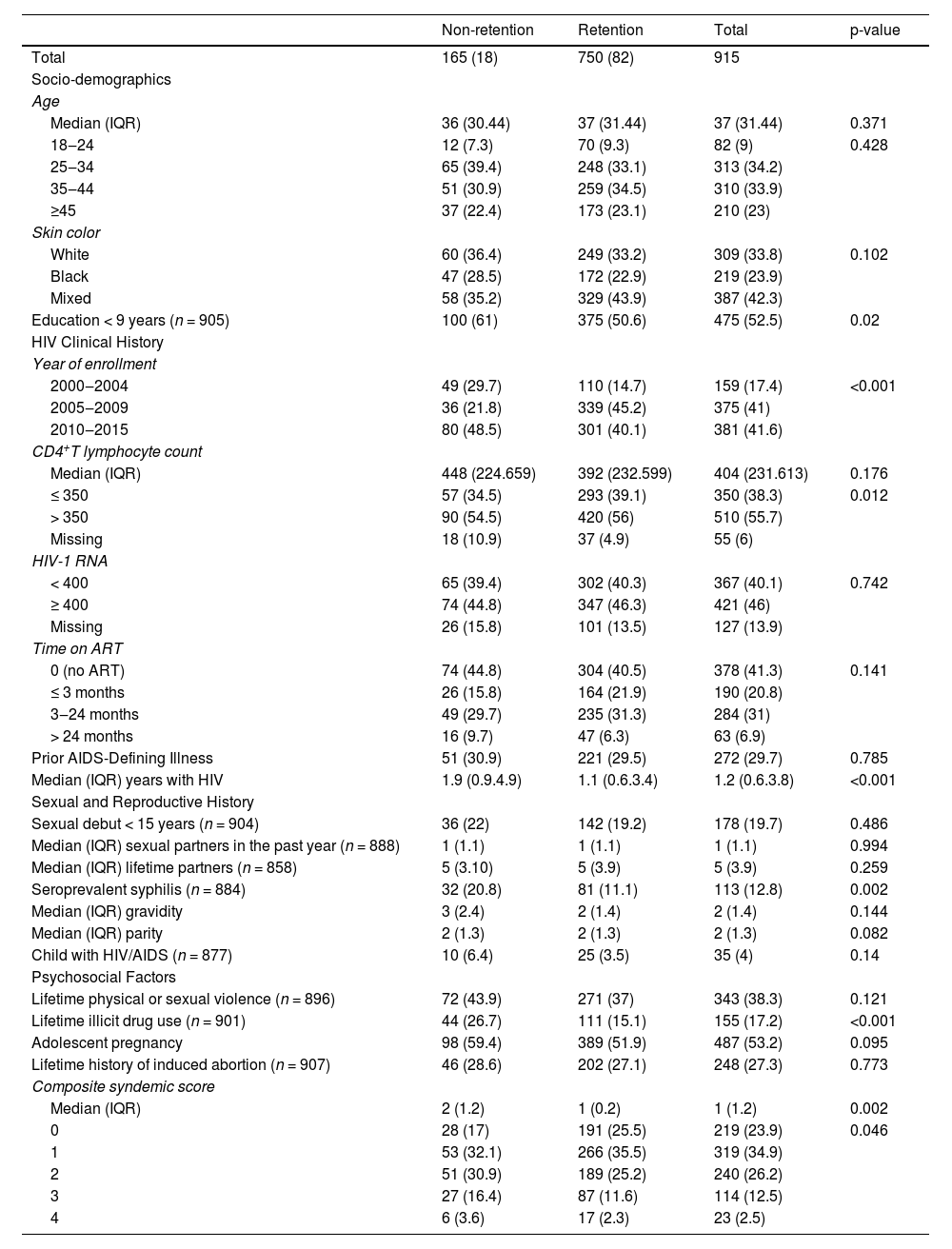
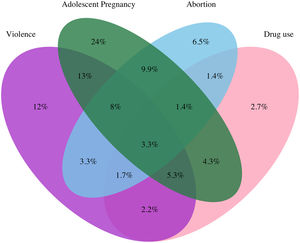
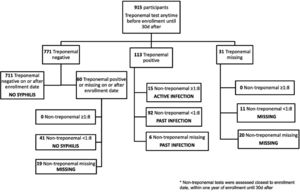
ResultsOverall, 915 women met inclusion criteria (Fig. 1). Eighteen percent (n = 165) of the study population were defined as “not retained in HIV care”. The median age at enrollment was 37 years (IQR 31‒44). Most participants were black or mixed race (66.2%) and had < 9 years of education (52.5%). Median CD4+T-lymphocyte count (CD4 count) on enrollment was 404 cell/mm³ (IQR 231‒613). At baseline, 41.3% of women were not on ART, 46% had HIV-1 RNA ≥ 400 copies/mL, and 29.1% were previously diagnosed with an ADI. Seroprevalent syphilis was diagnosed in 12.8% of our sample. Prevalence of syndemic factors were physical/sexual violence (38.3%), illicit drug use (17.2%), adolescent pregnancy (53.2%), and induced abortion (27.3%). Nearly half of participants (41.2%) experienced ≥ 2 syndemic conditions (Table 1).
Baseline socio-demographic, clinical, reproductive, and psychosocial factors by retention status among women living with HIV in Brazil, 2000‒2015.
Women who were not retained in HIV care were more likely to have: < 9 years education (61.0 vs. 50.6%, p = 0.020), longer duration of HIV diagnosis (median years 1.9 vs. 1.1, p = 0.016), and seroprevalent syphilis (20.8 vs. 11.1%, p = 0.002). History of illicit drug use (26.7 vs. 15.1%, p < 0.001) and higher composite syndemic score (median IQR 2(1,2) vs. 1(0,2), p = 0.002) were also more common among non-retained women. Two or more syndemic conditions were experienced by 39.1% and 50.9% of the women who were retained and non-retained in care, respectively (p = 0.002). Apart from seroprevalent syphilis, sexual and reproductive health variables (e.g., sexual debut, recent partners, lifetime partners, gravidity, and parity) did not differ significantly between retained and non-retained participants (Table 1).
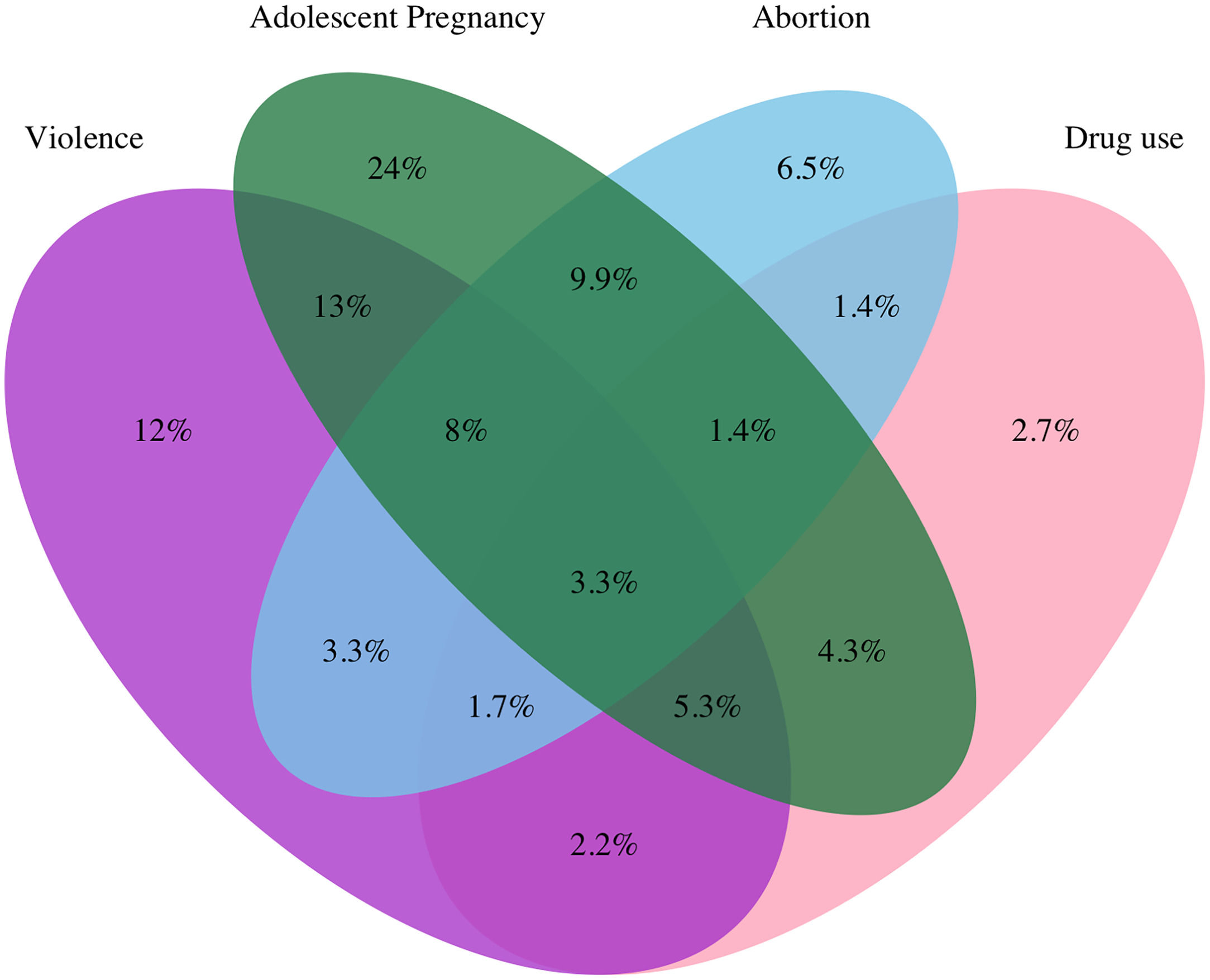
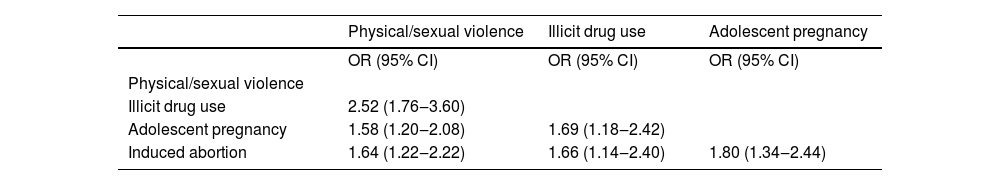
Among participants with at least one syndemic factor, 3.3% experienced all four conditions. The largest areas of overlap were between physical/sexual violence and adolescent pregnancy (13%), and adolescent pregnancy and induced abortion (9.9%) (Fig. 2). Bivariate logistic regressions showed that all syndemic factors were significantly associated with each other, with the strongest association between illicit drug use and physical/sexual violence (OR = 2.52, 95% CI 1.76-3.60) (Table 2). Seroprevalent syphilis was significantly associated with physical/sexual violence (OR = 1.57, 95% CI 1.05‒2.35) and illicit drug use (OR = 2.48, 95% CI 1.59‒3.87).
In the unadjusted models, < 9 years of education, missing CD4 laboratory result at baseline, longer duration of HIV diagnosis, and seroprevalent syphilis were all significantly associated with non-retention (p = 0.017, 0.008, 0.039, and 0.001, respectively). Illicit drug use (p < 0.001) and the presence of 2 and 3 syndemic factors (p = 0.017, p = 0.012) were also associated with non-retention in unadjusted analyses. Cohort enrollment in later years, between 2005‒2009 and 2010‒2015, was associated with improved retention (p < 0.001 and p = 0.015, respectively). Age and race were not found to be significantly associated with non-retention in unadjusted or adjusted models (Table 3).
Unadjusted and adjusted associations with non-retention in HIV care among women living with HIV in Brazil, 2000‒2015.
| Unadjusted OR (95% CI) | p-value | Model 1a Adjusted OR (95% CI) | p-value | Model 2b Adjusted OR (95% CI) | p-value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18‒24 | Ref | Ref | Ref | Ref | Ref | Ref |
| 25‒34 | 1.53 (0.78‒2.99) | 0.215 | 1.20 (0.57‒2.51) | 0.623 | 1.19 (0.58‒2.46) | 0.632 |
| 35‒44 | 1.15 (0.58‒2.27) | 0.69 | 0.76 (0.35‒1.61) | 0.470 | 0.75 (0.36‒1.59) | 0.458 |
| ≥ 45 | 1.25 (0.61‒2.53) | 0.54 | 0.75 (0.34‒1.69) | 0.490 | 0.70 (0.32‒1.55) | 0.382 |
| Skin color | ||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 1.13 (0.74‒1.74) | 0.565 | 1.34 (0.81‒2.21) | 0.250 | 1.35 (0.83‒2.21) | 0.228 |
| Mixed | 0.73 (0.49‒1.09) | 0.123 | 0.86 (0.55‒1.36) | 0.526 | 0.89 (0.57‒1.39) | 0.602 |
| Education < 9 years (n = 905) | 1.52 (1.08‒2.15) | 0.017 | 1.59 (1.05‒2.42) | 0.029 | 1.58 (1.06‒2.36) | 0.025 |
| Year of enrollment | ||||||
| 2000‒2004 | Ref | Ref | Ref | Ref | Ref | Ref |
| 2005‒2009 | 0.24 (0.15‒0.39) | <0.001 | 0.18 (0.12‒0.32) | <0.001 | 0.18 (0.11‒0.30) | <0.001 |
| 2010‒2015 | 0.60 (0.39‒0.91) | 0.015 | 0.50 (0.31‒0.81) | 0.005 | 0.50 (0.31‒0.80) | 0.004 |
| CD4+ T lymphocyte count | ||||||
| > 350 | Ref | Ref | ||||
| ≤ 350 | 0.91 (0.63‒1.31) | 0.602 | ||||
| Missing | 2.27 (1.24‒4.17) | 0.008 | ||||
| HIV-1 RNA | ||||||
| <400 | Ref | Ref | ||||
| ≥ 400 | 0.99 (0.69‒1.43) | 0.961 | ||||
| Missing | 1.20 (0.72‒1.99) | 0.489 | ||||
| Time on ART | ||||||
| 0 (no ART) | Ref | Ref | Ref | Ref | Ref | Ref |
| ≤ 3 months | 0.65 (0.40‒1.05) | 0.083 | 0.54 (0.31‒0.93) | 0.026 | 0.53 (0.31‒0.91) | 0.020 |
| 3‒24 months | 0.86 (0.57‒1.28) | 0.447 | 0.57 (0.36‒0.92) | 0.020 | 0.59 (0.37‒0.93) | 0.025 |
| > 24 months | 1.39 (0.75‒2.60) | 0.29 | 0.97 (0.45‒2.10) | 0.944 | 1.05 (0.49‒2.21) | 0.907 |
| Prior AIDS-Defining Illness | 1.07 (0.74‒1.54) | 0.714 | ||||
| Median (IQR) years with HIV | 1.04 (1.00‒1.08) | 0.039 | 1.06 (1.01‒1.11) | 0.016 | 1.05 (1.01‒1.10) | 0.019 |
| Sexual debut < 15 years (n = 904) | 1.18 (0.78‒1.79) | 0.421 | ||||
| Median (IQR) sexual partners in the past year (n = 888) | 1.03 (0.98‒1.09) | 0.212 | ||||
| Median (IQR) lifetime partners (n = 858) | 1.00 (0.99‒1.00) | 0.487 | ||||
| Seroprevalent syphilis (n = 883) | 2.10 (1.34‒3.30) | 0.001 | 1.85 (1.11‒3.06) | 0.018 | 1.89 (1.15‒3.11) | 0.012 |
| Median (IQR) gravidity | 1.05 (0.98‒1.14) | 0.141 | ||||
| Median (IQR) parity | 1.10 (1.00‒1.20) | 0.052 | ||||
| Child with HIV/AIDS (n = 877) | 1.09 (0.90‒4.05) | 0.094 | ||||
| Lifetime physical or sexual violence (n = 896) | 1.33 (0.94‒1.88) | 0.102 | 1.13 (0.75‒1.68) | 0.562 | ||
| Lifetime illicit drug use (n = 901) | 2.05 (1.37‒3.05) | <0.001 | 1.50 (0.94‒2.41) | 0.089 | ||
| Adolescent pregnancy | 1.36 (0.96‒1.91) | 0.08 | 1.36 (0.91‒2.05) | 0.137 | ||
| Lifetime history of induced abortion (n = 907) | 1.08 (0.74‒1.57) | 0.7 | 0.92 (0.59‒1.42) | 0.701 | ||
| Composite syndemic score | ||||||
| 0 | Ref | Ref | Ref | Ref | ||
| 1 | 1.36 (0.83‒2.23) | 0.224 | 1.51 (0.87‒2.62) | 0.143 | ||
| 2 | 1.84 (1.11‒3.04) | 0.017 | 1.94 (1.10‒3.41) | 0.022 | ||
| 3 | 2.12 (1.18‒3.80) | 0.012 | 2.16 (1.10‒4.24) | 0.025 | ||
| 4 | 2.41 (0.88‒6.62) | 0.089 | 1.34 (0.42‒4.30) | 0.617 |
In multivariate Model 1, the following variables were associated with non-retention: <9 years education (aOR = 1.59, 95% CI 1.05‒2.42), years with HIV (odds per year) (aOR = 1.06, 95% CI 1.01‒1.11), and seroprevalent syphilis (active and past infections) (aOR = 1.85, 95% CI 1.11‒3.06). Enrollment in 2005‒2009 and 2010‒2015 (aOR = 0.18, 95% CI 0.12‒0.32; aOR = 0.50, 95% CI 0.31‒0.81) was less likely to be associated with non-retention. We also found improved retention for women with ART initiation within 3 months of women's cohort enrollment (aOR = 0.54, 95% CI 0.31‒0.93) and within 3‒24 months (aOR = 0.57, 95% CI 0.36‒0.92). Associations between individual syndemic factors and non-retention did not reach statistical significance. However, in Model 2, syndemic sum scores of 2 (aOR = 1.94, 95% CI 1.10‒3.41) and 3 (aOR = 2.16, 95% CI 1.10‒4.24) were significantly associated with non-retention. The effect of the other covariates remained the same (Table 3). We did not find statistical evidence of interactive effects among the syndemic factors in our analysis (Supplemental Digital Content).
We stratified baseline characteristics of study participants by syphilis status. Among participants with complete serologic results on enrollment, 1.7% had active syphilis infection and 11.3% had evidence of past infection (Fig. 3, Supplemental Digital Content). Women with active or past syphilis infection were older, with a median age of 40 and 41 years, respectively (p = 0.002). A greater proportion of active cases were among black women (60% vs. 13.3% white), and there were more past cases reported among mixed-race women (46.9% vs. 26.5% white). Most participants with syphilis diagnoses had <9 years of education (71.4% active and 70.1% past vs. 52.5% overall, p < 0.001). A history of illicit drug use among women with syphilis infection was also common (33.3% active and 30.6% past vs. 17.2% overall, p < 0.001). Women with a history of past infection were more likely to have a higher syndemic score than any other group – median (IQR) 2 (1,2) for past versus 1 (1,2) overall (p < 0.001) (Supplemental Digital Content).
DiscussionOur results show a high proportion of women retained in HIV care and an important effect of syndemic factors on retention. Non-retained women experienced a disproportionate burden of concurrent adverse psychosocial and reproductive factors, i.e., syndemics. We observed a doubling of non-retention odds when multiple syndemic factors were combined. This study is the first, to our knowledge, to quantitatively show that reproductive characteristics can impact HIV care outcomes when combined with other social stressors in a syndemic fashion. The association between syphilis and non-retention, independent of certain sexual behavior risk factors, is also a novel finding with implications for targeting interventions to improve HIV care outcomes among vulnerable women living with HIV.
Overall, 18% of women in the INI-Fiocruz cohort were not retained in HIV care. This proportion is somewhat lower than rates observed among women enrolled in large cohorts across Latin America (26%) and North America (25%).6,24 Although prior studies have found associations between retention and clinical characteristics like CD4+ T-lymphocyte count and ADIs,25 our results suggest that sociodemographic and behavioral factors may be more relevant determinants of retention among urban Brazilian women. In conjunction with prior studies in Brazil and elsewhere, participants with limited education had a higher likelihood of being non-retained in care.22,26 Interventions targeting lower education populations to promote healthcare access or provide multidisciplinary support services may improve retention in HIV care.27,28
Regarding syndemic factors, our variable selection was rooted in both quantitative and theoretical literature. The SAVA syndemic has been well documented,9 along with studies demonstrating potential mechanisms for substance use and violence to limit healthcare engagement, including social instability, provider mistrust, and mental illness.7,29 Ostrach, Lerman & Singer have proposed that stigmatized reproductive options can adversely impact women's health in a syndemic fashion.17 The experience of adolescent pregnancy and induced abortion, particularly in societies where these pregnancies are “socially pathologized”, can potentiate internalized stigma, social exclusion, and medical complications for these women. Improved understanding of reproductive syndemics has implications for targeting interventions to support healthcare engagement for vulnerable women living with HIV. Syndemic psychosocial factors have been correlated with sexual risk behaviors and decreased healthcare utilization in U.S. women.30-32 Higher SAVA scores were also predictive of reduced viral suppression among women of color living with HIV in the U.S.33 Given that only 25% of quantitative syndemic studies (including both men and women) have occurred outside of the U.S., more research is needed to contextualize the impact of syndemics in low and middle income countries.13 Although understudied, reproductive stigma is rooted in political and cultural norms,34 and likely exhibits dramatic global variation.
Substance use and violence have also been correlated with unintended pregnancy in Brazil and elsewhere.35,36 Given the potential stigma surrounding adolescent pregnancy and induced abortion in the Brazilian context, we hypothesized that these experiences would act synergistically to reduce retention in HIV care. Perceived abortion stigma, for example, deters women from seeking treatment for complications and is associated with higher levels of psychologic distress post-procedure.37,38 Adolescent pregnancy can similarly perpetuate negative health consequences via social exclusion and economic disadvantage resulting from lost educational opportunities.17,39
Nearly half (41.2%) of women in the INI-Fiocruz cohort reported two or more syndemic factors. Although direct comparisons of syndemic prevalence are difficult due to varying study definitions, prior studies among other socially-vulnerable women found that 46.9%‒61.5% reported ≥2 syndemic conditions.30,31 Our findings are consistent with Biello and colleagues’ analysis of MSM in Latin America, which showed increasing odds of non-retention in HIV care with increasing number of syndemic factors.12 However, the dose-response relationship we observed did not persist in adjusted models, most likely due to the small proportion of women experiencing all four conditions.
Among individual syndemic factors, we found illicit drug use correlated with non-retention in unadjusted models, as found in previous studies of U.S. women.21,40 Our sample size and lower prevalence of drug use compared to North American cohorts may have limited our ability to detect differences in retention rates in the adjusted models.41,42 Substantial underreporting may also have occurred for syndemic factors like drug use and induced abortion that are illegal and highly stigmatized in Brazil.43 Despite the lack of statistical significance in Model 1, the high prevalence of syndemic factors and dose-response effects demonstrated in Model 2 suggests that interventions addressing substance use, interpersonal violence, and reproductive stigma are needed to advance comprehensive HIV care for Brazilian women.
Seroprevalent syphilis was an independent predictor of non-retention, apart from sexual risk factors of early sexual debut, multiple recent partners, and number of lifetime partners. Prior studies have associated syndemics with sexual risk behavior,30,44 incident syphilis,45 and other Sexually Transmitted Infections (STIs).31 One analysis of sexual minority women in the U.S. found positive correlations between health-related and behavioral syndemic factors, including history of STIs.46 In our sample, syphilis cases were concentrated among women of non-white race, low educational attainment, and history of illicit drug use. Singer's original syndemic description proposed that socioeconomic stressors such as poverty, chronic stress, and substance use can contribute to biologic and behavioral susceptibility to STIs.10 More recent research has shown that STIs can cluster in neighborhoods with greater social disorder and disadvantage.47 As such, syphilis infection may be an indicator of social vulnerability (perhaps through unstable partnerships, commercial sex work, or limited health access) in our cohort. Further research is needed to elucidate potential mechanisms underlying this exploratory finding, that is particularly relevant as syphilis incidence and the proportion of cases among women continues to increase in Brazil.48
Finally, our finding that non-retention correlated with earlier years of cohort enrollment was observed in a previous study of the INI-Fiocruz HIV clinical cohort. The authors attributed improvements in retention to increased staffing, decreased HIV testing costs, and enhanced laboratory capacity that occurred in the early 2000s.22 We also found that ART initiation within two years of cohort enrollment improved retention in HIV care, compared to women not on ART at baseline. Early ART initiation after diagnosis has been associated with improved retention and other beneficial HIV outcomes.49 As well, participants may have been monitored more closely to evaluate immunologic response following treatment initiation. Longer duration of HIV disease was also associated with non-retention, perhaps due to either clinical stability or feeling too sick to attend appointments.50
Our study has several limitations. Open enrollment procedures used in the INI-Fiocruz women's cohort may limit generalizability to other populations living with HIV because of non-probabilistic sampling. Findings may also not be applicable to non-urban centers, as our study population was concentrated in a metropolitan area. Due to limitations in our data collection, we could not establish whether syndemic conditions occurred simultaneously. However, the literature supports the use of lifetime history in syndemic analyses, particularly for traumatic events.20 We were unable to account for mental health disorders, alcohol consumption, and unstable housing, which have been previously associated with non-retention among women in the literature.21,40 Given the social vulnerability of the INI-Fiocruz women's cohort,15 incorporation of these characteristics would have potentially increased our overall syndemic prevalence and likely further supported the associations we observed. Lastly, we did not find evidence of synergistic effects among syndemic factors when testing interactions, most likely due to small sample size. Few syndemic studies have found statistical evidence for interaction,23 and future research could consider combining datasets to explore multiplicative effects in accordance with original syndemic theory.
In conclusion, improved interventions are needed to address suboptimal HIV healthcare engagement among vulnerable women living with HIV. Future studies should address these important challenges and consider incorporating reproductive variables and syphilis infection into syndemic analyses. Recognizing and characterizing sex-specific risk factors and designing targeted interventions is critical to moving the needle towards the 95-95-95 goals worldwide.
We would like to thank the INI-Fiocruz study participants and staff who devoted their time and efforts to make this project possible. This work was supported in part by NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (leDEA) (U01AI069923) and the Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz. This work was also supported in part by the Doris Duke Charitable Foundation through a grant supporting the Doris Duke International Clinical Research Fellows Program at the University of California San Francisco. CMZ is a Doris Duke International Clinical Research Fellow. This work was also supported by the US National Institute of Health grantsNIH R25 MH087222 to JLC and K23 AI110532 to JEL. BG acknowledges funding from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (305789/2019-8) and FAPERJ (E-26/202.915/2018). PML acknowledges funding from CNPq (316401/2021-8) and FAPERJ (E-26/201.133/2021). RBDB acknowledges funding from the Research Funding Agency of the State of Rio de Janeiro (FAPERJ)E-26/203.154/2017 and from the National Council of Technological and Scientific Development (CNPq)310541/2017-4.