Health care-associated infection remains a significant hazard for hospitalized patients. Hand hygiene is a fundamental action for ensuring patient safety.
ObjectiveTo promote adoption of World Health Organization Hand Hygiene Guidelines to enhance compliance among doctors and nurses and improve patient safety.
MethodsThe study design was a cross sectional intervention in a Federal Teaching Hospital South-eastern Nigeria. Interventions involved training/education; introduction of hand rub; and hand hygiene reminders. The impact of interventions and hand hygiene compliance were evaluated using World Health Organization direct observation technique.
ResultsThe post-intervention hand hygiene compliance rate was 65.3%. Hand hygiene indications showed highest compliance rate ‘after body fluid exposure’ (75.3%) and ‘after touching a patient’ (73.6%) while the least compliance rate was recorded ‘before touching a patient’ (58.0%). Hand hygiene compliance rate was significantly higher among nurses (72.9%) compared to doctors (59.7%) (χ2=23.8, p<0.05). Hand hygiene indication with significantly higher compliance rate was “before clean/aseptic procedure” (84.4%) (χ2=80.74, p<0.05). Out of the 815 hand hygiene practices recorded 550 (67.5%) were hand rub action.
Conclusionshand hygiene campaigns using the World Health Organization tools and methodology can be successfully executed in a tertiary health facility of a low-income setting with far reaching improvements in compliance.
Health care-associated infection (HCAI) transmission in the hospital environment remains a significant hazard for hospitalized patients and health-care workers are potential source of these infections.1–3 According to World Health Organization (WHO) an infection is considered a HCAI if it is occurring in a patient during the process of care in a hospital or other health-care facility which was not present or incubating at the time of admission, this includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility.3 It is estimated that at any one time, more than 1.4 million people worldwide are suffering from infections acquired in hospitals.2–4 Since most HCAIs can be transmitted from patient to patient via the hands of health-care workers, hand hygiene is the simplest proven method to reduce the incidence of health care-associated infections. This is the rationale behind the time-honoured advice for all to wash their hands before and after seeing each patient because there is substantial evidence that hand antisepsis reduces the incidence of HCAI.5 Hand hygiene is therefore a fundamental action for ensuring patient safety, which should occur in a timely and effective manner in the process of care.6 However, despite the fact that compliance with hand hygiene among all types of health-care workers remains poor,7 identifying effective methods to improve the practice of hand hygiene would greatly enhance patient safety and result in a significant decrease in HCAIs.
The WHO noted that successful and sustained hand hygiene improvement is achieved by implementing multiple actions to tackle different obstacles and behavioural barriers.3 Based on the evidence and recommendations from the WHO Guidelines on Hand Hygiene in Health Care,3,8 the following components make up an effective multimodal strategy for hand hygiene; (i) System change; (ii) Training/Education; (iii) Evaluation and feedback; (iv) Reminders in the workplace; and (v) Institutional safety climate.
Nigeria is one of the countries with high burden of HCAIs,9,10 yet the hand hygiene campaign is not commonly promoted in many health care facilities in the country. To the best of our knowledge there is currently no systematic study on hand hygiene promotion and evaluation in health facilities in Nigeria. The absence of such information hampers the development of effective policies on hand hygiene both at national and local levels. There is sufficient evidence from published research which suggests that multimodal, multidisciplinary strategies that focus on system change, training and monitoring have a great potential of success in terms of hand hygiene improvement, and reduction of HCAI.11–13
The specific objectives of the study were as follows: to Identify the factors associated with non-compliance with hand hygiene among medical doctors and nurses; to promote the adoption of the recommendations of the WHO Guidelines on Hand Hygiene in Health Care,3,8 in particular the implementation of two of the components (Training/Education and Reminders in the workplace) of the multidisciplinary, multimodal hand hygiene improvement strategies; and to evaluate hand hygiene compliance using the WHO evaluation and feedback methodology.
Materials and methodsSettingThe study took place from January 2010 to April 2011 at The Federal Teaching Hospital Abakaliki (FETHA) (formerly Ebonyi State University Teaching Hospital and Federal Medical Centre) of Ebonyi State, Southeastern Nigeria. The study targeted physicians, nurses, and other health workers involved in direct patient contact. In this research both the institutional and international guidelines on research ethics were strictly adhered to in all aspects of the project. The study was approved by the Ethics Committee of the hospital and by Ethical Review Committee of WHO.
Study designThe research design was a cross sectional intervention. The study was divided into two phases: the intervention phase and evaluation phase.
The intervention phaseConsultation/advocacy meetings were held in January 2010 by the Research Team with the management and major stakeholders (Chief Resident Doctors and Heads of Nursing Services Department) of the Hospital. The purpose of the meeting was to canvass for their co-operation and support towards achieving the goals and objectives of the project.
The intervention phase lasted for seven months, from January 2010 to July 2010. The major activities were as follows:
- (a)
Initiation and execution of WHO recommended activities for implementation of Intervention: This involved the implementation of strategies that promoted hand hygiene compliance as health care facility priority. Activities executed were training/education and use of reminders in the work place as recommended by WHO. The training/education sessions were conducted separately for nurses and doctors. Before the commencement of each training session, a questionnaire was administered. The questionnaire assessed the knowledge, attitudes, and practices (KAP) of the health workers on hand hygiene practices. The training was conducted by the Research Team at the Hospital's conference hall using PowerPoint presentation, and training handouts given to each participant. The training on hand hygiene focused on: background to WHO Patient Safety and the First Global Patient Safety Challenge; definition, effect and burden of HCAI; major patterns of transmission of health care-associated pathogens, with a particular focus on hand transmission; prevention of HCAI and the critical role of hand hygiene; WHO Guidelines on Hand Hygiene in Health Care and their implementation strategy and tools, including why, when and how to perform hand hygiene in health care.3,8
Each training session lasted for 2½–3½h and also involved a focus group discussion (FGD) comprising of 5–10 doctors and 6–12 nurses per group. The FGD identified the factors associated with non-compliance with hand hygiene and consistent stethoscope disinfection practices and the potential solutions to address them. A total of nine training sessions were held. A specialized training session was also conducted for selected nurses who served as observers of hand hygiene compliance during the evaluation phase of the study. The observers were taught how to openly and objectively observe and monitor hand practices and to gather data on hand hygiene using the WHO five hand hygiene indications and methodology.
The tools for the training sessions were downloaded from the WHO URL (http://www.who.int/gpsc/5may/tools/training_education/en/index.html).
- (b)
Use of reminders in the workplace: After the completion of all training activities, materials used as reminders were downloaded from WHO Patient Safety website (http://www.who.int/gpsc/5may/tools/workplace_reminders/en/index.html) and were reproduced in the forms of posters, prescription notebooks, and computer screen savers. Two posters were produced and these include (i) “Your 5 Moments for Hand Hygiene” and (ii). “How to Hand rub and Hand wash”. The hand hygiene posters were pasted in all the hospital wards at strategic locations such as: near wash hand sink, beside beds, consultation rooms, at all points where health worker–patient contact occurs.
- (c)
Introduction of alcohol hand rub: Hundreds of units of 250mL 70% isopropyl alcohol hand rub were procured by the Project Team and were placed in strategic ‘points of care’ places within the hospital. The Head of Nursing Services Department (HNSD) was in-charge of its distribution to the various hospital wards. The Project Team worked with the HNSD to ensure the availability of the hand rubs throughout the project implementation and evaluation period. The trained observers and ward/unit heads monitored the usage of the hand rubs and ensured prompt replacement of depleted containers.
The Project Evaluation Phase covered the period from September 2010 to March 2011. During this phase the hand hygiene compliance was evaluated using the direct observation technique described in the WHO Hand Hygiene Technical Reference Manual (HHTRM).14 The WHO Hand Hygiene Observation Form was used for the evaluation by trained observers. The observation data wre collected anonymously and kept confidential. The observers openly and objectively observed practices and gathered data on hand hygiene using the five indications in line with the methodology and instructions specified in the WHO HHTRM. The period of observation was formally announced to the head nurse, consultants and chief residents of the various units and departments. The observers were instructed to respect patients’ privacy and not interfere with health-care activities being carried out during the session. Observers were also instructed to not perform the observation in extreme situations (e.g., in high emergency medical treatment) since they may not reflect a “standard” care situation. All observers stood or sat close to the point of care while observing; close enough to see but not interfere with patient care activities. Each observation lasted 30–60min. Each observation form was checked immediately after the observation session and the end time, duration of session and signature was entered.
Data analysisData obtained from the study was analyzed using the Epi Info software (downloaded from http://www.cdc.gov/epiinfo/epiinfo.htm). The Epi Info was used to analyze the data collected via the Hand Hygiene Observation Form which is one of the WHO hand hygiene evaluation tools (available at http://www.who.int/gpsc/5themay/tools/evaluation_feedback/en/index.html). The analysis was performed according to the recommendations of WHO Hand Hygiene Reference Manual.14
ResultsA total of 202 health workers (39 doctors and 163 nurses) were trained in a series of workshops during the intervention phase, while 37 other doctors who could not attend the training workshops received the workshop training materials via email. As at the time of conducting this study the hospital had about 301 nurses and 167 doctors making a total of 468 health workers. Out of this number the 202 trained represented 43%. After the intervention, a total of 209 health workers were observed for hand hygiene compliance using the WHO direct observation method. These included 106 (50.7%) doctors, 73 (34.9%) nurses, 25 (12.0%) midwives, and 5 (2.4%) other health workers.
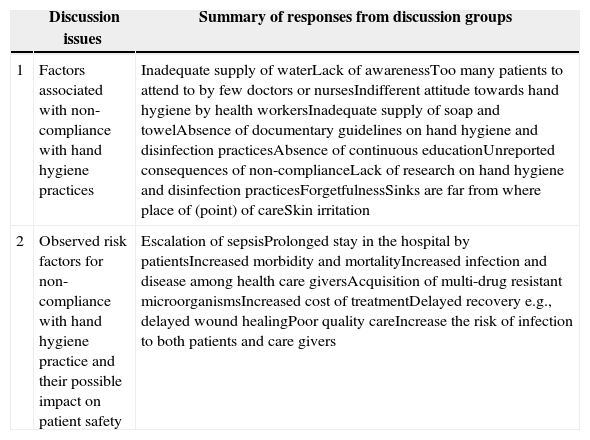
A summary of the main factors associated with non-compliance with hand hygiene identified by the doctors and nurses during the focus group discussion conducted during the training programme included: inadequate supply of water, soap and towel; lack of awareness; inadequate manpower; absence of guidelines on hand hygiene and disinfection practices; unreported consequences of non-compliance; etc. (Table 1). The doctors and the nurses stressed the importance of hand hygiene in the prevention of HCAI, and the need for regular re-orientation and training of health care workers on this. The importance of improvement of facilities was also stressed. They advocated the need for policies on hand hygiene and other patient safety issues and the establishment of a monitoring/supervision mechanism to ensure compliance. The need for the employment of more health care workers and commitment on the part of the nurses and doctors to adhere to patient safety guidelines were also stressed (Table 2).
The outcome of focus group discussion on factors associated with non-compliance with hand hygiene among doctors and nurses at Federal Teaching Hospital Abakaliki Nigeria.
| Discussion issues | Summary of responses from discussion groups | |
|---|---|---|
| 1 | Factors associated with non-compliance with hand hygiene practices | Inadequate supply of waterLack of awarenessToo many patients to attend to by few doctors or nursesIndifferent attitude towards hand hygiene by health workersInadequate supply of soap and towelAbsence of documentary guidelines on hand hygiene and disinfection practicesAbsence of continuous educationUnreported consequences of non-complianceLack of research on hand hygiene and disinfection practicesForgetfulnessSinks are far from where place of (point) of careSkin irritation |
| 2 | Observed risk factors for non-compliance with hand hygiene practice and their possible impact on patient safety | Escalation of sepsisProlonged stay in the hospital by patientsIncreased morbidity and mortalityIncreased infection and disease among health care giversAcquisition of multi-drug resistant microorganismsIncreased cost of treatmentDelayed recovery e.g., delayed wound healingPoor quality careIncrease the risk of infection to both patients and care givers |
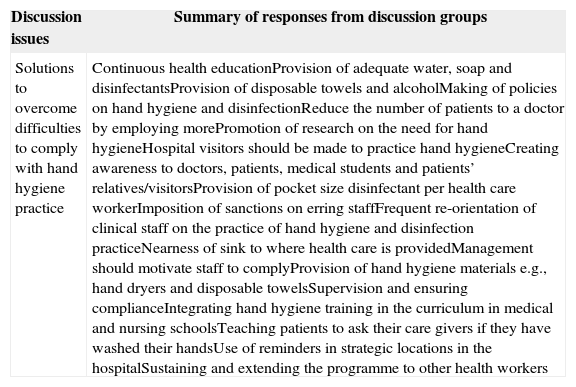
The outcome of focus group discussion on solutions to overcome non-compliance with hand hygiene among doctors and nurses at Federal Teaching Hospital Abakaliki Nigeria.
| Discussion issues | Summary of responses from discussion groups |
|---|---|
| Solutions to overcome difficulties to comply with hand hygiene practice | Continuous health educationProvision of adequate water, soap and disinfectantsProvision of disposable towels and alcoholMaking of policies on hand hygiene and disinfectionReduce the number of patients to a doctor by employing morePromotion of research on the need for hand hygieneHospital visitors should be made to practice hand hygieneCreating awareness to doctors, patients, medical students and patients’ relatives/visitorsProvision of pocket size disinfectant per health care workerImposition of sanctions on erring staffFrequent re-orientation of clinical staff on the practice of hand hygiene and disinfection practiceNearness of sink to where health care is providedManagement should motivate staff to complyProvision of hand hygiene materials e.g., hand dryers and disposable towelsSupervision and ensuring complianceIntegrating hand hygiene training in the curriculum in medical and nursing schoolsTeaching patients to ask their care givers if they have washed their handsUse of reminders in strategic locations in the hospitalSustaining and extending the programme to other health workers |
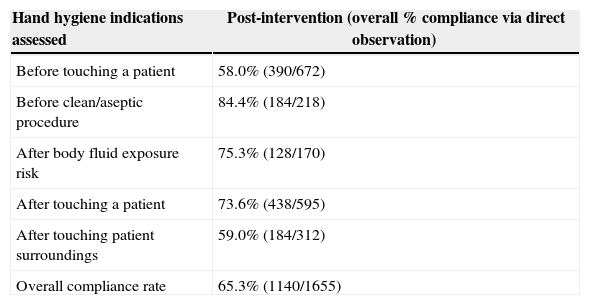
The post-intervention hand hygiene overall compliance rate was 65.3% determined via WHO direct observation technique. The post-intervention hand hygiene indications showed the highest compliance rate ‘after body fluid exposure’ (75.3%) and ‘after touching a patient’ (73.6%) while the least compliance rate was recorded ‘before touching a patient’ (58.0%) (Table 3).
Post-intervention hand hygiene indications and compliance rate among health workers at Federal Teaching Hospital Abakaliki Nigeria.
| Hand hygiene indications assessed | Post-intervention (overall % compliance via direct observation) |
|---|---|
| Before touching a patient | 58.0% (390/672) |
| Before clean/aseptic procedure | 84.4% (184/218) |
| After body fluid exposure risk | 75.3% (128/170) |
| After touching a patient | 73.6% (438/595) |
| After touching patient surroundings | 59.0% (184/312) |
| Overall compliance rate | 65.3% (1140/1655) |
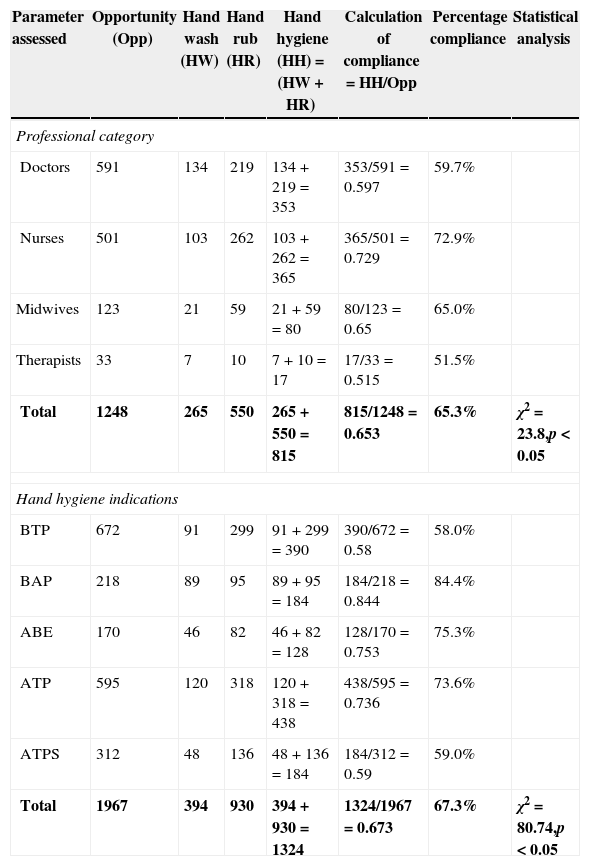
The outcomes of the post-intervention hand hygiene compliance based on professional category and WHO 5 moment hand hygiene indications are summarized in Table 4. The hand hygiene compliance rate was highest among the nurses (72.9%) compared to the doctors (59.7%) and midwives (65%). The difference was statistically significant (χ2=23.8, p<0.05). The hand hygiene indication with the highest compliance rate was “before clean/aseptic procedure” (84.4%) followed by “after body fluid exposure risk” (75.3%). The hand hygiene indications with the least compliance rate were “before touching a patient” (58.0%) and “after touching patient surroundings” (59.0%). The difference in the hand hygiene indication trend was significant (χ2=80.74, p<0.05). In all instances of hand hygiene action, the hand rubbing action was considerably higher than the hand washing action (Table 4). Out of the 815 hand hygiene practices recorded by the health workers in this study 550 (67.5%) was hand rub action (Table 4).
Post-intervention hand hygiene compliance based on professional category and hand hygiene indications determined via direct observation technique.
| Parameter assessed | Opportunity (Opp) | Hand wash (HW) | Hand rub (HR) | Hand hygiene (HH)=(HW+HR) | Calculation of compliance=HH/Opp | Percentage compliance | Statistical analysis |
|---|---|---|---|---|---|---|---|
| Professional category | |||||||
| Doctors | 591 | 134 | 219 | 134+219=353 | 353/591=0.597 | 59.7% | |
| Nurses | 501 | 103 | 262 | 103+262=365 | 365/501=0.729 | 72.9% | |
| Midwives | 123 | 21 | 59 | 21+59=80 | 80/123=0.65 | 65.0% | |
| Therapists | 33 | 7 | 10 | 7+10=17 | 17/33=0.515 | 51.5% | |
| Total | 1248 | 265 | 550 | 265+550=815 | 815/1248=0.653 | 65.3% | χ2=23.8,p<0.05 |
| Hand hygiene indications | |||||||
| BTP | 672 | 91 | 299 | 91+299=390 | 390/672=0.58 | 58.0% | |
| BAP | 218 | 89 | 95 | 89+95=184 | 184/218=0.844 | 84.4% | |
| ABE | 170 | 46 | 82 | 46+82=128 | 128/170=0.753 | 75.3% | |
| ATP | 595 | 120 | 318 | 120+318=438 | 438/595=0.736 | 73.6% | |
| ATPS | 312 | 48 | 136 | 48+136=184 | 184/312=0.59 | 59.0% | |
| Total | 1967 | 394 | 930 | 394+930=1324 | 1324/1967=0.673 | 67.3% | χ2=80.74,p<0.05 |
BTP, before touching a patient; BAP, before clean/aseptic procedure; ABE, after body fluid exposure risk; ATP, after touching a patient; ATPS, after touching patient surroundings.
The outcomes of this study suggest that hand hygiene campaign can be successfully executed in a health facility with improvement in the knowledge and attitudes of health workers on hand hygiene. Although all the doctors and nurses who participated in the training workshops organized in this study were aware of the importance of hand hygiene, they all admitted that compliance was very low even in the hospital. This finding confirms with earlier reports though it is being considered one of the most basic, as well as the most vital infection control measures, it is one of the most neglected practices.5 However unlike most hand hygiene studies from developed countries which cited reason for non-compliance to include lack of time, forgetfulness, hand washing agents detrimental to skin, wearing gloves, and increasing workload,15 the major reason cited for non-compliance in the present investigation was lack of adequate facilities. In most hospitals and clinics in developing countries hand hygiene facilities are grossly inadequate for instance alcohol hand rubs are not available, hand wash basins are poorly accessible and soaps and hand towels are unavailable.1
Apart from regular educational/promotional campaigns, the health workers in this study were of the general consensus that improvement of hand hygiene facilities in the hospitals can encourage compliance especially after an educational intervention. A number of reports have consistently shown that hand hygiene facility improvement enhances compliance among health workers.15–17 Another vital recommendation that can enhance compliance which was made by the health workers in this study is the need for the establishment of a monitoring/supervision mechanism to ensure compliance. There is numerous reported evidence which indicates that the use of hand hygiene monitoring mechanism can improve compliance rate among health workers.18,19 According to Boyce,18 monitoring hand hygiene compliance and providing healthcare workers with feedback regarding their performance are considered integral parts of a successful hand hygiene promotion programme. Interestingly the health workers in this study also were of the opinion that the engagement of more health workers will reduce the high patient care workload, which often contributes to noncompliance with hand hygiene. Some previous studies have indicated that factors such as high intensity of patient care, high patient occupancy, understaffing or low staff to patient ratio, and dense working conditions were among the major barriers to hand hygiene compliance.20–22
In this study, the overall hand hygiene compliance rate was 65.3%. This outcome was comparatively higher than the compliance rates reported by a number of recent similar studies from various developing countries including Saudi Arabia (50.3%),23 Brazil (46.7%),24 Kuwait (33.4%),25 and Indonesia (20%).26 The high compliance rate observed in the present study may be attributed to the positive effect of the interventional programmes which included systematic hand hygiene training using the WHO materials/tools and the use of hand hygiene posters and other reminders in the hospital facilities. This could also be attributed to the support of the hospital authority and the enthusiasm demonstrated by the health workers to comply particularly those who participated in the training programme. Findings from some recent studies have consistently indicated that hand hygiene compliance rates improve significantly following interventional efforts of training and use of reminders in workplace.19,13 These findings suggest that hand hygiene interventions have a great potential to improve health workers hand hygiene compliance and could minimize health care associated infections in hospital facilities.
In the present study, the post-intervention hand hygiene compliance rate was related to professional category and findings indicated that hand hygiene compliance rate was significantly higher among the nurses (72.9%) and the midwives (65%) compared to the doctors (59.7%) (χ2=23.48, p<0.05). Evidence emerging from some recent studies in Saudi Arabia, UK, and Italy showed that hand hygiene compliance rate is consistently higher among the nurses than the doctors.23,27 Clearly there is a need for the development of strategies to improve hand hygiene compliance among the doctors.
Post-intervention hand hygiene compliance rate was related to WHO's 5 moments for hand hygiene (indications) and the highest compliance rate was observed for “before clean/aseptic procedure” (84.4%), followed by “after body fluid exposure risk” (75.3%) with the least rates observed for “before touching a patient” (58.0%). The difference in the trend was statistically significant (χ2=80.74, p<0.05). Our finding is similar to the results reported by Randle and colleagues in Nottingham UK, who observed that compliance before an aseptic task was 100%; after body fluid exposure 93%; and before patient contact 68%.27 However a different situation was reported in a recent similar study in Indonesia, in which Marjadi and McLaws noted that although hand hygiene compliance was poor, it was more likely to be undertaken after patient contact than before-patient contact.26 In another recent study conducted in Germany, Scheithauer and co-workers reported that compliance rates before patient contact or aseptic tasks were significantly lower (17–47%) than after contact with patient, body fluid or patient's surroundings (31–78%).28 These differences in findings may be due to variations in hand hygiene behaviour in each health facility and the type of hand hygiene training that the health workers had undergone.
An important success factor, which might have greatly contributed to the high rate of post-intervention hand hygiene compliance observed in this study, was the introduction of the alcohol-based hand rubs. It is worth noting that out of the 815 hand hygiene practices recorded in this study 550 (67.5%) was hand rub action. There is enough evidence to prove that the introduction of alcohol hand rubs in hospitals improved hand hygiene compliance.19,29 In addition to this, both the Centres for Disease Control and Prevention and World Health Organization Guidelines on Hand Hygiene in Health Care, recommended that alcohol-based hand rub should be used as the preferred means for routine hand antisepsis.8
Limitations and conclusionThis investigation is the first systematic and coordinated hospital-wide campaign on hand hygiene in Nigeria using the WHO's hand hygiene tools and data collection methodology. A main limitation in this study was our inability to get most doctors trained due to their high clinical duties. In spite of our inability to train all the doctors and nurses, the effort made during the intervention including the training of some of the health workers (39 doctors and 163 nurses) the mailing of training materials to 37 doctors, the use of reminders in the workplace and the introduction of alcohol hand rub, provided adequate sensitization of the hand hygiene initiative to all the hospital health workers. We strongly believe the difference in the trained and the observed health workers has not adversely affected the outcome in line with the study objectives. Another limitation was the unavoidable hawthorn effect during the monitoring of hand hygiene compliance and the associated impact of the observer's interpretation of the definitions of the five moments for hand hygiene and the actual situation on the reliability of the data. However despite these limitations, the aim of the study was fully achieved. The results of this study suggest that a hand hygiene sensitization campaign using training, reminders in the workplace and introduction of alcohol hand rub might improve hand hygiene compliance in a low-income health facility. The outcome of this study can guide future efforts to improve hand hygiene and can also serve as a model of the way to perform a systematic assessment of hand hygiene in hospitals of low-income settings.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by the World Health Organization (WHO) Patient Safety Research Small Grants for funding and technical support (WHO Reference: 2009/54485-0; PO: 200152271). We are grateful to Sorin Banica of WHO Patient Safety Programme for providing technical and cooperative support during implementation of the project. The assistance of Mr. C.D.C. Ugwuoru of Medical Microbiology Department of Ebonyi State University Abakaliki during the intervention phase is appreciated. Authors are grateful to all the health workers who participated in this project.