Effective antiretroviral therapy (ART) has increased life expectancy for HIV patients to levels close to that observed for general population. Comorbidities are also increasing, due to ageing of such population. Erectile dysfunction (ED) has been a frequent finding in men living with HIV.
ObjectivesThe goals of the present study were to define the prevalence of ED and associated factors in HIV-infected men, in a referral center of Salvador city, Brazil.
MethodsHIV-infected men ≥18 years of age, receiving care at the AIDS Clinics of Complexo Hospitalar Professor Edgard Santos (C-HUPES), Universidade Federal da Bahia were consecutively included in the study until the estimated sample size (N=134) was reached. Patients filled a structured questionnaire on clinical-epidemiological characteristics, as well as the International Index on Erectile Function to assess ED.
ResultsMost (55%) were black and single (79%), mean age 44.8 years. ED was detected in 29 (21.6%) patients; 86% of ED cases were classified as severe. The only factors associated with ED were low income (p=0.02) and unemployment (p=0.01). No association was found between ED and frequency of comorbidities, age, or ART used by patients.
ConclusionIn a referral center in Salvador city, socio-economic problems were the main factors associated with ED. Psychological impact of poor social conditions should be routinely assessed in patients with ED to implement preventive measures for ED.
According to the World Health Organization (WHO), sexual health includes a combination of positive somatic, emotional, intellectual and social aspects of a sexual being.1 Sexual health results of the linkage of vascular, neurological and endocrine systems: any modification in one of these systems can potentially generate a sexual dysfunction.1–3
Erectile dysfunction (ED) is defined as the inability to have or keep a satisfactory penile erection. The main causes of ED are classified as psychogenic (anxiety, stress, depression) or organic (vascular, neurological, hormonal, and tissue problems). Any cause of hypogonadism can trigger ED, including hypothalamic-pituitary tumors, hyperprolactinemia, and primary or secondary hypogonadism.1–7
Hypogonadism is one of most frequent endocrine dysfunction in HIV-infected men. Usually, low levels of testosterone leads to decreased sexual desire and ED. In addition, psychological (especially depression) or neurological (infection, dementia) problems often cause ED.6–10
In Brazil, there is scarce evidence on the frequency and causes of ED in men living with HIV-Aids. We aimed to determine the prevalence of ED in HIV-infected men, in Salvador city, Brazil, as well as the associated factors.
Study design, patients and settings: A cross-sectional study was conducted at an Aids referral center, in Salvador, Brazil, from January to August, 2015. All male patients, aged 18 years or older, who attended the Aids clinic during the study period were invited to participate. Patients with a cognitive deficit and those with neurological problems were excluded. Patients were consecutively included, until the required sample size was reached. Sample size was defined based on an estimated prevalence of 18%, for a population of 1500 eligible male subjects under follow-up at the service. To guarantee a power of 80% and a confidence interval of 95%, the required sample size was 134 patients.
Data collection: the used instruments were a questionnaire on clinical and socio-demographic characteristics and the International Index on Erectile Function, a self-administered questionnaire on erectile function, which was previously validated and adapted to Brazil. It includes 15 multiple options questions to evaluate erectile function, sexual relationship, orgasmic function, sexual desire, and overall level of satisfaction with sexual life. According to the obtained scores ED was classified as absent, mild, moderate, or severe. Questionnaires were filled in by patients, under supervision of a trained investigator to solve doubts or to clarify any points of the instrument.
Statistical analysis: frequencies and proportions were used to describe the main categorical variables. Continuous variables were described as mean and standard deviation or median and interquartile range. Associations between categorical variables were assessed by use of chi-square test. We used 95% confidence intervals and set a p-value<0.05 for significance. Associations between variables were assessed through univariate and multivariate analyses. The SPSS statistical package software, version 20 was used to perform all analyses. The project was approved by institutional ethics review committee (number 1.035.816, on 26 April, 2015).
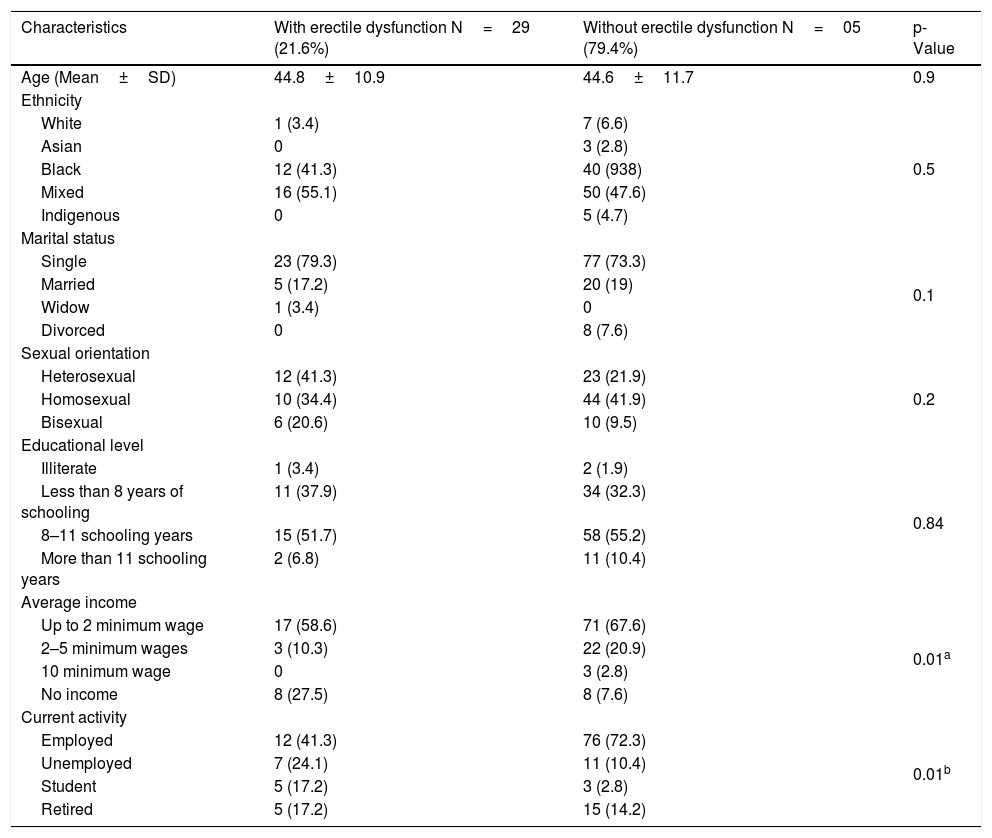
A total of 134 men were included in the study, most (55%) black and single (79%). The main characteristics of study sample are described in Table 1.
Sociodemographic characteristics of the study sample according to the presence of erectile dysfunction.
| Characteristics | With erectile dysfunction N=29 (21.6%) | Without erectile dysfunction N=05 (79.4%) | p-Value |
|---|---|---|---|
| Age (Mean±SD) | 44.8±10.9 | 44.6±11.7 | 0.9 |
| Ethnicity | |||
| White | 1 (3.4) | 7 (6.6) | 0.5 |
| Asian | 0 | 3 (2.8) | |
| Black | 12 (41.3) | 40 (938) | |
| Mixed | 16 (55.1) | 50 (47.6) | |
| Indigenous | 0 | 5 (4.7) | |
| Marital status | |||
| Single | 23 (79.3) | 77 (73.3) | 0.1 |
| Married | 5 (17.2) | 20 (19) | |
| Widow | 1 (3.4) | 0 | |
| Divorced | 0 | 8 (7.6) | |
| Sexual orientation | |||
| Heterosexual | 12 (41.3) | 23 (21.9) | 0.2 |
| Homosexual | 10 (34.4) | 44 (41.9) | |
| Bisexual | 6 (20.6) | 10 (9.5) | |
| Educational level | |||
| Illiterate | 1 (3.4) | 2 (1.9) | 0.84 |
| Less than 8 years of schooling | 11 (37.9) | 34 (32.3) | |
| 8–11 schooling years | 15 (51.7) | 58 (55.2) | |
| More than 11 schooling years | 2 (6.8) | 11 (10.4) | |
| Average income | |||
| Up to 2 minimum wage | 17 (58.6) | 71 (67.6) | 0.01a |
| 2–5 minimum wages | 3 (10.3) | 22 (20.9) | |
| 10 minimum wage | 0 | 3 (2.8) | |
| No income | 8 (27.5) | 8 (7.6) | |
| Current activity | |||
| Employed | 12 (41.3) | 76 (72.3) | 0.01b |
| Unemployed | 7 (24.1) | 11 (10.4) | |
| Student | 5 (17.2) | 3 (2.8) | |
| Retired | 5 (17.2) | 15 (14.2) | |
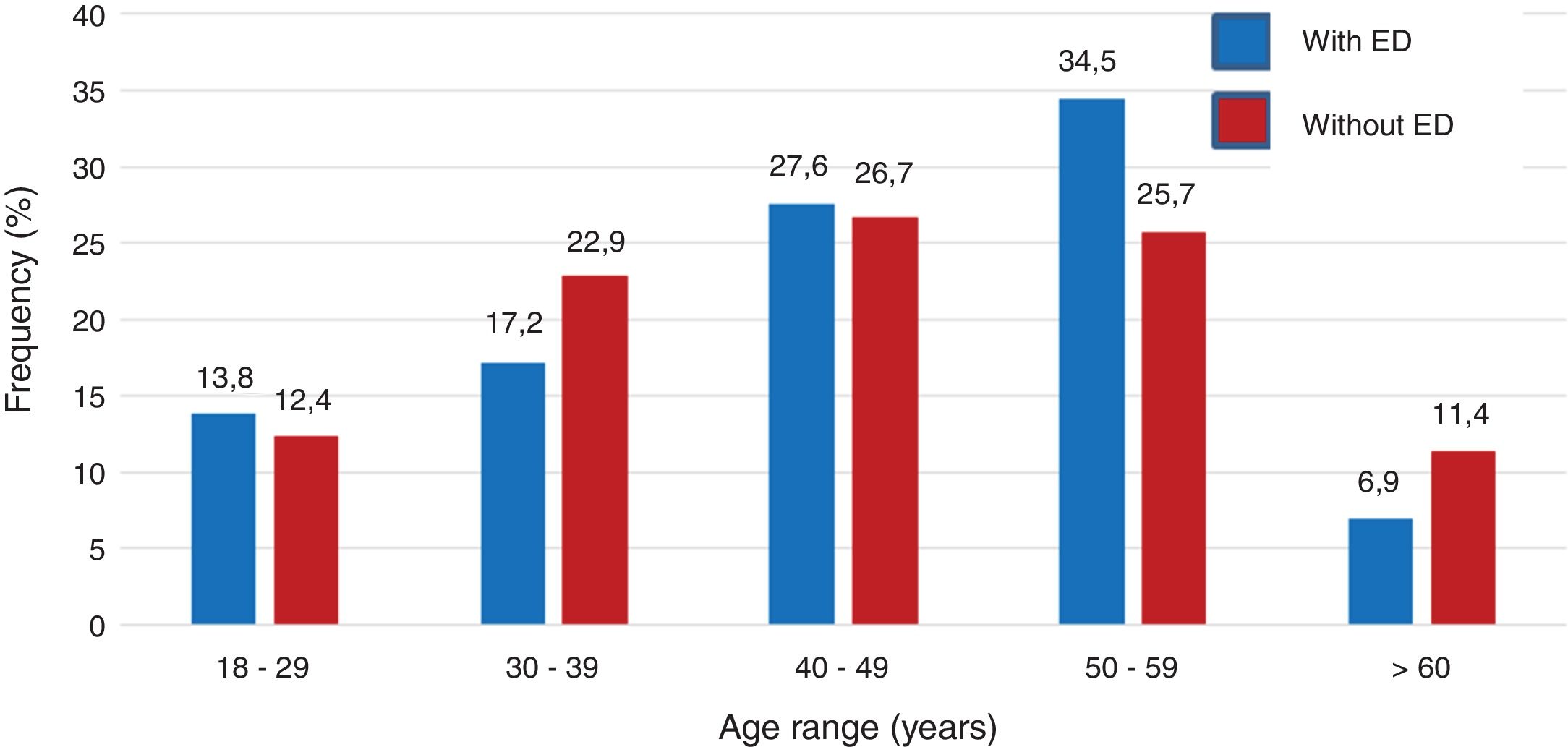
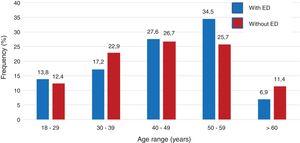
The frequency of ED was 21.6% (29 patients) which was classified as severe in 86.2% of them. ED was significantly associated with unemployment (p=0.01) and no income (p=0.02). Mean age was similar for patients presenting with ED (44.8±10.9 years) or not (44.6±11.7 years), as shown in Fig. 1.
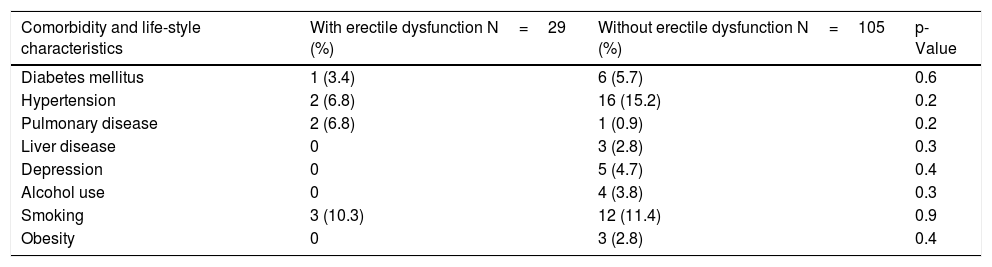
All but five patients were on antiretroviral therapy, two did not present ED, while three had severe ED. The majority used a non-nucleoside based (43%) or protease inhibitor-based regimens (32%), and most (76.9%) used no additional medications other than antiretroviral drugs. Among the 31 patients reporting use of medications other than ARV, 10 (32%) were on anti-hypertensive drugs. The mean time since HIV diagnosis was similar for patients with and without ED. Table 2 shows the frequency of ED according to the mean duration of HIV infection and to patients´ life style.
Frequency of comorbidities and life style characteristics of HIV patients according to the presence of erectile dysfunction.
| Comorbidity and life-style characteristics | With erectile dysfunction N=29 (%) | Without erectile dysfunction N=105 (%) | p-Value |
|---|---|---|---|
| Diabetes mellitus | 1 (3.4) | 6 (5.7) | 0.6 |
| Hypertension | 2 (6.8) | 16 (15.2) | 0.2 |
| Pulmonary disease | 2 (6.8) | 1 (0.9) | 0.2 |
| Liver disease | 0 | 3 (2.8) | 0.3 |
| Depression | 0 | 5 (4.7) | 0.4 |
| Alcohol use | 0 | 4 (3.8) | 0.3 |
| Smoking | 3 (10.3) | 12 (11.4) | 0.9 |
| Obesity | 0 | 3 (2.8) | 0.4 |
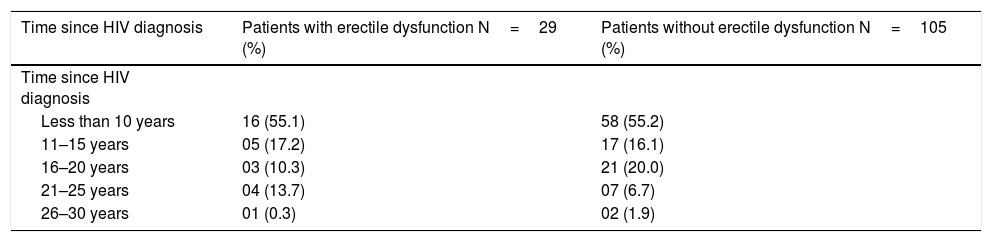
The most frequently detected comorbidity was arterial hypertension, which affected 18 (13.4%) patients. There was no difference in the frequency of diabetes, arterial hypertension, chronic pulmonary disease, depression, alcohol use, smoking, and viral hepatitis C among patients with or without ED. Table 2 summarizes these findings. There was no association between time since HIV diagnosis and frequency of ED (Table 3)
Frequency of erectile dysfunction in HIV patients according to time since diagnosis.
| Time since HIV diagnosis | Patients with erectile dysfunction N=29 (%) | Patients without erectile dysfunction N=105 (%) |
|---|---|---|
| Time since HIV diagnosis | ||
| Less than 10 years | 16 (55.1) | 58 (55.2) |
| 11–15 years | 05 (17.2) | 17 (16.1) |
| 16–20 years | 03 (10.3) | 21 (20.0) |
| 21–25 years | 04 (13.7) | 07 (6.7) |
| 26–30 years | 01 (0.3) | 02 (1.9) |
p>0.05 for all comparisons.
ED is highly prevalent in HIV-infected patients having a negative impact in their quality of life.11,12 ED prevalence was 21.6% among HIV-infected patients receiving care in a referral center in Salvador, Brazil, similar to that found in several studies. The main factors associated to ED in this study were unemployment and absence of income. In a large study, involving 1340 patients, Hart et al. found an ED prevalence of 21%, although the patients had a higher frequency of comorbidities, like diabetes (17%) and arterial hypertension (69%), than in the present study. Presence of comorbidities was closely related to ED prevalence, in contrast with our results where psychological problems were a more likely cause of ED than organic conditions.
The orgasmic function was null for all patients with ED, considering ejaculation with or without orgasm. In contrast, the evaluation of sexual desire was moderate/high for all patients with moderate ED and for 64% of those classified as presenting severe ED. The level of satisfaction with sexual life was moderate/high (>75%) for patients with ED. Most (80%) patients with ED reported satisfaction with their sexual partner. A previous report detected that men with Aids need more time and stimulation to develop a sexual response, which would require a collaborative sexual partner and explain the high levels of satisfaction detected in our work.2
Although some previous reports showed an association between older age and increased prevalence of ED, that was not detected in this study. The study sample was relatively young (mean age 44 years) and reflects the epidemiological HIV picture in Salvador, where only 30% of patients are older than 50 years. However, a study conducted by Shindel et al. shows similar results in a study sample with a mean age of 42 years, and a prevalence of diabetes (3.2%) or hypertension (26%) similar to that found in the present study. The main discrepancy was the association between ED and older age, as well as between the severity of ED and increased age. They also included HIV-negative subjects in the study.
The prevalence of ED in our study was lower than that detected in several studies.13–15 This probably reflects the characteristics of the study samples and geographic regions. On the other hand, our findings are similar to those obtained by Claramonte et al. in Africa. Salvador is the Brazilian city with the largest proportion of African descendants in Brazil and is considered the largest black city outside Africa. This could explain the similarity between the results of this study and those reported by Claramonte et al. The only detected risk factor for ED in our study was low income and unemployment. Such findings suggest that psychosocial problems play a major role in the development of ED in our patients. Although we did not perform any specific psychological evaluation, it would be expected to find depression and anxiety among these patients. The low prevalence of comorbidities indicates the absence of associations between organic problems and ED in this study. The relatively low proportion of older patients also reinforces this hypothesis.
One important finding in our study relates to the severity of ED dysfunction: only 13.7% of patients had a mild presentation of ED, while the remaining 86.3% presented severe ED. This contrasts with previous reports that identified higher proportion of ED in similar populations, but usually with fewer patients presenting the most severe presentations. In addition, our study detected a lower overall prevalence of ED than that observed for general population. However, the use of different patient group, with distinct epidemiological, social and clinical characteristics make it difficult to compare the available reports.
There was no association between ED and sexual orientation, similarly to that observed by Catalan et al. in a previous report. In addition, there was no association between antiretroviral regimens used by patients and ED. Although some reports show an association between specific ARV drugs and ED, the available evidence on that do not permit any conclusion regarding causality, as most studies have not controlled for other risk factors for ED.17–20
The main limitation of our study is the use of a single center, which may limit generalization of our results. However, the study center is the second largest referral center for Aids care in Bahia state, where about one third of all patients are followed, which minimizes the potential impact of selection bias. This was the first study on ED in HIV patients in Northeastern Brazil, and provides information on risk factors and magnitude of ED in our setting. The detection of socio-economic factors as the main driver of ED open room to psychological interventions that could mitigate this important problem of HIV-infected patients. Larger, prospective studies are necessary to define the magnitude of ED among HIV patients and to define appropriate tools for its management.