The hepatitis C virus and human immunodeficiency virus share the same transmission routes, which makes co-infection an unfavorable condition for the natural history of both viral diseases. In this context, it should be highlighted that the knowledge of the extent of co-infection and associated risk factors is a vital tool for prevention and control over infectious diseases. The aim of this study was to review the literature, seeking to examine the prevalence of human immunodeficiency virus/hepatitis C virus co-infection reported in studies conducted in Brazil, and identify the main risk factors associated with co-infection.
The electronic search was conducted in the Medline, Lilacs and SciELO databases. The following keywords were used: human immunodeficiency virus and Hepatitis C or hepatitis C virus and Brazil. The search led to 376 articles, of which 69 were selected for data extraction. We excluded animal studies, reports or case series, review articles, letters to the editor, other types of hepatitis and those studies in which co-infected patients were intentionally selected for comparison to single infected individuals. As a result, 40 articles were reviewed. The majority of the population in these studies was male (71%) and young adults, with a mean age of 26.7 years. The prevalence of hepatitis C virus co-infection among individuals living with human immunodeficiency virus in the studies conducted in Brazil ranged from 3.3% (serum samples) to 82.4% (drug users), with an average of 20.3%. The findings reveal that the prevalence of human immunodeficiency virus/hepatitis C virus co-infection is highly variable, depending on the characteristics of the study population. Risk factors associated with human immunodeficiency virus/hepatitis C virus co-infection were injection drug use and blood transfusion.
The human immunodeficiency virus (HIV) and hepatitis C virus (HCV) share the same transmission routes, which causes high rates of co-infection, and is a severe clinical condition for both viral diseases.1
HIV is most commonly spread by sexual contact with an infected partner, through contact with infected blood, accidental sticks or vertical transmission.2 HCV transmission occurs mostly through infected blood and blood products, but sexual, accidental and vertical transmission has been also evidenced.3
The HIV/HCV co-infection is a significant risk factor for liver fibrosis, since HIV seropositivity and low CD4+ count seems to accelerate this process.4,5 The progression of fibrosis in HCV/HIV co-infected patients occurs with high frequency during an average estimated time of three years.6 Similarly, HCV infection has been shown to be associated with faster progression to acquired immunodeficiency syndrome (AIDS).7
In Brazil, according to the Epidemiological Bulletin on Viral Hepatitis (2011), co-infection rates reach a percentage of 11.4% in HIV-seropositive patients.8 This percentage shows regional variation being dependent on the characteristics of the study population. However, this estimate is based on cases reported by the Information System for Notifiable Diseases (SINAN), and may not be representative of the general population, since only AIDS cases are reported, and there is a relative delay between case detection and publishing of reports.8
Therefore, this study is intended to review this issue, seeking to examine the prevalence of HIV/HCV co-infection encountered in studies conducted in Brazil, and identify the main risk factors for this co-infection.
MethodsThis is a narrative review on HIV/HCV co-infection in Brazil. The electronic search was conducted in the Medline, Lilacs and SciELO databases. The following keywords were used: HIV [MeSH] and HCV [textline] or Hepatitis C [MeSH] and Brazil [textline] in English and the corresponding words in Portuguese. The references of the selected articles were examined for possible inclusion of additional articles.
We included original scientific articles that presented data on the prevalence of HIV/HCV co-infection in different population groups, of both sexes, conducted in Brazil.
We excluded studies that addressed animal studies, reports or case series, review articles, letters to the editor, other types of hepatitis and those in which co-infected patients were intentionally selected for comparison to single-infected patients.
Duplicate articles were excluded. We started reading the titles, then the abstracts, and later the full texts. Exclusion criteria were applied in all stages, always by consensus between two readers.
The selected articles were analyzed to characterize the study: year of publication, location and period of data collection, type of study, study population and sampling (number of investigated subjects, mean age and gender of participants), prevalence rates of HIV, HCV and HIV/HCV co-infection, and risk factors associated with the presence of co-infection.
HIV-infected individuals were considered those who had positive anti-HIV serology. HCV-infected individuals were considered those who had positive anti-HCV serology. The co-infection rates were taken directly from the articles, and when this information was not provided, they were calculated by dividing the number of individuals who had serological markers for HIV and HCV by the total number of participants in the study.
To calculate the mean age and the prevalence of HIV/HCV co-infection, we used descriptive statistics to find the weighted mean, taking into account the sample size of each study.
ResultsThe search led to 376 articles, of which 69 were selected for data extraction. After applying the exclusion criteria, 40 articles remained (Fig. 1). This study period covered articles published between April 1999 and June 2012.
Of the 40 articles analyzed, 36 were cross-sectional studies (one multisite), three cohort studies (two historical cohorts) and a descriptive study.
In total, we studied 48,791 subjects; of these, 28,819 (59.0%) were pregnant women, 13,483 (27.6%) were subjects or blood samples from HIV-infected patients, 2780 (5.7%) were individuals under restriction of freedom, 550 (1.1%) drug users, 3159 (6.6%) individuals with other characteristics, such as alcoholics, homeless people, garbage collectors, or patients attending various outpatient clinics.
Demographic characteristics available in the selected studies showed that the majority of participants were men (71%).9–34 Of the 40 selected articles, men predominated in the samples of 26, with only one35 showing a predominance of women. The samples of seven studies comprised only women.35–41 The mean age was 26.7 years among the papers that presented this information.9–18,20–23,25,26,28,30–37,40–43 Eight of the selected papers had no data regarding gender and age of the participants.38,39,44–49
In 20 articles,9–12,14–17,19–21,23,25,26,34,43–47 the study population consisted entirely of HIV-infected individuals or serum samples, and showed HIV/HCV co-infection rates ranging from 3.3%11 to 54.7%47 (Table 1), with an average of 19.5%. Including the studies with pregnant women36,40 and injection drug users,29 whose participants were all infected with HIV as well, the weighted mean of HIV/HCV co-infection was 20.3% among 13,894 participants.
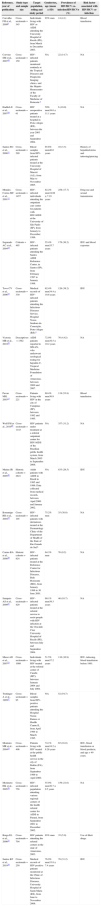
Description of the studies on HIV/HCV co-infection among HIV-infected patients.
| Reference, year of publication | Study type and sample size | Target population, setting and study period | Gender/sex, age (mean±SD) | Prevalence of HIV/HCV co-infectionHIV/HCVn (%) | Risk factor associated with HIV/HCV co-infection |
|---|---|---|---|---|---|
| Carvalho FH et al., 20099 | Cross-sectionaln=345 | Individuals living with HIV or AIDS attending the University Hospital of Recife (PE), from March to December 2003. | 65% men | 14 (4.1) | Blood transfusion |
| Corvino SM et al., 200744 | Cross-sectionaln=150 | HIV-infected patients monitored routinely at the Tropical Diseases and Diagnostic Imaging clinics, and the Hepato-Hemocentro of the Faculty of Medicine of Botucatu.a | NA | 22 (14.7) | NA |
| Hadlich E et al., 200710 | Cross-sectionaln=61 | HIV seropositive patients treated at a hospital in Porto Alegre (RS), between the year 2003 and September 2004. | 59% men38.0±11.1 years | 6 (10.0) | NA |
| Santos EO et al., 200811 | Cross-sectionaln=299 | Blood samples from HIV- infected patients treated at the University Hospital of Maceió (AL), from May to November 2005. | 65.6% men40.0 years | 10 (3.3) | History of hepatitis/icterus and tattooing/piercing |
| Mendes-Correa MC et al., 200112 | Cross-sectionaln=1457 | HIV-infected individuals attending the outpatient care center for patients with HIV/AIDS at the University of São Paulo (SP), from January to December 1996. | 82.2% men34.08±7.19 years | 258 (17.7) | Drug use and sexual transmission |
| Segurado AC et al., 200414 | Cohortn=495 | HIV-infected patients attending the Santos AIDS Reference Center, in Santos (SP), from February 1997 to January 1998. | 55.4% men35.7 years | 179 (36.2) | IDU and blood exposure |
| Tovo CV et al., 200615 | Cross-sectionaln=330 | Medical records of HIV-infected patients attending the Infectious Diseases Service, Hospital Nossa Senhora da Conceição, Porto Alegre (RS).a | 62.4% men34.4±10.6 years | 126 (38.2) | IDU |
| Victoria MB et al., 201016 | Descriptiven=1582 | AIDS patients reported to SINAN, who underwent serological testing for hepatitis C, Tropical Medicine Foundation of Amazonas, between 2000 and 2007. | 72.9% men38.5±10.2 years | 70 (4.42) | NA |
| Pavan MH, 200317 | Cross-sectionaln=221 | Patients living with HIV in the city of Campinas (SP), between 1992 and 1995. | 69.4% men30.8 years | 119 (53.8) | Blood transfusion |
| Wolf FH et al., 201045 | Cross-sectionaln=1143 | HIV patients under treatment at a referral outpatient center for HIV/AIDS of the Brazilian public health system, from March 2005 to September 2006. | NA | 357 (31.2) | NA |
| Marins JR et al., 200546 | Historic cohortn=2821 | Adult patients with AIDS in Brazil in 1995 and 1996. Data collected from medical records, between April 2000 and January 2002. | NA | 833 (29.5) | IDU |
| Bonamigo RR et al., 200419 | Cross-sectionaln=105 | HIV-infected patients with dermatoses treated at the Dermatology Clinic of the Department of Health of the State of Rio Grande do Sul.a | 75.2% men | 35 (38.0) | NA |
| Carmo RA et al., 200820 | Historic cohortn=824 | HIV-infected patients treated at the Reference Center for Infectious Diseases, Belo Horizonte (MG), from January 1996 to 30 June 2001. | 64.3% men | 76 (9.2) | NA |
| Sampaio AS et al., 200921 | Cross-sectionaln=429 | HIV-infected patients treated at the referral service to assist people with HIV infection at the Oswaldo Cruz University Hospital of Recife (PE), between July and September 2004. | 60.1% men39.3 years | 46 (10.7) | NA |
| Mussi AD et al., 200723 | Cross-sectionaln=1008 | Individuals living with HIV treated at the referral center of Cuiabá (MT), between January 2004 and July 2004. | 51.5% men37.2 years | 110 (10.9) | IDU, tattooing, blood transfusion before 1991. |
| Treitinger A et al., 199947 | Cross-sectionaln=95 | Blood samples from HIV-positive patients attending the Hospital Nereu Ramos or Health Centre II, from April 1994 to March 1995. | NA | 52 (54.7) | |
| Monteiro MR et al., 200425 | Cross-sectionaln=406 | Patients living with HIV treated at the public health service in the city of Belém (PA), from September 1999 to April 2000. | 74.1% men34.2±8.26 years | 65 (16.0) | IDU, blood transfusion or blood products, and age>49 years. |
| Morimoto HK et al., 200526 | Cross-sectionaln=758 | HIV-infected population attending various regional centers of the health referral center for AIDS in Paraná, from September 2001 to December 2002. | 55.9% men36.7±9.5 years | 159 (21.0) | NA |
| Braga EL et al., 200627 | Cross-sectionaln=704 | HIV patients attending the referral centers in the state of Amazonas, 2003. | 65% men | 35 (5.0) | Use of illicit drugs. |
| Santos KF et al., 201034 | Cross-sectionaln=250 | Medical records of HIV-positive patients monitored at the Clinic of Infectious Diseases, University Hospital of Santa Maria (RS), from June to November 2006. | 76.9% men33.8±7.4 years | 78 (31.2) | IDU |
NA, not assessed; IDU, injection drug user; HIV, human immunodeficiency virus; HCV, hepatitis C virus; SD, standard deviation; n, sample size.
Five papers studied pregnant women, aiming to determine the prevalence of certain infectious diseases and/or verify the risk of vertical transmission.36–40 In these studies, the prevalence of HIV/HCV co-infection ranged from 0.0000737 to 27.6%39 (Table 2).
Description of studies on HIV/HCV co-infection among pregnant women.
| Reference, year of publication | Study type and sample size | Target population, setting and study period | Age (mean±SD) | Prevalencen (%) | ||
|---|---|---|---|---|---|---|
| HIV | HCV | HIV/HCV | ||||
| Tornatore M et al., 201236 | Cross-sectionaln=130 | HIV-infected pregnant women attending the HIV/AIDS center at the University Hospital of the Federal University of Rio Grande do Sul, from July 2006 to December 2008. | 26.2±5.69 years | 130 (100.0) | 14 (10.8) | 14 (10.8) |
| Costa ZB et al., 200937 | Cross-sectionaln=28,561 | Pregnant women attending antenatal care of the public health system in Goiânia (GO), between 2004 and 2005. | 23.9±5.6 years | 38 (0.13) | 65 (0.22) | 2 (0.00007) |
| Gardenal RV et al., 201138 | Cross-sectionaln=23 | HCV-positive pregnant women enrolled in the System Information Program for Humanization of Prenatal and Birth (SISPRENATAL) used by the Health Secretary of the municipality of Campo Grande (MS), between 2002 and 2005. | NA | 2 (8.7) | 23 (100.0) | 2 (8.7) |
| Peixoto MF et al., 200439 | Cross-sectionaln=29 | HCV-positive pregnant women attending antenatal care of the Hospital Nossa Senhora da Conceição of Porto Alegre (RS), from August 1998 to November 1999. | NA | 8 (27.6) | 29 (100.0) | 8 (27.6) |
| Dal Fabbro MM et al., 200540 | Cross-sectionaln=76 | HIV-infected pregnant women treated at the Reference Department in Campo Grande (MS), from May 1996 to October 2001. | 24.0 years | 76 (100.0) | 11 (14.5) | 11 (14.5) |
NA, not assessed; HIV, human immunodeficiency virus; HCV, hepatitis C virus; SD, standard deviation; n, sample size.
Among drug users18,29,35 the prevalence of HIV/HCV co-infection ranged from 15.1%35 to 82.4%29 (Table 3). Five studies assessing individuals in restraint of freedom24,28,32,33,48 found a prevalence of co-infection ranging from 1.6%28 to 7.1%32 (Table 4).
Description of studies on HIV/HCV co-infection among drug users.
| Reference, year of publication | Study type and sample size | Target population, setting and study period | Gender/sex, age (mean±SD) | Prevalencen (%) | Risk factor associated with HIV/HCV co-infection | ||
|---|---|---|---|---|---|---|---|
| HIV | HCV | HIV/HCV | |||||
| Zocratto KB, 200618 | Cross-sectional multisite studyn=272 | Injecting drug users in 5 Brazilian cities selected by the AjUDE Brasil-I project, starting 1998. | 82.7% men29.25±8.4 years | 25 (9.2) | 28 (10.3) | 116 (42.6) | IDU, male homosexual intercourse |
| von Diemen L et al., 201035 | Cross-sectionaln=73 | Female crack users in Porto Alegre (RS), from August to December 2004. | 100% women28.1±7.6 years | 27 (37.0) | 18 (27.7)a | 11 (15.1) | NA |
| Marchesini AM et al., 200729 | Cross-sectionaln=205 | Injection drug users infected with HIV under treatment at the STD/AIDS municipal health department in São Paulo (SP), from January to November 2003. | 81% men39±6.1 years | 205 (100.0) | 169 (82.4) | 169 (82.4) | NA |
HIV, human immunodeficiency virus; HCV, hepatitis C virus; NA, not assessed; SD, standard deviation; n, sample size; IDU, injection drug users; STD, sexually transmitted diseases; AIDS, acquired immunodeficiency syndrome.
Description of studies on HIV/HCV co-infection among individuals in restraint of freedom.
| Reference, year of publication | Study type and sample size | Target population, setting and study period | Gender/sex, age (mean±SD) | Prevalence (%) | ||
|---|---|---|---|---|---|---|
| HIV | HCV | HIV/HCV | ||||
| Pompilio MA et al., 201124 | Cross-sectionaln=686 | Prisoners of Mato Grosso do Sul State, 2009. | 64.6% men | 34 (5.0) | 33 (4.8) | 11 (1.6) |
| Gabe C and Lara GM, 200848 | Cross-sectionaln=76 | Serum samples of female prison inmates in Rio Grande do Sul, stored in the Santa Helena Laboratory, Porto Alegre (RS).a | NA | 7 (9.2) | 11 (14.5) | 2 (2.6) |
| Catalan-Soares BC et al., 200028 | Cross-sectionaln=63 | Prisoners of Manhuaçu (MG).a | 100% men30.2 years | 2 (3.2) | 4 (6.3) | 1 (1.6) |
| Guimaraes T et al., 200132 | Cross-sectionaln=756 | Blood samples of inmates at the House of Detention in São Paulo (SP), between December 1993 and January 1994. | 100% men30.2 years | 105 (13.7) | 310 (41.0) | 54 (7.1) |
| Zanetta DM et al., 199933 | Cross-sectionaln=1199 | Teenagers from two FEBEM centers in São Paulo (SP), from December 1994 to April 1995. | 92% men16.2 years | 38 (3.2) | 21 (1.8) | 21 (1.8) |
HIV, human immunodeficiency virus; HCV, hepatitis C virus; NA, not assessed; SD, standard deviation; n, sample size; FEBEM, Portuguese acronym for the State Foundation for the Well-Being of Minors.
The HIV/HCV co-infection rates ranged from 0.6%30 among homeless people who used hostels to 82.4%29 among injection drug users. Studies that have determined the prevalence of HIV/HCV co-infection in other populations are presented in Table 5.
Description of studies on HIV/HCV co-infection among different population groups.
| Reference, year of publication | Study type and sample size | Target population, setting and study period | Gender/sex, age (mean±SD) | Prevalence (%) | Risk factor associated with HIV/HCV co-infection | ||
|---|---|---|---|---|---|---|---|
| HIV | HCV | HIV/HCV | |||||
| Oliveira ML et al., 200913 | Cross-sectionaln=131 | Alcoholic patients in a consecutive order, between March 1998 and November 1999. | 90.8% men44.3±10.8 years | 4 (3.0) | 5 (4.2) | 2 (1.5) | NA |
| Pereira GA et al., 200642 | Cross-sectionaln=592 | People attending a Center for anonymous testing and counseling for HIV in Goiânia (GO).a | 65% women | 19 (3.2) | 15 (2.5) | 14 (2.4) | IDU |
| Reis NR et al., 201122 | Cross-sectionaln=402 | Patients under treatment for tuberculosis (TB) at the referral hospital for infectious diseases in Goiânia (GO), from April 2008 to March 2010. | 71.9% men44.1 years | 111 (27.6) | 30 (7.5) | 20 (5.0) | Age, IDU and HIV infection |
| Portelinha Filho AM et al., 200949 | Cross-sectionaln=1.228 | Individuals attending the Clinic of Infectious Diseases at the Dr. Dominic Leonardo Cerávolo Regional University Hospital in Presidente Prudente (SP), from January 2000 to December 2006. | NA | 303 (24.7) | 173 (14.0) | 49 (4.0) | NA |
| Berra JAP et al., 200641 | Cross-sectionaln=225 | Serum samples from patients with infectious diseases at the Rio Claro Regional Laboratory of the Adolfo Lutz Institute (SP), between March 2003 and June 2004. | 100% women | 8 (3.6) | 17 (7.5) | 2 (0.9) | NA |
| Brito VO et al., 200730 | Cross-sectionaln=330 | Homeless people who use hostels in Sao Paulo (SP), from 2002 to 2003. | 80.9% men40.2 years | 6 (1.8) | 28 (8.5) | 2 (0.6) | NA |
| Rozman MA et al., 200831 | Cross-sectionaln=251 | Seroepidemiological survey of autonomous garbage collectors in the city of Santos (SP), June 2005. | 84.9% men42.4 years | 22 (8.9) | 31 (12.4) | 7 (2.8) | NA |
NA, not assessed; HIV, human immunodeficiency virus; HCV, hepatitis C virus; SD, standard deviation; n, sample size; IDU, injection drug user.
Out of the 40 papers reviewed only 14 reported data on risk factors associated with HIV/HCV co-infection, and these highlighted the injection drug use as the main transmission mechanism,12,14,15,18,22,23,25,34,42,46 followed by blood transfusion.9,17,23,25 Behavioral risks such as tattooing,11,23 piercing11 and exposure to infected blood,14 although to a lesser extent, as well as sexual exposure,12 homosexuality,18 and older age22,25 were positively associated with the presence of HIV/HCV co-infection.
DiscussionThis review comprised 40 studies that surveyed a total of 48,791 Brazilians, including pregnant women, subjects or blood samples from HIV-infected patients, individuals under restriction of freedom, drug users, individuals with other characteristics, such as alcoholics, homeless people, garbage collectors, or patients attending various outpatient clinics. Due to this regional and population diversity, the prevalence of HIV/HCV co-infection had great amplitude. This variation is explained by the exposure to different risk factors for co-infection.2
Thus, we chose to group the participants with similar characteristics, creating subgroups to analyze the seroprevalence rates of HIV/HCV co-infection.
Of the 20 studies that had determined the prevalence of HCV co-infection among individuals living with HIV, the average co-infection rate was 19.5%, which is higher than the rate of 11.8% published by the Ministry of Health in the last Epidemiological Bulletin of Viral Hepatitis.8 This can be attributed to the fact that this estimate is based on cases reported by the SINAN, and may not be representative of the general population, since only AIDS cases are reported and there is a delay between case detection and publishing of reports.8
The HIV/HCV co-infection rates among individuals in restraint of freedom are higher than in the general population. Containment is considered a risk factor due to crowding into small enclosures, promiscuity and rape, illicit drug use, and sharing of personal hygiene objects. These factors create favorable conditions for infection with HIV, HCV and co-infection.50
According to the demographic characteristics of the participants in the different studies, 71% were men, which is in accordance with the national and international data showing that men are the most affected group by HIV, HCV and, consequently, co-infection.8,51,52 The mean age was 26.7 years, i.e., young adults, unlike some studies that showed older age populations.7,15 This discrepancy can be explained by the inclusion of teenagers33 and pregnant women,36–40 e.g., women of childbearing age, and therefore, younger, coupled with the fact that several studies did not provide the age of the study population,19,38,39,44–49 which may have underestimated this figure.19,38,39,44–49 It should be emphasized, however, that the predominance of men and young population represents the sample described in the studies, and not the co-infection cases, since these data were not available. Nevertheless, one can assume that there was a demographic similarity among the detected co-infection cases.
The articles that addressed studies with pregnant women showed a great variation of co-infection rates, ranging between 0.00007 and 27.6%.36–40 This variation can be explained by the fact that only Costa et al.37 conducted research with large numbers of pregnant women to determine the prevalence of infection with HIV, HCV and co-infection, reaching rate values of 0.13%, 0.22% and 0.00007%, respectively. These findings diverge from some different studies included in the review, whose main objective was to verify the vertical transmission by studying subgroups of HIV- and HCV-seropositive subjects or both, thereby increasing the rates found. In Brazil, the prevalence of HIV infection in pregnant women is estimated to be 0.41%.53 There is no national estimate of the prevalence of HCV infection among pregnant women, but the rate of HCV vertical transmission is 0.3%.8
Injection drug use is a major mode of HIV and HCV transmission.54 In all studies included in this review, injection drug users had high rates of co-infection. This high rate of transmission can be attributed to the sharing of drug preparation equipment, facilitating HIV and HCV transmission through the exposure to contaminated blood.55 This pathway is the main route of transmission for HCV. Drug injection practices also predispose to other risky behaviors such as promiscuity, lack of condom use, homosexual intercourse, among others.56
Different HIV/HCV co-infection rates were observed among the study population that participated in the studies included in this review. The heterogeneity of the studies did neither allow summarizing the prevalence of coinfection in each subgroup nor an overall prevalence. Therefore, we opted to calculate just the weighted average of HIV/HCV co-infection rate in people living with HIV. The variation of coinfection rates found in this study is justified by the peculiar characteristics of the diverse population groups that are exposed to different risk factors.
The studies that reported data on risk factors associated with HIV/HCV co-infection highlighted that drug injection practices were the main transmission mechanism,12,14,15,18,22,23,25,34,46,57 followed by blood transfusion.9,17,23,25 Since the risk factors for HIV and HCV have close connection, these can be characterized as behavioral and biological factors.58
The limitations of this review include missing information in some articles that could allow a more detailed analysis of the characteristics of the study populations and the risk factors for co-infection.
ConclusionThe data show that the prevalence of HIV/HCV co-infection is highly variable, depending on the prevalence of HIV and HCV infection, and the exposure to various risk factors in the study populations. The prevalence of HIV/HCV co-infection among people living with HIV was 20.3%. Risk factors associated with HIV/HCV co-infection were injection drug use and blood transfusion.
Conflict of interestAll authors declare to have no conflict of interest.