The number of people living with HIV / AIDS in the world has increased and, in Salvador, Brazil, the mortality rate is above the state and national rates. This study sought to describe the characteristics of HIV patients who died in a referral hospital. This is a retrospective cohort study between 2012 and 2017 conducted at the, Federal University of Bahia´s Hospital, involving patients who died during hospitalization. There were 62 deaths among the 461 hospitalized patients with a predominance of males, blacks, and residents of Salvador. Mean age was 41.4 years. Most patients had at least one associated infection and 13% had a malignant neoplasm. The main reported cause of death was septic shock / HIV-associated infections. About 6.4% had an undetectable viral load and in-hospital survival was longer in this group. The lowest in-hospital survival was seen in patients presenting with pneumonia. Although the HIV / AIDS mortality rate at this center reflects the complexity of the country's epidemiological scenario poor adherence and therapeutic failure play a key role in the risk of death.
The Acquired Immunodeficiency Syndrome (AIDS) was identified in the 1980s in the USA. Since then, approximately 79.3 million people have been infected with HIV, of whom 36.3 million died of causes directly associated with the infection. In 2020, 37.7 million people were living with HIV/AIDS and 28.2 million were on antiretroviral therapy. Despite the observed decrease in HIV incidence in last decade, the number of people living with HIV/AIDS (PLWHA) remained on the rise, as a result not only of new infections but also due to increased life expectancy for PLWHA.1
In Brazil, in 2020, the mortality rate was 4.9/100,000 inhabitants2 and in the state of Bahia, the gross mortality rate between 2010 and 2020 ranged from 3.8 to 3.9/100,000 inhabitants.2 In Salvador, capital city of Bahia, in 2020, the standardized mortality coefficient was approximately 7.8/100,000 inhabitants, ranking 5th among Brazilian capitals according to the composite index.2
Mortality due to HIV/AIDS is mostly associated with late diagnosis, poor adherence to therapy and/or absence of therapy. These factors favor the surge of opportunistic infections and neoplasms that are responsible for most deaths in untreated patients. In addition, virologic failure is associated with high mortality, underscoring the need for greater attention to this at-risk population. In untreated cases, death usually ensues two years after the onset of clinical symptoms.3,4
Mortality is a consequence of several factors related to HIV infection. In Salvador city, the mortality rate is above the state and national standards and there are scarce information on the driving factors related to this process. The objective of this study was to assess the rate and causes of mortality in HIV-infected patients admitted to a reference, university hospital in Salvador, Brazil between 2012 and 2017.
This is a retrospective cohort study involving patients who died during hospitalization at the Hospital Universitário Professor Edgard Santos (HUPES), in Salvador, between January 2012 and December 2017, and it was approved by the IRB of Maternidade Climério de Oliveira (approval number: 1.035.826).
All patients admitted to the hospital during the study period were included. Patients hospitalized due to diseases other than HIV/AIDS were included as controls.
Median survival was estimated from the date of diagnosis of HIV infection to death and from the date of admission to death (in-hospital survival). The reason for hospitalization was stratified according to the predominance of symptoms, and clustered into four groups: gastrointestinal, respiratory, neurological, and systemic symptoms (such as fever, fatigue, and weight loss). Other variables analyzed were age, sex, ethnicity, origin, and associated infections/neoplasms.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 18 (IBM Corp.). Frequencies were described for categorical variables. Means of normally distributed continuous variables (viral load, CD4+ count and comorbidities) were compared with mean in-hospital survival using Student's t test or ANOVA. Viral load and causes of death were compared using chi-squared test. Risk of death for the seropositive population was calculated using the relative risk. Results were considered statistically significant if p < 0.05.
The mean age was 41.4 ± 12.0 years, with a predominance of males (58.1%) and blacks (53.1%). The median survival from diagnosis to death was 53.0 ± 68.0 months and the median survival from hospitalization to death was 37.0 ± 33.0 days. Most (83.9%) patients lived in the city of Salvador.
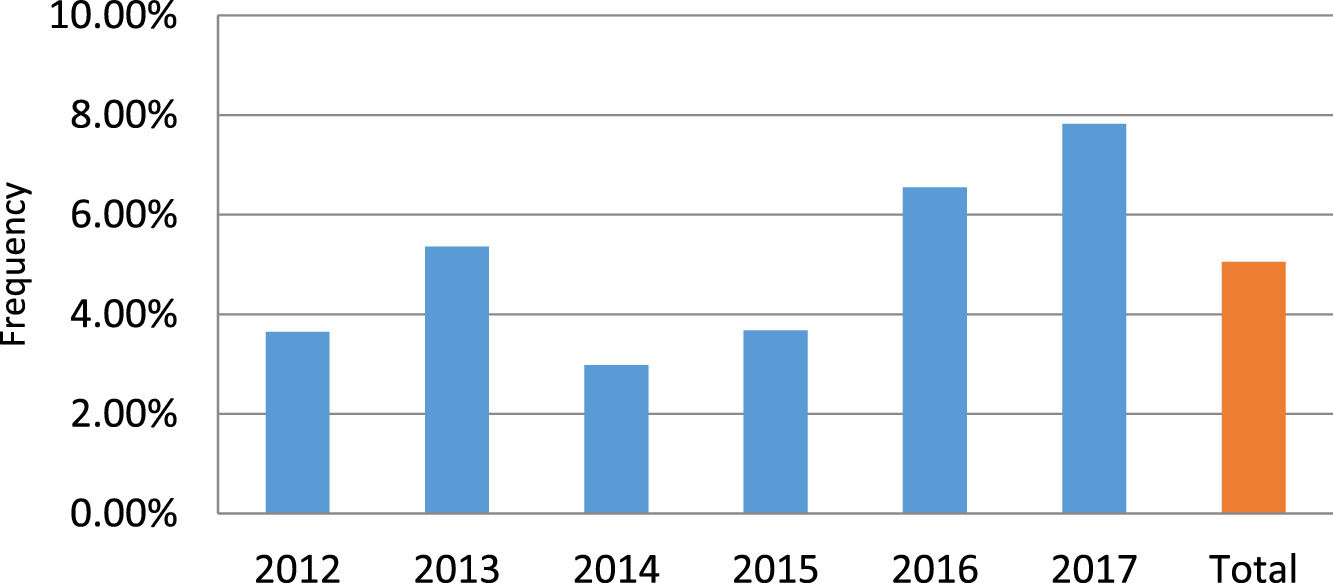
Among the 40,822 hospital admissions during the study period, 461 (1.2%) were due to HIV/AIDS. Overall, there were 1,228 deaths (3%), of which 62 were in patients with HIV/AIDS (Fig. 1). The risk of death in HIV/AIDS patients at HUPES was 4.8 times higher than in seronegative patients.
At baseline, 40.3% of patients who died had a CD4+ cell count < 50 cells/mm3, 38.7% had a viral load > 100,000 copies, and only 6.4% had undetectable viral load. Gastrointestinal symptoms were the most common cause of hospitalization (48.4%), followed by respiratory (29.0%), and neurological symptoms (14.5%). Most patients had multiple symptoms.
Most patients (67.7%) had septic shock/HIV-associated infections as the cause of death. Other causes were respiratory failure (14.5%), HIV-associated cancer (9.7%), cardiogenic shock (3.2%), and undetermined cause (3.2%). Table 1 shows these causes of death among patients with detectable or undetectable viral load. The most prevalent associated infection was oral/esophageal candidiasis (21%), followed by pneumocystosis (17.7%), tuberculosis (16.1%) and neurotoxoplasmosis (11.3%). Only eight patients (12.9%) had no associated infections. In addition, eight patients (12.9%) had some cancer associated with HIV.
Table 2 shows the survival time of patients according to prognostic markers levels.
Mean survival time, baseline and current CD4+ count, HIV plasma viral load, and use of ART in HIV patients who died during hospitalization.
In-hospital survival time was similar between men and women (p = 0.80), between age groups (p = 0.53) after adjustment, and CD4+ levels (p = 0.86). Patients with associated neoplasms had a lower survival time compared to those without (18.4 days; p = 0.04). Patients co-infected with pneumonia had an shorter survival (14.2 days; p = 0.03) and those co-infected with neurotoxoplasmosis had a longer survival (64.1 days; p = 0.47).
The HIV/AIDS mortality rates in Brazilian states are heterogeneous and have shown a significant increase in recent years despite differences in magnitude and trends.5 The overall in-hospital mortality rate in PLWHA in a referral hospital in Salvador, Brazil, was 13.44%, similar to other studies.6,7 However, it was higher when compared with rates of 11.6% in a cohort study in Rio de Janeiro,8 and in other centers located in richer countries,9,10 but lower than the rate of 33.5 % in another referral hospital in Salvador.11 The rates of other international studies in poorer countries were higher than the rates in our study,12,13 which reflects a variation between the samples and the regions studied.14
The population of the present study had a predominance of males, blacks and middle-aged adults, coming from urban areas. Variables such as sex, mean age and origin were similar to the sociodemographic profiles found in other national studies and in other countries, including developed countries.8,9,11,15,16 Regarding race, there was a variation in different regions.8,11
Most of this study sample showed a pattern in the most recent CD4+ count ≤ 250 cells/mm3, as in other studies.4,9,10,11 A viral load > 100,000 copies/mL, for most patients, is related to early death and suggests absence of therapy, poor adherence, or therapeutic failure.17
The literature shows that a viral load > 1,000 is already associated with higher mortality and virological failure and a detectable viral load, in the vast majority of patients, was associated with a lower survival, as it has been shown in other centers.4,8,9 Gastrointestinal symptoms were the most common cause of hospitalization, different from the findings of another study in which gastrointestinal symptoms were the third most common cause.7
In our study, tuberculosis was the third most prevalent associated infection, whereas most studies have shown that tuberculosis was the main associated infection and was the main cause of early death.12,15,18 In another study, the main associated infection was also candidiasis, but lower survival time was related to non-bacterial pneumonia, and septicemia was the main final cause of death, similarly to studies carried out in New York and Shanghai.9,10 The in-hospital survival time of 35 days was longer compared to other studies.8,11,13,15 A significantly lower survival time was observed in patients with associated neoplasms and the most prevalent type was non-Hodgkin's lymphoma, as shown in other centers.19,20
The main limitation of our study was the use of a single center, which limits the generalization of results to the city, state and country population. However, the study center is the second largest reference center for AIDS treatment in the state of Bahia, which minimizes selection bias. The low number of deaths in the studied period compromises the statistical analysis of the study sample. In addition, there was a lack of data related to therapeutic adherence, diagnostic confirmation of associated infections, in addition to imprecision of the cause of death in the medical records. There was a clear association between interruption of therapy and death, as highlighted by the comparison of the initial CD4+ count with that recorded at hospital admission (Table 2). On the other hand, the proportion of patients dying due to aids-related illnesses despite adequate virological suppression indicates that infectious and non-infectious problems are still a problem in this population, as a late consequence of HIV infection, even with proper treatment. Other hard to manage problem is retention in care as recognized by the Brazilian Ministry of Health. It can lead to treatment interruption and disease progression, which ultimately results in death.
The HIV/AIDS mortality rate in a referral hospital in Salvador has varied over the years and is low when compared to other centers that serve similar populations and reflects the complexity of the country's epidemiological scenario. Thus, our findings suggest that, even in the current era, further, larger prospective studies are needed to define the magnitude of mortality among hospitalized patients with HIV/AIDS and which tools are needed for greater adherence to therapy and monitoring of prognostic markers so that therapeutic failures are evidenced.