Technologies applied to mobile devices can be an important strategy in antibiotic stewardship programs.
ObjectiveThe aim of this study was to determine the impact of a decision-making application on antibiotic prescription.
MethodsThis was an observational, analytical and longitudinal study on the implementation of an antimicrobial guide for mobile application. This study analyzed the period of 12 months before and 12 months after the app implementation at a university hospital based on local epidemiology, avoiding high cost drugs and reducing the potential for drug resistance including carbapenem. Antimicrobials consumption was evaluated in Daily Defined Dose/1000 patients-day and direct expenses converted into USD.
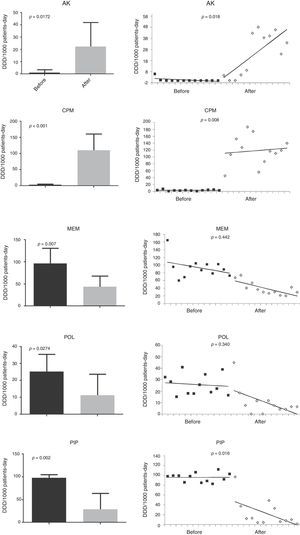
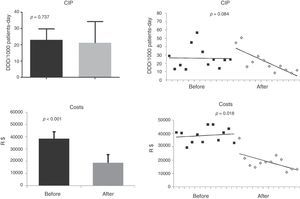
ResultsThe monthly average consumption of aminoglycosides and cefepime had a statistically significant increase (p<0.05), while the consumption of piperacillin/tazobactam and meropenem was significantly decreased (p<0.05). The sensitivity to meropenem as well as to polymyxin increased after the app implementation. A decrease in sensitivity to cefepime was observed after introduction of this antibiotic as a substitute of piperacillin/tazobactam for treating intra-hospital infections.
There was a net saving of USD 296,485.90 (p<0.05).
ConclusionAn antibiotic protocol in the app can help antibiotic stewardship reducing cost, changing the microbiological profile and antimicrobial consumption.
Proper antibiotic use is a major challenge. In addition to patient safety-related aspects (dosage and duration), the adequacy of antibiotics may reduce bacterial resistance. A major concern has been related to costs, especially in developing countries.1,2 In order to stimulate the interaction between the clinical staff and the specialized team, and as up to 84.5% of healthcare professionals use their smartphones in the work environment,3 applications for antibiotic management may be an attractive tool to bridge this gap.
Despite the existence of several manuals for the use of antimicrobials, the challenge is to choose a drug based on local epidemiology, especially when it comes to hospital infection. For this reason, many of the available applications are not useful for antimicrobial control. The application should be adequate to the local reality, considering the institution's objectives, regarding cost issues, induction of resistance, posology convenience, possibility of oral switch, among others. In the medical literature there is no description of the impact such an application has in helping in the activities of antibiotic stewardship.
The aim of this study was to determine the impact of a decision-making application on antibiotic prescription. The secondary objectives were to assess the impact on the resistance profile.
MethodsThis was an observational, analytical and longitudinal study on the implementation of an antimicrobial use guidance application. This study analyzed the period of 12 months before and 12 months after the application implementation (January 2014 through December 2014 and December 2014 through December 2015). The study was carried out at a university hospital with 186 beds, 37 in ICU, and reference in renal and cardiac transplantation.
The application consisted of a guidance manual for the choice of antimicrobials according to the site of infection. Therapeutic regimens were chosen based on local epidemiology, with suggestions avoiding the use of linezolid, daptomycin, tigecycline, and carbapenems, due to the high cost. Restriction of carbapenems was also due to the high potential of resistance induction through the production of carbapenemases. The application was linked with laboratory cultures results and susceptibility profile, allowing a real time update.
Antibiotics such as aminoglycosides and vancomycin were favored because of the low cost and low resistance among microorganisms. The use of vancomycin and aminoglycosides was based on the serum level to increase safety and acceptance by the clinical staff, and their doses were proposed and adjusted in accordance with the clinical pharmacist.
For the application implementation, all physicians of the hospital clinical staff were previously informed by e-mail and through meetings with the major groups of prescribing physicians about the application (medical clinic, intensive care units, nephrology, orthopedics, urology, cardiac surgery). The application was made available free-of-charge on the iOS and Android platforms in their respective download services, App store and Google play, respectively.
To evaluate the application use, antimicrobials consumption was evaluated, which were calculated in DDD/1000 patients-day and direct expenses converted into USD (United States dollar). The susceptibility profile of the main antimicrobials against bacteria obtained from clinical samples in the same period were considered, excluding surveillance samples.
Other information such as number of downloads, informing their respective geographical location, most accessed page and usage time per user were also evaluated.
For the quantitative analysis, univariate analyses were performed according to the type of variable and its distribution, such as Student's t test, Mann–Whitney, chi-square or Fisher exact test. Segmented regression analysis was used to statistically evaluate the effect of the decision-making application (app) on antibiotic prescription.4 The adjusted model was: Yt=β0+β1T+β2Xt+β3TXt, where T is time of observations (month), Yt is the patients-day on time T (outcome), Xt is a dummy variable representing period (0 and 1 for before and after use of the app, respectively), β0 represents the baseline level (first month), β1 indicates the change in patients-day for each month, β2 is the level change, and β3 is the slope change following the use of the app. Significance of level and slope changes was evaluated using deviance function. p<0.05 was considered statistically significant. All analyses were performed using Stata/SE 14.1 (StataCorp LP, USA).
ResultsThe application was implemented in December 2014. After implementation, 1-year data using the device was evaluated. Among users, 62% used the iOS system while 38% used the Android system. Although the application was for use in this hospital, it was available in stores of each system, allowing people elsewhere to use it as well. Only in the city of Curitiba, where the study hospital is located, there were 1741 downloads. The application usage time is short, because as it is used for consultation, 50% of accesses took less than 1min.
The monthly average consumption of aminoglycosides and cefepime had a statistically significant increase (p<0.05), while the consumption of piperacillin/tazobactam and meropenem decreased significantly (p<0.05) (Fig. 1). Consumption of quinolones (ciprofloxacin) did not change and a reduction in the use of polymyxin was observed.
To assess the susceptibility profile, 922 cultures of Gram-negative bacilli were analyzed in 2014, out of a total of 1214 cultures. There was increased susceptibility to meropenem (73%–83%, p<0.05) as well as to polymyxin (69%–83%, p<0.05) in the year of 2015 (622 clinical samples out of a total of 878 cultures). Decrease susceptibility to cefepime (62%–57%, p<0.05) was noted after introduction of this antibiotic as a substitute of piperacillin/tazobactam for treating intra-hospital infections. Susceptibility to amikacin (79%–83%), ciprofloxacin (52%–49%) and gentamycin (68%–69%) have not changed significantly in the two periods.
In relation to antibiotics cost, there was a progressive and significant reduction of expenditures. Comparing the cost in 2014 with that of 2015 there was a saving of US$ 296,485.90 (p<0.05), an average of US$ 24,707.00 per month.
DiscussionThe increase in use of mobile phones in the last decade is evident, from 450 million in 2000 to five billion ten years later,5 reaching 98% of healthcare professionals, of whom 84.5% bring their cell phones to the hospital every day.
Taking advantage of this, more and more applications are being developed to aid in diagnosis and treatment.6 Therefore, following this new trend, the application also has its space within the hospital environment. The application tested in this study showed to be efficient, since it was able to significantly reduce costs, when comparing the year following implementation of the application in the hospital with the year that preceded its implementation. It generated an economy of almost USD 300,000 in one year.
In Brazil, drug costs account for a large share of the hospital bill, which is not the case in developed countries. For this reason, the decrease in consumption of high-cost antimicrobials such as polymyxin, tigecycline, linezolid, meropenem is fundamental for resources saving. The pattern of antimicrobials consumption within the hospital was influenced by the application protocol. The mean monthly consumption of aminoglycosides and cefepime had a significant increase, while consumption piperacillin/tazobactam and meropenem was reduced. It can be inferred, therefore, that the clinical staff followed the application's protocol.
In the analysis of microbial susceptibility, there was a direct relationship between consumption and resistance to cefepime, while the reduction in meropenem consumption was translated in increased susceptibility. The same was evident for polymyxin. This fact is extremely relevant in the current context of carbapenem-resistant Enterobacteriaceae, since therapeutic options are limited.
The limitations of this study include the impossibility to monitor how many professionals have accessed the application, the current impossibility of external validation once the application was not the sole orientation in the stewardship.
In summary, the use of an application protocol can significantly interfere with the institution's reality, reducing cost, changing the microbiological profile and antimicrobial consumption pattern according to guidelines of an appropriate stewardship. The use of the application at no time replaces the multidisciplinary group functions of rational use of antimicrobials, but it is an ally in the difficult task of guiding physicians.
Conflicts of interestThe authors declare no conflicts of interest.
We thank the collaboration of Paulo De Tarso Barros Dos Santos Filho, Matheus Wuerzius Chillemi, Luiz Eduardo Andraus Marcondes Do Nascimento and Fabio Aurelio Franco MD in this study.