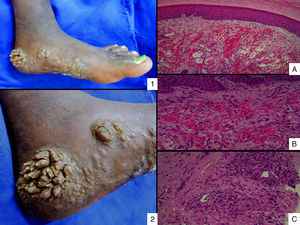
Kaposi's sarcoma (KS) is a vascular lesion of low-grade malignant potential and is the most frequent neoplasm in acquired immunodeficiency syndrome (AIDS).1 Typical cases can present with erythematous or violaceous lesions, plaques or nodules, but the hyperkeratotic variants are rare.1 A 31-year-old woman presented with a 6-year history of intractable injury in the left foot with worsening in pain and difficulty walking. The patient had a positive serology for HIV and reported intermittent and irregular use of antiretroviral therapy. On examination, a vegetative lesion with 20cm in its largest diameter located on the medial side and plantar region of the left foot (Fig. 1(1, 2)) was noted. Fungal, bacteria/mycobacteria cultures were negative. Skin biopsy revealed hyperkeratosis and dermis with proliferation of mesenchymal lineage cells with formation of malformed vessels with the presence of red blood cells out of the light thereof (Fig. 1A–C). KS is a vascular neoplasm from vascular and lymphatic endothelium caused by human herpesvirus 8.1 Four different types of KS are distinguished: classic (Mediterranean), endemic (African), iatrogenic (transplant-related), and epidemic (AIDS-related).1 Hyperkeratotic KS is a rarely described clinicopathalogic variant of KS.2 There is verrucous epidermal acanthosis and hyperkeratosis overlying an often fibrotic epidermis.2 The explanation for the hyperkeratotic variant of KS may be the high interstitial protein concentration that retains fluid in the connective tissue, in turn leading to chronic inflammation causing fibrosis and hyperkeratosis.3 Highly active antiretroviral therapy (HAART) has greatly changed the clinical course of HIV-infected patients and several epidemiological studies indicate a decrease of several opportunistic infections and Kaposi's sarcoma.4
(1) Hyperkeratotic KS on the medial side and plantar region of the left foot. (2) Hyperkeratotic KS (in more detail). Epidermis with hyperkeratosis (A) and dermis with proliferation of mesenchymal lineage cells and malformed vessels with the presence of red blood cells out of the light thereof (B and C).
Cassio Porto Ferreira and José Augusto da Costa Nery contributed to clinical care and paper preparation. Alice Miranda contributed to laboratory diagnosis and paper preparation.
Role of funding sourceNone.
Ethics committee approvalCEP 14/2001 Instituto Oswaldo Cruz – CPqHEC/FIOCRUZ.
Conflicts of interestThe authors declare no conflicts of interest.