Influenza season is expected between October and February in the northern hemisphere, including Mexico. Previous studies suggested that transmission peak may occur earlier in Yucatan, a state in southeast Mexico.
Objectives(a) Describe the seasonality of 2018 influenza cases seen at O´Horan hospital, statewide, and nationwide; (b) analyze the characteristics, clinical manifestations and outcomes of ambulatory and hospitalized patients; (c) analyze fatal outcomes occurrence among vaccinated and unvaccinated individuals.
MethodsRetrospective analytic cohort of all confirmed influenza cases assisted at O´Horan hospital during 2018, along with a chronologic graphic description of the statewide epidemic curve from the epidemiological surveillance registries.
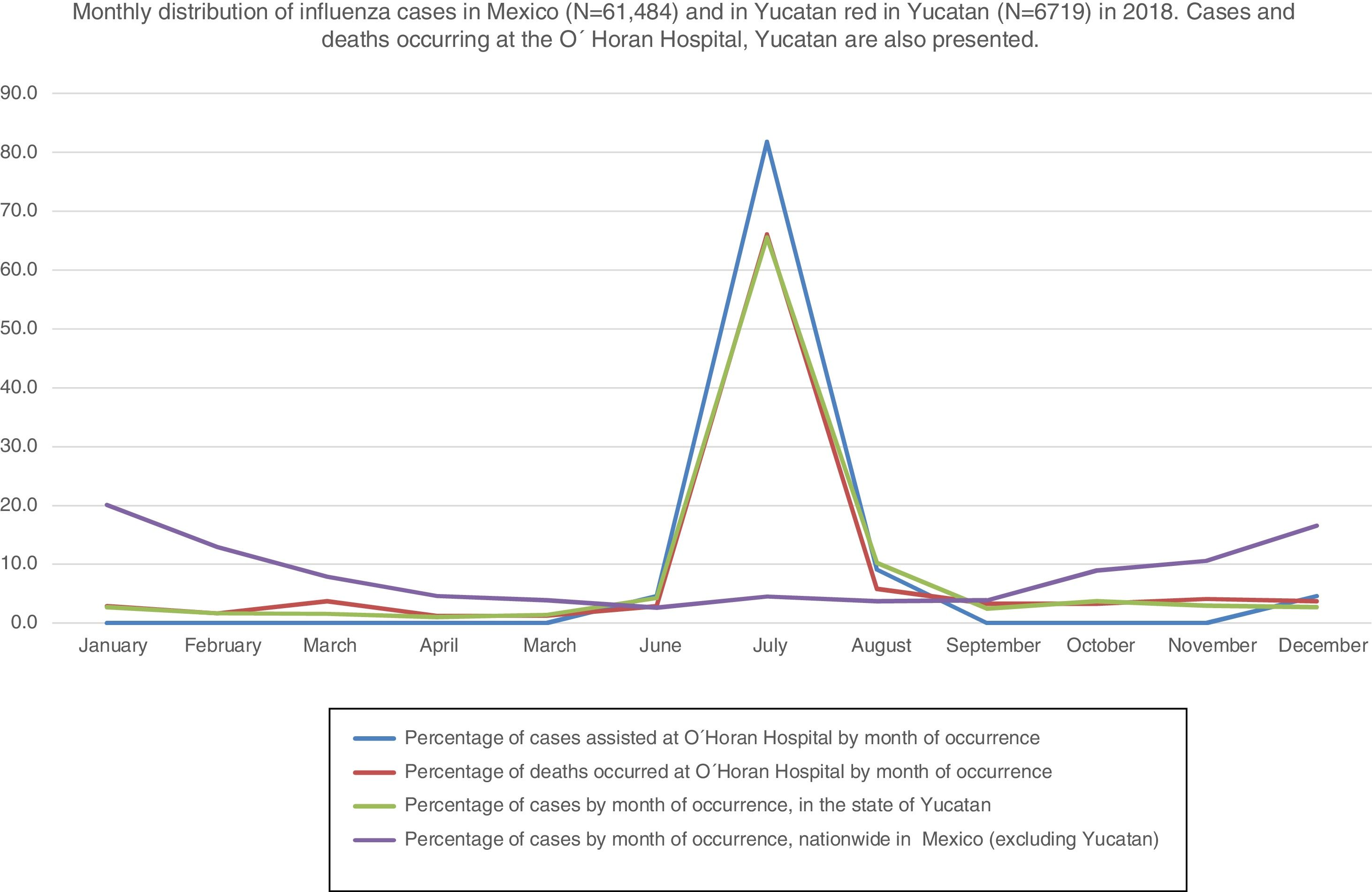
ResultsA total of 264 influenza cases were analyzed; 145 (55%) were female; 26% were vaccinated. Health workers and unvaccinated individuals were more prone to develop severe cases. Dyspnea and tachypnea were strong predictors of hospitalization; headache, myalgias, arthralgias and rhinorrhea correlated inversely. 236 (89.47%) cases occurred in July and 22 of the 23 deaths occurred before October. No fatal outcomes were observed among vaccinated individuals. Influenza AH1N1 represented 83.6% of serotyped cases.
DiscussionOnset of influenza season in Yucatan may reflect a need for rethinking timing of vaccination and of preventive campaigns, as most cases occurred before vaccination period.
Every year, almost 15% of the world population becomes infected with influenza, resulting in deaths worldwide. Influenza surveillance is sentinel-type in Mexico, meaning that it is aimed to detect the occurrence and onset of cases, along with identifying any new circulating viral strains. In general, clinical specimens of hospitalized patients are laboratory-confirmed and randomly serotyped. For ambulatory cases, samples are analyzed depending on the available resources. Samples are processed at State Public Health Laboratories with standardized techniques and quality control. When an epidemic is declared, all health units are urged to report cases (even if unsampled) and to emphasize in identifying severe cases to be hospitalized. 2018 was declared as an epidemic year. Even when the influenza season is expected to happen between October and February in the northern hemisphere, including Mexico, where vaccination period starts in October. Previous studies suggested that transmission peak may occur earlier in Yucatan.1–4
Chronology of non-severe, hospitalized and fatal cases has not yet been reported for the region, nor are the signs and symptoms presented in-patients or out-patients. Updating the chronological presentation, sociodemographic characteristics, clinical manifestations, antecedents of vaccination, and main outcomes among hospitalized and ambulatory patients could provide relevant information for preventive purposes.
The aims of the present communication was to (a) Describe the chronology of 2018 influenza cases from O´ Horan General Hospital, statewide, and nationwide; (b) analyze the characteristics, clinical manifestations and outcomes of ambulatory and hospitalized patients; and (c) analyze fatal outcomes among vaccinated and unvaccinated individuals.
MethodsThis retrospective-cohort study is based on the epidemiologic case reports of all patients who were clinically diagnosed with influenza at O´ Horan General Hospital in 2018. For each patient, the standardized, unified, epidemiological case report form including clinical manifestations was reviewed. Case report forms, laboratory results and clinical outcomes at discharge of all hospitalized patients were identified with the international classification of diseases under code J10. Ambulatory cases were monitored and recorded. All cases were anonymized, coded in a spreadsheet then transformed into variables using Stata14 software for descriptive statistics and association measures (Odds Ratio); results were considered statistically significant when p-value <0.05; post hoc goodness of fit Hosmer-Lemeshow was performed.
The annual influenza cases distribution for the studied hospital, the state, and nationwide were grouped by month of onset of symptoms. Timing of onset of O’ Horan General Hospital cases was derived from case report forms, while statewide and nationwide cases were retrieved from an open-access platform of the Board of Health Department for Access to Health Information and the department of Epidemiological Surveillance.
ResultsFor 2018, in the state of Yucatan, 6719 ambulatory cases and 480 severe cases were reported. Of those, 264 were assisted at O´Horan General Hospital, where ambulatory patients represented 61.7% (n=164), 145 (55%) women, 11 (7%) pregnant, mean age 27.1 years, 46 (27.42) health workers. A total of 40 (26.85%) ambulatory and 9 (6.21%) hospitalized patients were vaccinated between October 2017 and January 2018.
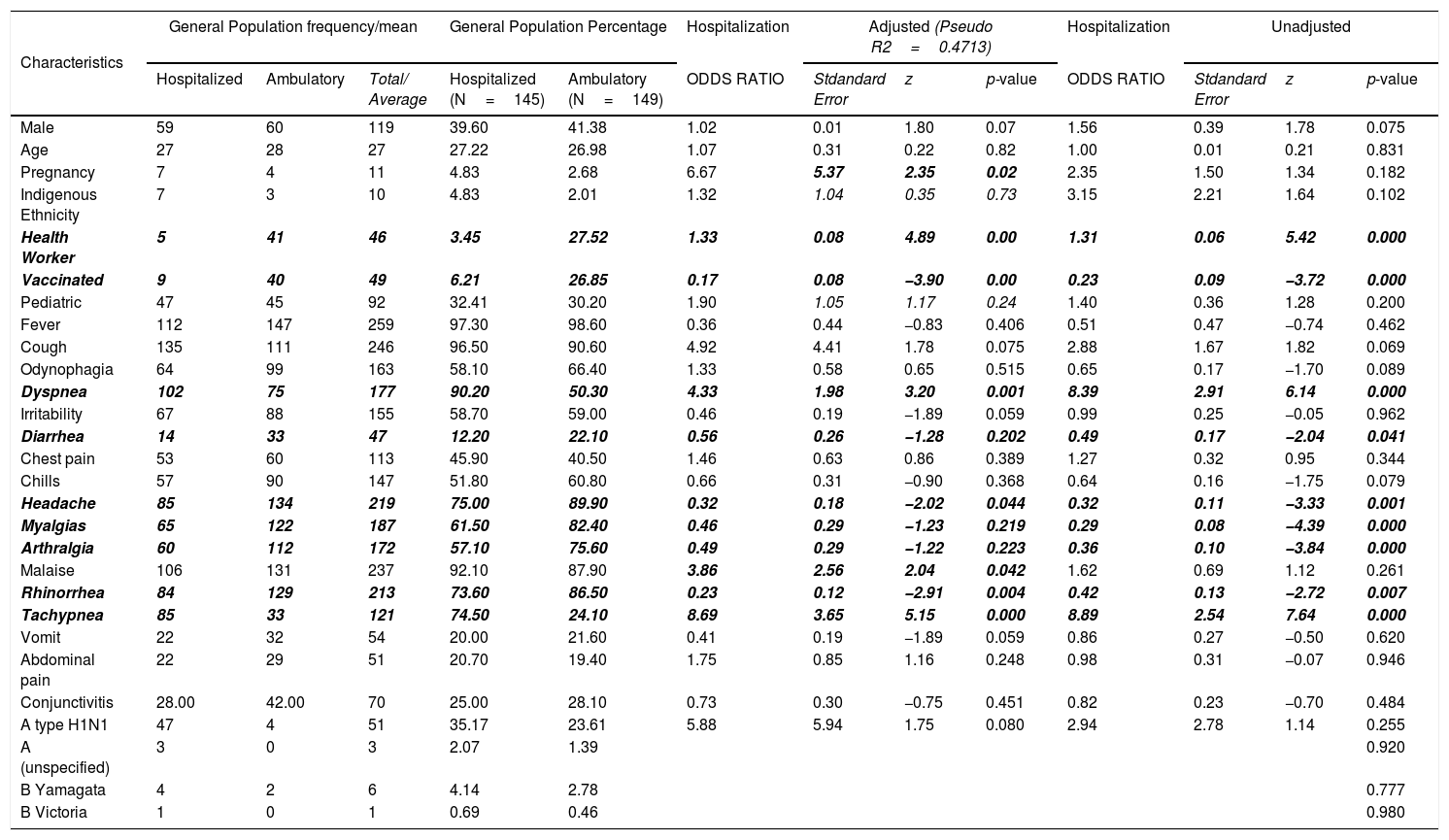
Health workers and unvaccinated individuals were more prone to have a severe course of the infection. Clinical manifestations among ambulatory and hospitalized patients varied; while dyspnea and tachypnea (Table 1) were strong predictors of hospitalization, headache, myalgias, arthralgias and rhinorrhea correlated inversely.
Signs and symptoms among hospitalized and ambulatory patients diagnosed with influenza in 2018 at O´Horan Hospital in Yucatan, Mexico (N=264).
| Characteristics | General Population frequency/mean | General Population Percentage | Hospitalization | Adjusted (Pseudo R2=0.4713) | Hospitalization | Unadjusted | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospitalized | Ambulatory | Total/ Average | Hospitalized (N=145) | Ambulatory (N=149) | ODDS RATIO | Stdandard Error | z | p-value | ODDS RATIO | Stdandard Error | z | p-value | |
| Male | 59 | 60 | 119 | 39.60 | 41.38 | 1.02 | 0.01 | 1.80 | 0.07 | 1.56 | 0.39 | 1.78 | 0.075 |
| Age | 27 | 28 | 27 | 27.22 | 26.98 | 1.07 | 0.31 | 0.22 | 0.82 | 1.00 | 0.01 | 0.21 | 0.831 |
| Pregnancy | 7 | 4 | 11 | 4.83 | 2.68 | 6.67 | 5.37 | 2.35 | 0.02 | 2.35 | 1.50 | 1.34 | 0.182 |
| Indigenous Ethnicity | 7 | 3 | 10 | 4.83 | 2.01 | 1.32 | 1.04 | 0.35 | 0.73 | 3.15 | 2.21 | 1.64 | 0.102 |
| Health Worker | 5 | 41 | 46 | 3.45 | 27.52 | 1.33 | 0.08 | 4.89 | 0.00 | 1.31 | 0.06 | 5.42 | 0.000 |
| Vaccinated | 9 | 40 | 49 | 6.21 | 26.85 | 0.17 | 0.08 | −3.90 | 0.00 | 0.23 | 0.09 | −3.72 | 0.000 |
| Pediatric | 47 | 45 | 92 | 32.41 | 30.20 | 1.90 | 1.05 | 1.17 | 0.24 | 1.40 | 0.36 | 1.28 | 0.200 |
| Fever | 112 | 147 | 259 | 97.30 | 98.60 | 0.36 | 0.44 | −0.83 | 0.406 | 0.51 | 0.47 | −0.74 | 0.462 |
| Cough | 135 | 111 | 246 | 96.50 | 90.60 | 4.92 | 4.41 | 1.78 | 0.075 | 2.88 | 1.67 | 1.82 | 0.069 |
| Odynophagia | 64 | 99 | 163 | 58.10 | 66.40 | 1.33 | 0.58 | 0.65 | 0.515 | 0.65 | 0.17 | −1.70 | 0.089 |
| Dyspnea | 102 | 75 | 177 | 90.20 | 50.30 | 4.33 | 1.98 | 3.20 | 0.001 | 8.39 | 2.91 | 6.14 | 0.000 |
| Irritability | 67 | 88 | 155 | 58.70 | 59.00 | 0.46 | 0.19 | −1.89 | 0.059 | 0.99 | 0.25 | −0.05 | 0.962 |
| Diarrhea | 14 | 33 | 47 | 12.20 | 22.10 | 0.56 | 0.26 | −1.28 | 0.202 | 0.49 | 0.17 | −2.04 | 0.041 |
| Chest pain | 53 | 60 | 113 | 45.90 | 40.50 | 1.46 | 0.63 | 0.86 | 0.389 | 1.27 | 0.32 | 0.95 | 0.344 |
| Chills | 57 | 90 | 147 | 51.80 | 60.80 | 0.66 | 0.31 | −0.90 | 0.368 | 0.64 | 0.16 | −1.75 | 0.079 |
| Headache | 85 | 134 | 219 | 75.00 | 89.90 | 0.32 | 0.18 | −2.02 | 0.044 | 0.32 | 0.11 | −3.33 | 0.001 |
| Myalgias | 65 | 122 | 187 | 61.50 | 82.40 | 0.46 | 0.29 | −1.23 | 0.219 | 0.29 | 0.08 | −4.39 | 0.000 |
| Arthralgia | 60 | 112 | 172 | 57.10 | 75.60 | 0.49 | 0.29 | −1.22 | 0.223 | 0.36 | 0.10 | −3.84 | 0.000 |
| Malaise | 106 | 131 | 237 | 92.10 | 87.90 | 3.86 | 2.56 | 2.04 | 0.042 | 1.62 | 0.69 | 1.12 | 0.261 |
| Rhinorrhea | 84 | 129 | 213 | 73.60 | 86.50 | 0.23 | 0.12 | −2.91 | 0.004 | 0.42 | 0.13 | −2.72 | 0.007 |
| Tachypnea | 85 | 33 | 121 | 74.50 | 24.10 | 8.69 | 3.65 | 5.15 | 0.000 | 8.89 | 2.54 | 7.64 | 0.000 |
| Vomit | 22 | 32 | 54 | 20.00 | 21.60 | 0.41 | 0.19 | −1.89 | 0.059 | 0.86 | 0.27 | −0.50 | 0.620 |
| Abdominal pain | 22 | 29 | 51 | 20.70 | 19.40 | 1.75 | 0.85 | 1.16 | 0.248 | 0.98 | 0.31 | −0.07 | 0.946 |
| Conjunctivitis | 28.00 | 42.00 | 70 | 25.00 | 28.10 | 0.73 | 0.30 | −0.75 | 0.451 | 0.82 | 0.23 | −0.70 | 0.484 |
| A type H1N1 | 47 | 4 | 51 | 35.17 | 23.61 | 5.88 | 5.94 | 1.75 | 0.080 | 2.94 | 2.78 | 1.14 | 0.255 |
| A (unspecified) | 3 | 0 | 3 | 2.07 | 1.39 | 0.920 | |||||||
| B Yamagata | 4 | 2 | 6 | 4.14 | 2.78 | 0.777 | |||||||
| B Victoria | 1 | 0 | 1 | 0.69 | 0.46 | 0.980 | |||||||
| Deaths reported among influenza patients according to vaccination status | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deaths | General population frequency | General Population Percentage | Adjusted | Unadjusted | |||||||||
| Hospitalized | Ambulatory | Total | Hospitalized | Ambulatory | Death Odds Ratio | Stdandard Error | z | p-value | Death Odds Ratio | Stdandard Error | z | p-value | |
| Unvaccinated | 21 | 1 | 22 | 95.45 | 1.05 | 12.84 | 15.18 | 2.16 | 0.031 | 31.16 | 32.19 | 3.33 | 0.001 |
| Vaccinated | 0 | 0 | 0 | No observations | |||||||||
| Post hoc Hosmer Lewenshow p=0.930 | |||||||||||||
Of 62 serotyped samples, one was hemolyzed; 51 (83.6%) were type AH1N1, 7 (11.47%) were influenza B (one Victoria, six Yamagata) and 3 (4.9%) were unspecified Influenza A. In addition, 19 (82.6%) deaths were associated with AH1N1.
At O'Horan General Hospital, during 2018, 236 (89.47%) cases occurred before October. Due to influenza, 23 (8.27%) patients died, of whom 22 died before October (Fig. 1). All fatal cases occurred in unvaccinated individuals.
Monthly distribution of influenza cases in Mexico (N=61,484) and in Yucatan red in Yucatan (N=6719) in 2018. Cases and deaths occurring at the O´Horan Hospital, Yucatan are also presented.
Chronology of cases occurrence at the hospital coincided with the state transmission for 2018 (Fig. 1) but different from the national trend. An additional figure provides a 10-year chronological distribution of cases.
DiscussionInfluenza infection became the first pandemic in the 21st century, to show seasonal patterns.1–3 The observed pattern at O´Horan General Hospital in 2018 is congruent with the earlier yearly seasonality in Yucatan.4 In addition, the present study adds that almost 90% of the ambulatory influenza cases and hospitalizations occurred even before the seasonal vaccination started and that 22 out of the 23 fatalities occurred before the expected season onset. Previous studies from Yucatan had emphasized that vaccination should start earlier.4 Grohskopf et al. recommended early vaccination for regions with earlier timing of influenza season, always considering that waning would also decrease earlier,5 but as Yucatan historical data show that incidence is unlikely to increase in January-February,6 implementing an earlier vaccination in Yucatan seems to be a reasonable preventive strategy. Previous season vaccination may have been protective in severe hospitalized cases, as none of them died.
Influenza AH1N1 was the most common type associated with mortality, which is consistent with previous findings,7 but contrary to a recent study from Tekin et al., in which AH3N2 was related with more fatal cases.8 We observed that the presence of influenza signs and symptoms varied, although headache did not correlate with hospitalization.9 The association between dyspnea and tachypnea with hospitalization has been previously reported in other series.9,10 In conclusion, yearly season of influenza cases in Yucatan may reflect a need for implementing specific preventive strategies and even though no vaccinated individual with a severe case died in the present series, fatal cases occurred even before the time when the season (and vaccination) was expected to start.
Conflict of interestThe authors declare that there is no conflict of interest.