Infection by hepatitis B virus (HBV) is a worldwide public health problem. Chronic HBV infection with high viral replication may lead to cirrhosis and/or hepatocellular carcinoma. Mutant HBV strains, such as the HBV A1762T/G1764A double mutant, have been associated with poor prognosis and higher risk of the patient for developing cirrhosis and/or hepatocellular carcinoma. This study analyzed the presence of the HBV A1762T/G1764A double mutant in patients with chronic HBV and its association with clinical parameters such as viral load, aminotransferases, and HBV antigens. A total of 49 patients with chronic hepatitis B were included in the study, and the HBV A1762T/G1764A double mutant strain was detected in four samples (8.16%) by polymerase chain reaction followed by restriction fragment length analysis (PCR-RFLP). The viral load was not significantly different between patients with or without the double mutant strain (p=0.43). On the other hand, carriers of the HBV A1762T/G1764A double mutant had higher levels of ALT (p=0.0028), while AST levels did not differ between groups (p=0.051). In this study, 75% of the samples with the HBV A1762T/G1764A double mutation were HBeAg negative and anti-HBe positive, reflecting seroconversion even though they still displayed high viral loads. Our study has shown that the HBV A1762T/G1764A double mutant strain circulates in Brazilian patients, and is associated with elevated levels of ALT and HBeAg seroconversion.
Infection by hepatitis B virus (HBV) is a public health problem. Despite being a disease for which there is vaccine available, it is estimated that two billion people are infected worldwide, out of which about 350 million have serological markers of active infection.1 Carriers of HBV may develop cirrhosis and/or hepatocellular carcinoma (HCC), which may be related to mutations in specific regions of the HBV genome and is responsible for over one million deaths annually.2
The areas with high prevalence of HBV (>8%) are concentrated in Southeast Asia, China, the Philippines, Africa, the Amazon Basin, and the Middle East; areas with intermediate prevalence (2–7%) are regions of Eastern Europe, Central Asia, Japan, Israel, and Russia; and areas with low prevalence (<2%) are Western Europe, Australia, New Zealand, North America, and South America.3,4 In Brazil, the distribution of HBV is quite heterogeneous; it is more prevalent in the northern region of the country, covering the states of Acre, Amazonas, Rondônia, and Roraima, and less prevalent in the South. From 1999 to 2011, of the 120,343 confirmed cases of hepatitis B that were reported in Brazil, 31.6% (38,007 cases) were in the Southern region, with a total of 1,693 cases reported in the city of Porto Alegre, Rio Grande do Sul.5,6
HBV presents eight genotypes (A, B, C, D, E, F, G, and H), which differ in their nucleotide sequences.7–11 In Brazil, A, B, D, and F genotypes are found,12,13 the most prevalent being genotype A, accounting for 48.5% of all cases, followed by genotype D in 38.5%.5,12–14 HBV genotype D is the most prevalent genotype in the state of Rio Grande do Sul, Brazil, being found in approximately 63% of the cases, followed by genotype A (32%); genotype F represents only 5% of all cases.7,12
HBV is an enveloped virus of the family Hepadnaviridae; its partially double-stranded circular DNA genome contains approximately 3200 nucleotides (3.2kb), arranged in overlapping genes. Gene S has three regions, Pre-S1, Pre-S2 and S, each coding for one of the surface glycoprotein – S (small), L (large), and M (middle), respectively, and also for the HBV s antigen (HBsAg); gene C, with regions pre-core and core, codes for antigens c and e (HBcAg and HBeAg, respectively); gene P codes the DNA polymerase; and gene X code for the x antigen (HBxAg).2,5,15–18
Mutations in certain regions of the HBV genome, such as in the pre-core and in the basal core promoter (BCP), may disrupt the expression of viral proteins. The BCP region is located in the X gene, which in addition to coding for HBxAg, it also regulates the expression of HBeAg; patients carrying HBV strains with mutations in this region often appear as HBeAg-negative. Notably, even though they appear to have seroconverted, these patients might have an unfavorable prognosis.19–21
Among the mutations described in the BCP region, the HBV A1762T/G1764A double mutation is worth of note for its significant clinical importance: patients with this mutant strain showed an increased level of viral replication, and decrease or absence of HBeAg. Despite being HBeAg-negative, these patients may rapidly develop liver cirrhosis, which installs progressively and despite being often asymptomatic, it may progress to HCC.22–29 The HBV A1762T/G1764A double mutation is located in the BCP region and causes an amino acid substitution from lysine (K) to methionine (M) at position 1762, and from valine (V) to isoleucine (I) at position 1764.30,31
The aim of this study was to assess the circulation of HBV strains with the A1762T/G1764A double mutation in patients from Porto Alegre, Rio Grande do Sul. The presence or absence of the double mutant was correlated with viral load, aminotransferases levels, as well as with HBeAg and anti-HBe parameters.
Material and methodsHuman subjectsThis was a cross-sectional study, which followed-up HBV patients receiving care at the Infectious Diseases Adult Clinic of the Nossa Senhora da Conceição Hospital in Porto Alegre, Brazil, and from the Gastroenterology Clinic of Santa Casa de Porto Alegre Hospital Complex, Brazil, from November 2012 to December 2013. This study was approved by the Research Ethics Committee (CEP-UFCSPA), Protocol Number 575.347.
All patients included in this study were HBsAg-positive for more than six months, with viral load higher than 200copies/ml, and agreeing to participate in the study by signing the Informed Consent Form. Exclusion criteria were HBsAg-negative, alcohol consumption of more than 20g/day (for women) or 30g/day (for men), coinfection with hepatitis D virus (HDV), autoimmune hepatitis and NASH, patients on drug treatment for hepatitis, and patients who were unable to read and sign the Informed Consent Form. Each sample gained a numerical sequence and was de-identified, and a database was created including the main laboratory tests: biochemical parameters, HBV viral load, HBV antigens, anti-HBV antibodies, and aminotransferases. Such information was abstracted from physical and electronic records of each patient together with their coadministred medications.
All selected patients were submitted to blood collection, which was carried out at the hospital by using vacuum venipuncture in 4ml tubes containing EDTA. The samples were transported to the Molecular Biology Laboratory of Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), where molecular analyses were performed.
Molecular analysisAn aliquot of 500μl of blood was centrifuged for five minutes at 500×g at room temperature; plasma was separated in a 1.5ml tube. All plasma samples were numbered and were stored at −80°C until viral DNA extraction.
Viral DNA was extracted with PureLink™ viral DNA/RNA Kit (Invitrogen Life Technologies), quantified in a NanoDrop instrument (NanoDrop Technologies, Wilmington, USA) and used as template in PCR. The primers used in the PCR were the forward primer P2-1 that anneals at position 1652–1672 (5′-CACAAGAGGACTCTTGGACT-3′), and the reverse primer P2-2 that anneals at position 1940–1959 (5′-GGCAAAAAAGAGAGTAACTC-3′). PCR was performed with GoTaq® Master Mix (Promega) and 0.05μM of each primer, in a final volume of 25μl. Reaction conditions were 95°C for five minutes; 40 cycles of 95°C for one minute, 55°C for one minute, 72°C for one minute; final extension at 72°C for five minutes. The PCR product was analyzed by electrophoresis on 1.5% agarose gel.32,33
The PCR product presented a fragment size of 307bp, which was subjected to RFLP with Sau3AI enzyme, which cleaves the nucleotide sequence with the A1762T/G1764A (G/ATC) double mutation. Therefore, when the A1762T/G1764A double mutation is present, Sau3AI enzyme cleaves the amplicon generating two fragments of 197pb and 110pb. For the RFLP, 10μl of the PCR product was cleaved with 10 units of Sau3AI enzyme in a final volume of 50μl. The reaction was incubated at 37°C for 100min and inactivated at 65°C for 20min. The RFLP product was analyzed by electrophoresis on 2% agarose gel.
Statistical analysisQuantitative variables were described as the minimum, maximum, mean, standard deviation, and compared between groups with Student's t test. Categorical variables were analyzed by the chi-square test. The significance level was 5.0%.
ResultsA total of 49 patients were included in this study, 21 females (42.85%) and 28 males (57.14%). Age ranged from 19 through 79 years-old (average of 50.48±12.76).
Results of the biochemical analysis, HBV viral load, HBV antigen, anti-HBV antibodies, and aminotransferase tests were abstracted from the physical and electronic records of each patient. Divergence occurs in the total number of samples for some parameters, due to unavailability of some patient records.
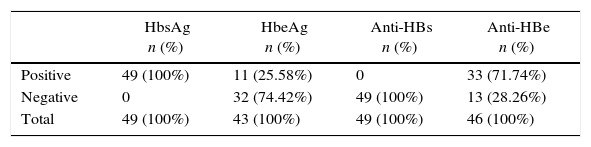
The main antigens and antibodies used for HBV evaluation were HBsAg, HBeAg, anti-HBs, and anti-HBe. Table 1 summarizes the reactivity of patients’ sera to each of these markers. All patients were positive for the HBsAg and none of them displayed antibodies against this antigen. Regarding HBeAg, which is a marker of viral replication, 25.58% of the patients were HBeAg-positive, and 71.73% of the patients had seroconverted as shown by the anti-HBe levels. Two patients were also coinfected with HIV, and four with HCV.
Main serological parameters in patients with chronic hepatitis B.
| HbsAg n (%) | HbeAg n (%) | Anti-HBs n (%) | Anti-HBe n (%) | |
|---|---|---|---|---|
| Positive | 49 (100%) | 11 (25.58%) | 0 | 33 (71.74%) |
| Negative | 0 | 32 (74.42%) | 49 (100%) | 13 (28.26%) |
| Total | 49 (100%) | 43 (100%) | 49 (100%) | 46 (100%) |
HBsAg, hepatitis B surface antigen; HBeAg, hepatitis B e antigen; anti-HBs, antibody against the surface antigen; anti-HBe, antibody against the e antigen.
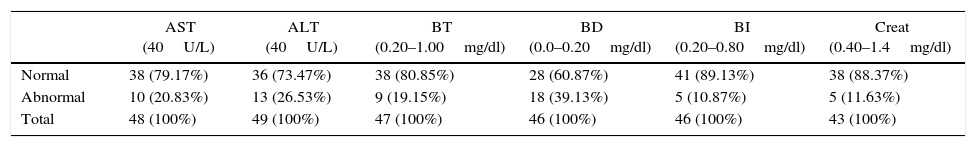
Analysis of liver biochemical parameters showed that the majority of patients had normal levels of aminotransferases, bilirubin, and creatinine, except for direct bilirubin, which was altered in 39.13% of the patients (Table 2). Also, five (11.63%) patients have increased creatinine levels, but all of them were on conservative treatment.
Main biochemical parameters in patients with chronic hepatitis B.
| AST (40U/L) | ALT (40U/L) | BT (0.20–1.00mg/dl) | BD (0.0–0.20mg/dl) | BI (0.20–0.80mg/dl) | Creat (0.40–1.4mg/dl) | |
|---|---|---|---|---|---|---|
| Normal | 38 (79.17%) | 36 (73.47%) | 38 (80.85%) | 28 (60.87%) | 41 (89.13%) | 38 (88.37%) |
| Abnormal | 10 (20.83%) | 13 (26.53%) | 9 (19.15%) | 18 (39.13%) | 5 (10.87%) | 5 (11.63%) |
| Total | 48 (100%) | 49 (100%) | 47 (100%) | 46 (100%) | 46 (100%) | 43 (100%) |
AST, aspartate aminotransferase; ALT, alanine aminotransferase; BT, total bilirubin; BD, direct bilirubin; BI, indirect bilirubin; Creat, creatinine. Normal reference values for each parameter are shown.
All samples were successfully amplified by PCR, using primers specific for the BCP region of HBV where the double mutation is located, generating fragments of 307pb. Analysis by RFLP revealed that four (8.16%) patients carried the HBV A1762T/G1764A double mutant, as shown by the presence of DNA fragments of 197pb and 110pb; the fragment of 307pb was also visible in these samples (not shown).
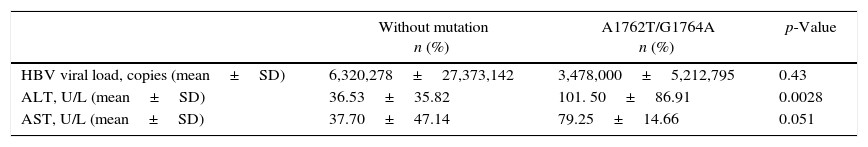
To verify a possible association between the presence of the A1762T/G1764A double mutant and the risk of developing chronic hepatitis, viral load and aminotransferases were analyzed in these patients. As shown in Table 3, there was no significant difference in the mean viral load between patients carrying the double mutant and patients without the mutant strain. Aspartate aminotransferase (AST) levels showed a larger variance in patients without the double mutant, but the mean AST levels were higher in patients with HBV A1762T/G1764A double mutant. However, such differences were not significant (p=0.051). On the other hand, alanine aminotransferase (ALT) levels were significantly higher in patients carrying the double mutant (p=0.0028).
Mean values of HBV viral load and aminotransferases in patients with chronic hepatitis B according to the presence of the double mutation A1762T/G1764A in HBV.
| Without mutation n (%) | A1762T/G1764A n (%) | p-Value | |
|---|---|---|---|
| HBV viral load, copies (mean±SD) | 6,320,278±27,373,142 | 3,478,000±5,212,795 | 0.43 |
| ALT, U/L (mean±SD) | 36.53±35.82 | 101. 50±86.91 | 0.0028 |
| AST, U/L (mean±SD) | 37.70±47.14 | 79.25±14.66 | 0.051 |
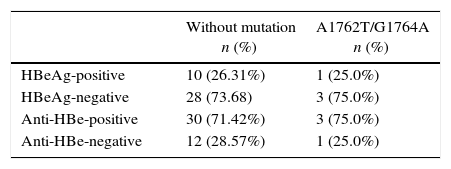
The HBeAg and anti-HBe were analyzed in 42 and 46 samples, respectively, including the four samples with the HBV A1762T/G1764A double mutation. According to the results shown in Table 4, the serological profile of samples with the HBV A1762T/G1764A double mutation was 25% HBeAg-positive, 75% HBeAg-negative, 75% anti-HBe-positive, and 25% anti-HBe-negative. Regarding the samples without the presence of the double mutation, they were 26.31% HBeAg-positive, 73.68% HBeAg-negative, 71.42% anti-HBe-positive, and 28.57% anti-HBe-negative. The rates of HBeAg and the anti-HBe were not significantly different.
Analysis of HBsAg and anti-HBe in samples from patients with chronic hepatitis B with and without the double mutation A1762T/G1764A.
| Without mutation n (%) | A1762T/G1764A n (%) | |
|---|---|---|
| HBeAg-positive | 10 (26.31%) | 1 (25.0%) |
| HBeAg-negative | 28 (73.68) | 3 (75.0%) |
| Anti-HBe-positive | 30 (71.42%) | 3 (75.0%) |
| Anti-HBe-negative | 12 (28.57%) | 1 (25.0%) |
HBV infection is a worldwide public health problem, even though it is a disease that can be prevented by vaccination. The presence of mutant viral strains may aggravate the disease; of note, the HBV A1762T/G1764A double mutant is associated to complications leading to the development of cirrhosis and/or HCC.2,31,32 The study of HBV and improvements of techniques to easily identify the HBV A1762T/G1764A double mutation as well as its correlation with biochemical and serological data can contribute to an improved understanding of hepatitis B.29,30,32
In this study, the serological data of the major antigens and antibodies related to HBV were analyzed together with the presence of the HBV A1762T/G1764A double mutation. All patients in this study were positive for the HBsAg for more than six months and were not using any antiviral therapy, therefore HBsAg reactivity was 100% as expected.
Other markers for hepatitis B are HBeAg, which indicates viral replication, while the antibody anti-HBe is an indicator of seroconversion. In this study, 74.41% of the samples were HBeAg negative and 71.73% anti-HBe positive, representing patients who had seroconverted. Other biochemical parameters were normal in most of the samples.
In the present study, there were four patients (8.16%) positive for the HBV A1762T/G1764A double mutant, as revealed by DNA fragments of 197pb and 110pb after incubation with Sau3AI enzyme. Of note, the 307pb DNA fragment was also observed in these samples, suggesting that HBV strains without this mutation was present in these patients together with the double-mutant strain. In fact, the double-mutant strain is usually found in very low levels in patients infected with HBV, a reason why most analyses fail to detect the mutant in these samples.29,32,33 Nonetheless, identification of the mutant is important considering its potential to increase the risk of cirrhosis and HCC.
HBV viral load was compared between samples with and without the HBV A1762T/G1764A double mutation, and no significant difference was found (p=0.43) probably due to the low number of samples with the HBV A1762T/G1764A double mutation. Nevertheless, studies suggest that the HBV A1762T/G1764A double mutation is directly related to increased viral replication and therefore the progression of liver disease.29,32,33
The aminotransferases (AST and ALT) were also analyzed in patients with and without the HBV A1762T/G1764A double mutation. For the AST parameter, there was no significant difference, but there was a clear trend for a significant difference (p=0.051). On the other hand, ALT levels were significantly higher in patients carrying the double mutant (p=0.0028). Given the results found here and in other studies, aminotransferases may be used as an indication for the possible presence of strains with the HBV A1762T/G1764A double mutation.29,30
The seroconversion of HBeAg to anti-HBe in samples with active viral replication is directly related to the presence of mutations in HBV in the BCP region, especially the HBV A1762T/G1764A double mutation. Usually the seroconversion process in patients with viral replication is associated with poor prognosis of the disease.34 In this study, seroconversion was observed in 75% of the patients with the HBV A1762T/G1764A strain; the patient that did not show seroconversion was the same that showed high viral replication according to his medical records.
The incidence of hepatitis B is relatively low in Porto Alegre, therefore a low number of patients could be enrolled in the present study. In addition, due to the lack of biochemical data in some patients’ electronic records, some parameters could not be analyzed for all patients. Another limitation was the difficulty in establishing a good molecular assay to detect the double mutant strain. Even though some studies have reported the use of real-time PCR (qPCR) to detect the A1762T/G1764A double mutation, most patients that carry the double mutant also have non-mutant strains, which are usually in higher concentrations; therefore, detection of the mutant strain is hamperd by non-mutant amplification products.35
In conclusion, in Southern Brazil HBV A1762T/G1764A double mutant strain circulates in low levels in patients with apparent seroconversion. This strain was associated with altered levels of ALT and seroconversion of HBeAg to anti-HBe in patients with liver disease. Considering that this strain has been associated with a higher risk of cirrhosis and/or HCC in patients with hepatitis B, it is important to verify the presence of this HBV double mutant in patients in the region.
Financial supportA.C.S. Souza and G.S. Marasca hold a fellowship from CAPES (Ministry of Education, Brazil). Ana B. Gorini da Veiga held a fellowship from CNPq (Productividade em Pesquisa) during the project
Conflicts of interestThe authors declare no conflicts of interest.
We thank the Graduate Program in Medicine: Hepatology at UFCSPA and the Hospital Nossa Senhora da Conceição (HNSC).