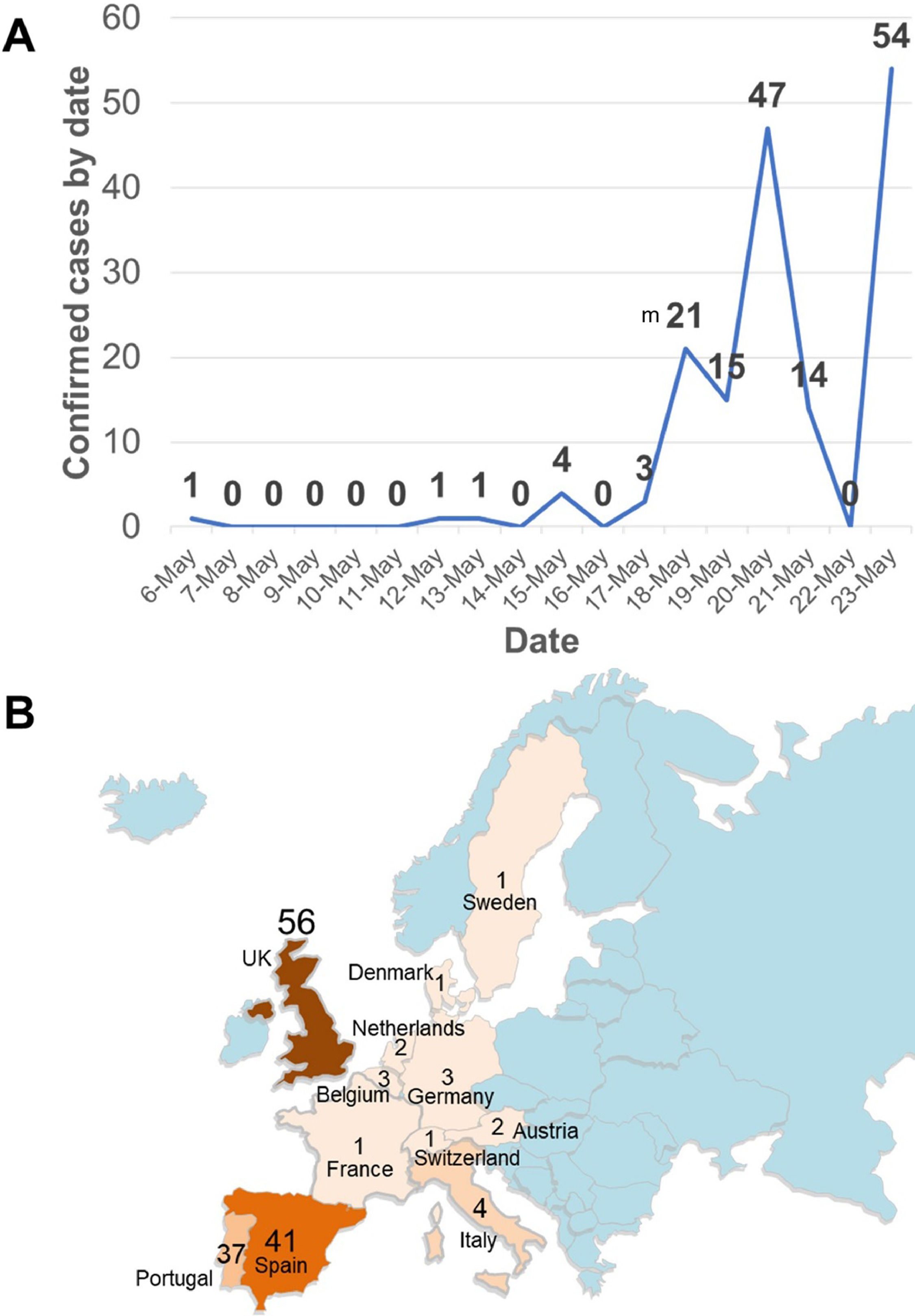
On May 13, 2022, the World Health Organization (WHO) was notified of two laboratory confirmed cases and one probable case of monkeypox, from the same household, in the United Kingdom. On May 14, 2022, four additional laboratory confirmed cases have been reported amongst Sexual Health Services attendees presenting with a vesicular rash illness in men who have sex with men (MSM). Based on currently available information, infection seems to have been locally acquired in the UK. The extent of local transmission is unclear at this stage and there is the possibility of identification of further cases.1 Nevertheless, other countries, especially in Europe, but also in North America, and other regions have reported suspected and confirmed cases so far, including recently suspected cases in Argentina and Colombia (Fig. 1). As occurred with COVID-19,2,3 travel would be a factor associated with some cases, as also previously reported for monkeypox.4
After two years of the COVID-19 pandemic, which has caused deep impact in Brazil and Latin America,2 reaching globally more than 525.7 million cases and 6.2 million deaths up to May 23, 2022. In Brazil alone, more than 30 million cases and more than 665 thousand deaths; a top question would be whether Latin America is prepared for a new viral zoonotic disease outbreak after SARS-CoV-2.5 A question that may have a complex answer, but undoubtedly, we are now, in 2022, in a better position to deal with monkeypox, than we were for COVID-19 in early 2020.6
With monkeypox, although is currently considered a self-limited condition in most of cases, previous studies in prairie dogs (animals considered important hosts of the virus after the 2003 USA outbreak involving six states and dozens of human cases), have showed that this DNA Orthopoxvirus may reach multiple organ and systems, including brain, heart, kidney, liver, lung, skin, spleen, thyroid, tongue, among others.7 Nevertheless, at least in humans, its viremia is considered low and short; consequently, blood sample is not an appropriate sample for laboratory diagnosis. Then, it is important to study carefully human cases and patients, sampling properly, multiple lesions and body fluids to assess the presence of the virus, its identification and hopefully genome sequencing of its DNA. An individualized clinical assessment of patients should be conducted. Although most of patients should evolve with mild disease, during the ongoing outbreak a child in UK has been admitted to the Intensive Care Unit (ICU) due to monkeypox. In recent times, the case fatality ratio has been around 3–6% (http://www.who.int/news-room/fact-sheets/detail/monkeypox). So far, in this current outbreak at least 22 confirmed cases have been hospitalized. Specially during the skin eruption period of disease (with the vesicular rash), isolation or quarantine of cases, should be considered. Currently, countries such as Belgium, have introduced a mandatory 21-day quarantine for Monkeypox patients as cases spread globally. As some experts indicate, testing and containing are the right measures to be implemented.
As expected, in countries such as Brazil and others in Latin America, the overlapping with other conditions of regional importance would be a differential diagnosis with Monkeypox, including Smallpox (eradicated in 1980), Cowpox (humans are susceptible), Chickenpox or varicella (a herpesvirus), measles (with recent outbreaks originated in Venezuela and disseminated to multiple countries in South America), syphilis (caused by the bacterium Treponema pallidum), the Peruvian wart or Oroya fever (Carrion's Disease, a Lutzomyia-borne disease caused by Bartonella bacilliformis), among others, especially in unvaccinated children for those preventable infections. We should even anticipate the possibilities of coinfection between monkeypox and other relevant conditions in the region (e.g. HIV). However, its impact in those with comorbidities including immunosuppressive conditions is still to be understood, in terms of epidemiological and clinical consequences.
Concerning laboratory capacity, Brazil and other Latin American countries have built up many skilled molecular biology and genome sequencing laboratories that routinely perform RT-PCR and phylogenetic studies, to diagnose Monkeypox once the primers and protocols are standardized in each reference site.
Neither vaccines nor drugs for monkeypox are yet available in Latin America. However, as the WHO is working to deploy monkeypox vaccines (licensed in 2019) and to reassess drugs previously evaluated for this reemerging virus, our countries will need to expedite their regulatory process to approve their use in each territory, probably and especially for the still rare, complicated cases. With monkeypox, as occurred with COVID-19, will be important to use only evidence-based treatments and interventions. Again, the advice by regional infectious diseases societies, after critical assessment of their utility will be key in the clinical guidance. Even more, as it was also showed during the COVID-19 pandemic, and discussed by our group,2,3 the political scenario has not been friendly for evidence-based decisions. That was mostly the situation in Brazil, Mexico, and Venezuela, among others where not scientifically supported interventions were recommended by high-rank stakeholders. Again, there is a need to broadly follow the recommendations of the WHO during this multi-country monkeypox outbreak.1–6
Latin America should be aware of the potential importance of monkeypox on arrival, enhance surveillance, diagnosis capabilities, and clinical and epidemiological research to better understand this reemerging viral zoonotic disease and its impact in the region and in their already vulnerable populations. Healthcare workers in the region should be aware of the geographic origin of suspected cases, particularly from European countries (Fig. 1).
FundingNone.