In this study, we evaluated trends in hospitalization rates, length of stay and in-hospital mortality in a cohort of HIV-infected patients in Rio de Janeiro, Brazil, from 2007 through 2013. Among the 3991 included patients, 1861 hospitalizations occurred (hospitalization rate of 10.44/100 person-years, 95% confidence interval 9.98–10.93/100 person-years). Hospitalization rates decreased annually (per year incidence rate ratio 0.92, 95% confidence interval 0.89–0.95) as well as length of stay (median of 15 days in 2007 vs. 11 days in 2013, p-value for trend<0.001), and in-hospital mortality (13.4% in 2007 to 8.1% in 2013, p-value for trend=0.053). Our results show that, in a middle-income setting, hospitalization rates are decreasing over time and non-AIDS hospitalizations are currently more frequent than those related to AIDS. Notwithstanding, compared with high-income settings, our patients had longer length of stay and higher in-hospital mortality. Further studies addressing these outcomes are needed to provide information that may guide protocols and interventions to further reduce health-care costs and in-hospital mortality.
Combination antiretroviral therapy (ART) has led to a reduction in the rates of hospitalization among HIV-infected patients.1,2 Immunological improvement and gain in life expectancy achieved as a result of ART also modified causes of hospitalizations, and, in most recent years, non-AIDS events surpassed AIDS-related as the main cause of hospitalization in high income settings.2–4 Simultaneously, duration of hospitalizations (i.e. length of stay) and in-hospital mortality1,5 among HIV-infected patients decreased over time. Nevertheless, there is a need to assess hospitalizations, length of stay, and in-hospital mortality in late ART era since they provide updated information on morbidity and health care utilization among HIV-infected patients, which are essential to evaluate health care provision, guide health policies and project its associated costs. In this study, we sought to assess trends in hospitalization rates, length of stay, and in-hospital mortality in a cohort of HIV-infected patients from Rio de Janeiro, from 2007 through 2013.
MethodsInstituto Nacional de Infectologia Evandro Chagas (INI, formerly known as Instituto de Pesquisa Clínica Evandro Chagas/IPEC) is a reference center for research and care of HIV-infected patients, in Rio de Janeiro, Brazil, since 1986. INI provides primary, specialty and tertiary care for HIV-infected patients and it includes an outpatient facility, an emergency department, a day-clinic, and an inpatient care unit (comprising an intensive care unit), all funded by the Brazilian National Health System. Patients followed at INI have free-of charge access to all available facilities. A longitudinal database maintains in-hospital and outpatient clinical information on patients receiving HIV care. Cohort procedures and results were published eslwhere.6,7
The present study included HIV-infected adults (≥18 years of age at cohort enrollment), enrolled in the INI cohort between 01 January 1986 and 01 December 2013, who were alive and in active care (at least one medical visit) after 01 January 2007. Follow-up started on 01 January 2007 or the date of cohort enrollment, whichever occurred last, and it ended on 31 December 2013, date of death, or last clinical visit (medical visit, CD4, HIV viral load or any blood exam) whichever occurred first. Lost to follow-up was defined as not having a clinical visit after 01 January 2013 for those known not to be deceased. Information regarding vital status was exhaustedly checked using the patients’ medical charts and by linkage with the Rio de Janeiro mortality database (up to 31 December 2013) using a previously validated algorithm.8
The primary cause of a hospitalization was inferred from discharge reports. All diagnoses listed in the discharge report were classified using the 10th Edition of the International Classification of Disease (ICD-10), into 24 different categories.9 Since some ICD-10 codes could be allocated to several categories, we considered a hierarchical classification protocol with a decreasing order of priority as follows: AIDS-events, non-AIDS malignancies, infections, and then systemic events.9 To determine the primary cause of a hospitalization, one or more ICD-10 codes listed in the discharge reports were hierarchically classified as follows: AIDS-defining diseases, non-AIDS cancer, cardiovascular disease, bacterial infections, fungal infections, viral infections, parasitic infections, digestive diseases, renal diseases, respiratory diseases, neurologic diseases, endocrine diseases, hematological diseases, psychiatric diseases, viral hepatitis, non-viral hepatitis, dermatological diseases, rheumatologic diseases, trauma, gynecologic disease, toxicities, others, and sings and symptoms.
Socio-demographic and clinical features were compared among included patients by study period (2007–2009, 2010–2011, 2012–2013) using Kruskal–Wallis test for continuous variables and Chi-square for categorical variables. Annual hospitalization rates, defined as the number of hospitalizations divided by the person-years (PY) of follow-up, were calculated per 100 PY; Poisson regression models were used to estimate trends in hospitalization rates. Length of stay (LOS) was calculated by subtracting hospital admission date from date of discharge and adding 1; linear regression models were used to estimate trends in LOS. In-hospital mortality, defined as the number of hospitalizations that ended in death divided by the total number hospitalizations, were calculated; logistic regression models were used to estimate trends of in-hospital mortality.
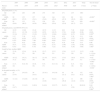
ResultsA total of 3991 patients, enrolled from June 1986 until November 2013, were followed from 01 January 2007 until 31 December 2013, accounting for 17,822 PY of follow-up. One hundred and eighty nine patients (4.7%) were deemed loss to follow up, yielding a loss to follow up rate of rate of 1.06/100 PY. The study population aged slightly through the years and the proportion of patients with 60 years or more increased from 5.1% in 2007–2009 to 7.1% in 2012–2013 (p<0.001, Table 1). Likewise, the median CD4 counts (419cells/mm3 in 2007–2009 to 542cells/mm3 in 2012–2013, p<0.001), the proportion of patients on ART (80.9% in 2007–2009 vs. 90.8% in 2012–2013, p<0.001) and the proportion of patients with a HIV viral load under 400copies/mL (54% in 2007–2009 vs. 69.5% in 2012–2013, p<0.001) significantly increased through the years.
Study population characteristics by study periods.
| 2007–2009 | 2010–2011 | 2012–2013 | p-Value | |
|---|---|---|---|---|
| (n=2639) | (n=3117) | (n=3605) | ||
| Sex | 0.678 | |||
| Male | 1699 (64.4) | 2020 (64.8) | 2359 (65.4) | |
| Female | 940 (35.6) | 1097 (35.2) | 1246 (34.6) | |
| Age in yearsa | ||||
| Median (IQR) | 41.7 (34.1, 48.6) | 42 (34.2, 49.4) | 42.5 (34.5, 50.5) | 0.004 |
| ≤30 | 372 (14.1) | 414 (13.3) | 466 (12.9) | <0.001 |
| 31–40 | 807 (30.6) | 925 (29.7) | 1051 (29.2) | |
| 41–50 | 885 (33.5) | 1065 (34.2) | 1124 (31.2) | |
| 51–60 | 440 (16.7) | 525 (16.8) | 709 (19.7) | |
| >60 | 135 (5.1) | 188 (6) | 255 (7.1) | |
| Race/ethnicity | ||||
| White | 1454 (55.1) | 1619 (51.9) | 1807 (50.1) | <0.001 |
| Non White | 1185 (44.9) | 1498 (48.1) | 1798 (49.9) | |
| Educational level | 0.075 | |||
| Up to 9 years | 1340 (50.8) | 1555 (49.9) | 1730 (48) | |
| More than 9 years | 1299 (49.2) | 1562 (50.1) | 1875 (52) | |
| HIV exposure category | 0.028 | |||
| Heterosexual | 1420 (53.8) | 1636 (52.5) | 1830 (50.8) | |
| MSM | 948 (35.9) | 1146 (36.8) | 1363 (37.8) | |
| IDU | 52 (2) | 50 (1.6) | 47 (1.3) | |
| Other/unknown | 219 (8.3) | 285 (9.1) | 365 (10.1) | |
| Chronic hepatitis Bb | 169 (6.4) | 188 (6) | 198 (5.5) | 0.308 |
| Chronic hepatitis Cc | 278 (10.5) | 301 (9.7) | 309 (8.6) | 0.03 |
| CD4 count (cells/mm3)d | ||||
| Median (IQR) | 419 (254, 616) | 532 (336, 772) | 542 (358, 775) | <0.001 |
| >500 | 970 (36.8) | 1664 (53.4) | 1924 (53.4) | <0.001 |
| 500–351 | 581 (22) | 554 (17.8) | 676 (18.8) | |
| ≤350 | 996 (37.7) | 801 (25.7) | 831 (23.1) | |
| Missing | 92 (3.5) | 98 (3.1) | 174 (4.8) | |
| HIV viral load (copies/mL)d | <0.001 | |||
| ≤400 | 1424 (54) | 2050 (65.8) | 2504 (69.5) | |
| >400 | 1073 (40.7) | 952 (30.5) | 956 (26.5) | |
| Missing | 142 (5.4) | 115 (3.7) | 145 (4) | |
| ART usee | 2136 (80.9) | 2687 (86.2) | 3273 (90.8) | <0.001 |
MSM, men who have sex with men; IDU, injectable drug use; ART, combination antiretroviral therapy.
During the study period, there were 1861 hospitalizations, yielding an overall hospitalization rate of 10.44/100 PY (95% confidence interval [CI] 9.98–10.93/100 PY). Hospitalization rates decreased annually (from 10.52/100 PY in 2007 to 7.28/100 PY in 2013, per year incidence rate ratio [IRR] 0.92, 95% CI 0.89–0.95) mainly due to a decrease of AIDS-related hospitalizations (from 5.17/100 PY in 2007 to 2.78/100 PY in 2013, per year IRR 0.88, 95% CI 0.84–0.92). Non-AIDS related hospitalization also decreased with a borderline significant trend (from 5.34/100 PY in 2007 to 4.49/100 PY in 2013, per year IRR 0.96, 95% CI 0.92–1.00; Table 2). Moreover, throughout the years the proportion of non-AIDS related hospitalizations gradually increased and accounted for the majority of the hospitalizations in the last three years of the study period. Bacterial infections (53.4%, n=507), cardiovascular diseases (18.6%, n=177), and viral infections (10.3%, n=98) represented the three most common causes on non-AIDS hospitalizations during the study.
Number of hospitalizations, hospitalization rates and length of stay, and in-hospital mortality, stratified by AIDS- and non-AIDS-related causes by year, 2007–2013, INI cohort.
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total | Test for trend | |
|---|---|---|---|---|---|---|---|---|---|
| Person-years | 1778 | 2057 | 2336 | 2556 | 2825 | 3040 | 3229 | 17,822 | p-Value |
| Hospitalizations, n (%) | |||||||||
| All causes | 187 | 284 | 290 | 274 | 320 | 271 | 235 | 1861 | |
| AIDS-relatede | 92 (49.2) | 152 (53.5) | 157 (54.1) | 148 (54.0) | 144 (45.0) | 128 (47.2) | 90 (38.3) | 911 (49) | <0.001a |
| Non-AIDS related | 95 (50.8) | 132 (46.5) | 133 (45.9) | 126 (46.0) | 176 (55.0) | 143 (52.8) | 145 (61.7) | 950 (51) | <0.001a |
| Hospitalizations, rate/100 PY (95% CI) | |||||||||
| All causes | 10.52 (9.11, 12.14) | 13.80 (12. 29, 15.51) | 12.42 (11.07, 13.93) | 10.72 (9.52, 12.07) | 11.33 (10.15, 12.64) | 8.91 (7.91, 10.04) | 7.28 (6.40, 8.27) | 10.40 (9.98, 10.93) | 0.92 (0.89–0.95)b |
| AIDS-relatede | 5.17 (4.22, 6.35) | 7.39 (6.30, 8.66) | 6.72 (5.75, 7.86) | 5.79 (4.93, 6.80) | 5.10 (4.33, 6.00) | 4.21 (3.54, 5.01) | 2.78 (2.27, 3.43) | 5.11 (4.79, 5.45) | 0.88 (0.84–0.92)b |
| Non-AIDS related | 5.34 (4.37, 6.53) | 6.42 (5.41, 7.61) | 5.69 (4.80, 6.75) | 4.93 (4.14, 5.88) | 6.23 (5.37, 7.22) | 4.70 (3.99, 5.54) | 4.49 (3.81, 5.28) | 5.33 (5.00, 5.68) | 0.96 (0.92–1.00)b |
| Length of stay, median (IQR) | |||||||||
| All causes | 15 (8, 25) | 15 (8, 27) | 14 (8, 26) | 15 (7, 26) | 12 (7, 21) | 12 (6, 21) | 11 (7, 20) | 13 (7, 23) | −1.00 (−1.54 to −0.47)c |
| AIDS-relatede | 19 (12, 31.2) | 19 (11, 30.2) | 19 (11, 33) | 21 (10, 36) | 18 (11, 31) | 15 (9, 26) | 16 (9, 25) | 18 (11, 31) | −0.92 (−1.78 to −0.06)c |
| Non-AIDS related | 11 (7, 22) | 9 (6, 19) | 10 (6, 16) | 9 (5, 17) | 8 (5, 14) | 8 (5, 16) | 8 (5, 16) | 9 (6, 16) | −0.65 (−1.26 to −0.04)c |
| In-hospital mortality, n (%) | |||||||||
| All causes | 25 (13.4) | 24 (8.5) | 30 (10.3) | 25 (9.1) | 19 (5.9) | 30 (11.1) | 19 (8.1) | 172 (9.2) | 0.92 (0.85–1.00)d |
| AIDS-relatede | 11 (12) | 13 (8.6) | 22 (14) | 19 (12.8) | 9 (6.3) | 21 (16.4) | 11 (12.2) | 106 (11.6) | 1.00 (0.90–1.12)d |
| Non-AIDS related | 14 (14.7) | 11 (8.3) | 8 (6.0) | 6 (4.8) | 10 (5.7) | 9 (6.3) | 8 (5.6) | 66 (6.9) | 0.84 (0.74–0.96)d |
PY, person-years; 95% CI, 95% confidence interval; IQR, inter-quartile range.
Per calendar year increase, incidence rate ratio and 95% confidence interval estimated using Poisson regression.
Per calendar year increase, linear coefficient and 95% confidence interval estimated using linear regression.
Following the trends of hospitalization rates, the overall LOS decreased significantly over the study period (median of 15 days in 2007 vs. 11 days in 2013, p-value for trend<0.001) as well as the LOS of non AIDS-related hospitalizations (median of 11 days in 2007 vs. 8 days in 2013, p-value for trend=0.038) and of AIDS-related hospitalizations (median of 19 days in 2007 vs. 16 days in 2013, p-value for trend=0.036). Overall, in-hospital mortality decreased during the study period (from 13.4% in 2007 to 8.1% in 2013, per calendar year increase odds ratio 0.92, 95% CI 0.85–1.00), as well as in-hospital mortality of non-AIDS related hospitalizations (from 14.7% in 2007 to 5.6% in 2013, per calendar year increase odds ratio 0.84, 95% CI 0.74–0.96). In-hospital mortality of AIDS related hospitalizations remained stable throughout the study period and, overall, it was 1.66 times higher than in-hospital mortality of non-AIDS related hospitalizations (11.6% vs. 7.0%, p<0.001; Table 2).
DiscussionIn this study, we have shown that among HIV-infected patients living in a middle-income setting in the late ART era, hospitalization rates have decreased through the years, mostly due to a decrease in the rate of AIDS related hospitalizations. Consequently, non-AIDS hospitalizations became more common than AIDS related in the last three years of the study period. Decreases in hospitalization rates in late ART era have been described for both high-4 and middle-income settings.10 This shift in hospitalizations causes (from AIDS related to non-AIDS related) follows the reduction in AIDS-defining diseases incidence11 and mortality12 already demonstrated in our cohort, highlighting an increased relevance of non-communicable events among HIV-infected patients. Changes in the study population characteristics through the study period have likely contributed to this scenario. Our results show that, over time, the cohort population aged, while CD4 counts, the proportion of virologic suppressed patients, and ART use among patients have increased.
LOS decreased throughout the study though it remained high mainly due to AIDS related hospitalizations. Overall, our estimated median LOS (13 days) surpasses the one reported for a US multicentric HIV study (median of 5 days)4 but is closer to that reported by a national Portuguese study (median 11 days).13 Additionally, similarly to other studies,4,14 we found that hospitalizations due to AIDS were associated with longer LOS (median of 9 vs. 18 days for non-AIDS and AIDS-related hospitalizations, respectively).
In-hospital mortality also decreased over the study period, although in-hospital mortality of AIDS-related hospitalizations remained quite stable through the years. In-hospital mortality was almost two times higher in AIDS-related hospitalizations than in non-AIDS-related hospitalizations. The overall 9.2% in-hospital mortality rate found in our study is higher than the 2.6% rate previously reported in a tertiary hospital in New York between 2004 and 2008,15 but is lower than the rate observed by Akinkuotu et al. in Malawi (24%).16
Disparities in hospitalization rates, LOS, and in-hospital mortality among the studies (particularly, when comparing high- vs. low- and middle-income settings) can be explained by several factors that range from hospital structure, hospital setting, type of health care system, as well as by the burden of diseases, in particular of AIDS-defining illnesses. In this context, tuberculosis burden might play a key role. In settings with high burden, tuberculosis is a leading cause of hospitalization among HIV-infected patients and is related to high in-hospital mortality (24.9% in a meta-analysis including 66 studies).17 In addition, tuberculosis is also associated with longer LOS both among the general and the HIV-infected population.18,19 In our study cohort, tuberculosis accounted for 43% of all AIDS related hospitalizations and yielded an in-hospital mortality of 10.9% (data not shown). Additionally, LOS of tuberculosis related hospitalization was significantly longer than non-tuberculosis hospitalizations (median of 18 days vs. 12 days, respectively, p<0.001, data not shown).
There are several limitations that need to be highlighted in the present study. First, our study casuistic is from a single cohort that has access to an outpatient as well as an infectious diseases hospital located in Rio de Janeiro, and our results may not reflect those for other HIV-infected populations in Brazil. Second, although patients have a free of charge access to Evandro Chagas hospital we cannot rule out the possibility of hospitalizations in other hospitals within the city, implying that our rates may have been somewhat underestimated. Finally, Evandro Chagas hospitalizations are restricted to non-surgical and non-obstetrics procedures, and therefore our rates do not represent the entire sort of events that can happen to an HIV-infected patient.
In summary, we demonstrated that, in a middle-income setting, hospitalizations rates are decreasing over time and that non-AIDS hospitalizations are currently more frequent than AIDS related ones. We also showed that in our setting we still struggle with long LOS and high in-hospital mortality. Studies addressing predictors of LOS and in-hospital mortality, mainly in low- and middle-income settings are needed and will be of utmost importance to guide health policies and assistance protocols in order to reduce health costs and in-hospital mortality.
FundingBG and PML acknowledge funding from the National Council of Technological and Scientific Development (CNPq) and the Research Funding Agency of the State of Rio de Janeiro (FAPERJ). This work was supported in part by the NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (leDEA) (U01AI069923).
Conflicts of interestThe authors declare no conflicts of interest.