The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has become a public health emergency, as it is a highly contagious disease, health services had to adapt to the high demand for hospitalizations in order to contain hospital outbreaks. We aimed to identify the impact of nosocomial transmission of severe acute respiratory coronavirus virus 2 among inpatients at a university hospital in São Paulo, Brazil. Among 455 inpatients diagnosed with coronavirus disease 2019 in March–May, 2020, nosocomial infection was implicated in 42 (9.2%), of whom 23 (54.7%) died. becoming routine, especially when community transmission occur with high levels of incidence. It was possible to observe with this study that the nosocomial transmission by SARS-CoV-2 was present even with these measures instituted, and some of the damages caused by these infections are intangible.
Transmission of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) occurs primarily through contact with respiratory secretions such as droplets.1 Aerosol transmission has been reported in situations that favor the dispersion of aerosolized particles.2 In-hospital transmission of SARS-CoV-2 has been reported at various institutions.3-7 In a prospective study of 1,353 health care workers in Singapore, Ran et al.6 found that 86 (6.4%) were infected with SARS-CoV-2, suggesting that the infections were hospital-acquired.
The objective of this study was to evaluate the impact of nosocomial transmission of SARS-CoV-2 among inpatients in Brazil. We evaluated patients hospitalized at a tertiary care teaching hospital—the Hospital São Paulo, operated by the Federal University of São Paulo, in the city of São Paulo, Brazil—between March 1 and May 31 of 2020.
To define cases of nosocomial transmission of SARS-CoV-2, we applied the criteria established by the Brazilian National Health Oversight Agency8: having been hospitalized with a diagnosis unrelated to infection with the target pathogen - SARS-CoV-2 - and having presented signs and symptoms or radiological findings consistent with the target disease—coronavirus disease 2019 (COVID-19) - or having tested positive for infection with the target pathogen - SARS-CoV-2 (by reverse-transcriptase polymerase chain reaction)—after day 14 of hospitalization or between days seven and 14 of hospitalization in case of close contact with an infected individual (health care worker, companion, or visitor) for more than 24 hours. Patients who were readmitted with signs and symptoms of COVID-19 within the first seven days after discharge were also evaluated.
This study was approved by the Research Ethics Committee of the Hospital São Paulo (Reference nos. 4,264,650 and 37048020.3.0000.5505). Because of the retrospective nature of the study, the requirement for written informed consent was waived.
During the study period, positivity for SARS-CoV-2 was identified, by reverse-transcriptase polymerase chain reaction, in respiratory secretions collected from 455 inpatients. Of those, 42 (9.3%) were considered cases of nosocomial transmission.
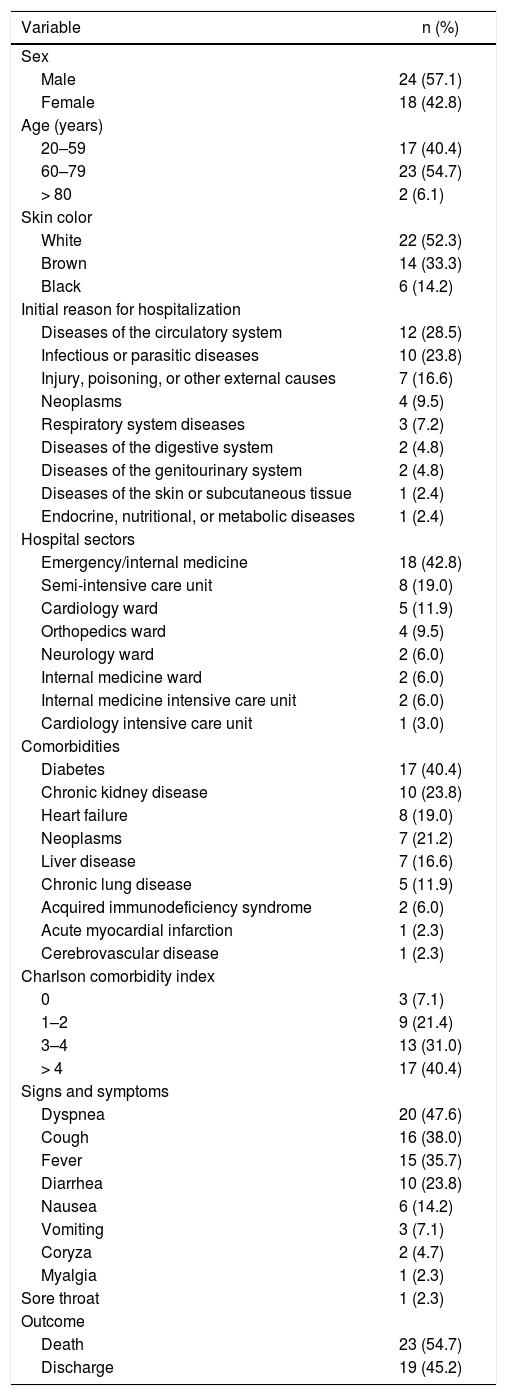
Among the 42 patients identified as cases of nosocomial SARS-CoV-2 infection, the mean age was 59 years (range, 23–86 years), 24 (57.1%) male and 22 (52.3%) self-reported their skin color as White.10 The main diagnoses that prompted admission were diseases of the circulatory system in 12 (28.5%), infectious and parasitic diseases in 10 (23.8%), and injury, poisoning, and certain other consequences of external causes in 7 (16.6%). The most affected hospital wards were the emergency/internal medicine ward, with 18 cases (42.8%), the semi-intensive care unit, with 8 (19.0%), and the cardiac intensive care unit, with 5 (11.9%).
Out of the 42 patients evaluated, the main comorbidities were diabetes, in 17 (40.4%), chronic kidney disease, in 10 (23.8%), and heart failure, in 8 (19%). We also calculated the Charlson comorbidity index, which was found to be 0 in 3 (7.0%) cases, 1–2 in 9 (21.4%), 3–4 in 13 (31.0%), and > 4 in 17 (40.4%).
In 69.0% (29/42) of the cases, SARS-CoV-2 infection was identified after day 14 of hospitalization, whereas in 13 (31.0%) it was identified between days 7 and 14. Of those, 69.2% (9/13) were tested because they had been in close contact with SARS-CoV-2-infected patients and 4 (30.7%) were tested after isolated outbreaks among the staff of the wards.
During the study period, 85.7% (36/42) of the patients with nosocomial infection were diagnosed with COVID-19 during their hospital stay. The mean time from admission to the onset of COVID-19 symptoms was 19.5 (8-129) days. Six patients (14.3%) were discharged and readmitted with symptoms of COVID-19 within seven days after discharge (mean, 3.8 days). Among those patients, the mean hospital stay during the first hospitalization was 21.6 (8–39) days and the mean time from discharge to symptom onset was 1.8 (1–3) days. In the 42 patients with confirmed nosocomial infection, the symptoms reported were dyspnea, in 20 cases (47.6%); cough, in 16 (38.0%); fever, in 15 (35.7%); diarrhea, in 10 (23.8%); nausea, in 6 (14.2%); vomiting, in 3 (7.1%); coryza, in 2 (4.7%); myalgia, in 1 (2.3%); and sore throat, in 1 (2.3%). Seven patients (16.6%) were asymptomatic. Supplemental oxygen was required in 25 (59.5%) cases. Twenty-six (62.0%) patients were treated in the intensive care unit, and mechanical ventilation was required in 15 (57.6%) of those patients. The mean stay at the intensive care unit was 14 (1–69) days and the mean time on mechanical ventilation was 9.5 (3-28) days. In 5 (15.1%) cases, the first symptom was acute respiratory failure, and the affected patients were promptly intubated. Twenty-three (54.7%) patients died. The mean time from the diagnosis of COVID-19 to death was 22 (1–88) days. Of the 23 patients who died, 9 (39%) had a Charlson comorbidity index > 4.
Despite preventive measures, nosocomial infections affect health care workers disproportionately. We identified nosocomial transmission of SARS-CoV-2 in 42 (9.3%) of the 455 inpatients diagnosed with COVID-19 during the study period. Other studies have reported similar rates.4,5,7 In Brazil, until May 31, 2020, 514,992 cases had been confirmed (2,437 cases per 1,000,000 inhabitants), 29,341 (5.7%) deaths, 206,555 (40%) cases recovered, according to official data released by the Ministry of Health. In the same period in São Paulo, 109,698 cases and 7,615 deaths were reported.9
We chose to define nosocomial transmission on the basis of the criteria established by the Brazilian National Health Oversight Agency,8 which defines cases as those occurring after day 14 of hospitalization or after day 7 if the individual has been in close contact with a confirmed case. Nishiura et al.11 found the mean incubation time in cases of nosocomial transmission to be 6.4 days. In other studies, cases of nosocomial SARS-CoV-2 transmission have been defined as those that occur after day 5 of hospitalization in patients hospitalized with a diagnosis unrelated to COVID-19,4,5 which could result in the inclusion of cases of community transmission, given the ≤ 14 day incubation period of COVID-19. In our sample, the reasons for hospitalization and the comorbidities reported at admission were similar to those reported in other studies,4 indicating that chronic diseases are potential aggravating factors for SARS-CoV-2 infection.
Few studies have investigated the possibility that the hospital ward were a patient is could be a risk factor. In all of the wards identified in the present study, there was considerable foot traffic, which made it difficult for us to identify sources of transmission.
In our sample, the most common symptom of COVID-19 was dyspnea, followed by cough and fever. Other studies have found the predominant symptoms to be fever, sore throat, nausea, and diarrhea.4,5,7 Our finding of asymptomatic cases supports evidence that < 50% of individuals infected with COVID-19 in the hospital environment are asymptomatic.11 However, it should be borne in mind that asymptomatic individuals are a major source of silent transmission. Therefore, the COVID-19 contact tracing process should include the contacts of asymptomatic individuals.
It is well known that comorbidities are risk factors for the severe form of COVID-19.4 In the present study, comorbidity rates (i.e., Charlson comorbidity indices) were highest among those who died.
Nosocomial SARS-CoV-2 transmission can be prevented through early identification of cases, diagnostic confirmation (by reverse-transcriptase polymerase chain reaction and imaging analysis), and better communication among hospital sectors, as well as precautions and isolation measures. It should be underscored the need for the hospital infection control team to establish daily communication sessions and provide continuing education on the use of personal protective equipment to prevent SARS-CoV-2 outbreaks. (Table 1)
Characteristics of Inpatients Infected Nosocomially with Severe Acute Respiratory Coronavirus Virus 2 (n = 42).