The main objective was to evaluate HBV infection and occult HBV infection (OBI) cases in mentally ill patients based on serological and molecular profiles.
Material and methodsSerum samples of 333 long-stay mentally ill patients were tested for the prevalence of HBV markers by serological (ELISA) and molecular (PCR) assays. The PCR products were sequenced to determine viral genotypes.
ResultsIt was observed a global prevalence of 12.9% (43/333) for HBV infection markers, considering HBsAg and/or anti-HBc positivity. Fourteen samples tested positive for anti-HBs alone. All samples positive (n=57) for any HBV serological markers were tested for HBV-DNA and six were positive: HBsAg/anti-HBc (n=1), anti-HBc/anti-HBs (n=1), anti-HBs alone (n=1), and anti-HBc alone (n=3). The rate of OBI was 9.2% (5/54) from samples that were anti-HBc and/or anti-HBs positive. All sequenced samples were characterized as genotype A.
ConclusionThe high rate of HBV infections found in this study suggests the possibility of HBV transmission due to risk factors displayed by some patients, and highlights the importance of vaccination of susceptible patients and the staff of that institution.
Hepatitis B virus (HBV) infection is a global public health issue. It is estimated that nearly two billion people worldwide have serological evidence of past or present HBV infection, whereas more than 240 million people, who are chronically infected, are at high risk of death from liver complications such as cirrhosis and hepatocellular carcinoma (HCC). According to the World Health Organization (WHO), more than 780 thousand people die every year as a consequence of acute or chronic HBV infection.1,2
The natural course of HBV infection is determined by the interactions between the host and the virus. Traditionally, clearance of HBV surface antigen (HBsAg) followed by positivity for anti-HBs is considered as infection recovery. Chronic HBV infection is characterized by the persistence of HBsAg. Therefore, HBsAg and anti-HBc total represent viral exposure markers while anti-HBs is a surrogate for immunity against HBV.3,4 Additionally, the use of molecular biology techniques in the diagnosis of hepatitis B has allowed the identification of occult HBV infection (OBI) by detection of viral DNA that may or may not be present in the serum of HBsAg-negative individuals.5,6
The clinical importance of OBI is that it constitutes a possible source of viral transmission. It has also been associated with the risk of disease reactivation during immunosuppression, and with progression to cirrhosis and/or HCC, since viral activity may determine a continuous inflammatory condition.7
OBI has been observed in the general population8 as well as in distinct groups such as blood donors,9 transplant recipients,10 and in HIV-infected individuals.11 Mentally ill patients are also at risk for HBV infection, especially because of their peculiar behavior.12,13 To our knowledge data on HBV occurrence among these patients are limited, and data on the literature have focused on prevalence of HBV infection.14–19
This study shows data on the serological and molecular profiles of HBV infection and OBI among long-stay mentally ill patients in a care center from Brazil.
Material and methodsStudy populationA total of 333 blood samples from the same number of mentally ill patients, including 121 males and 212 females, were collected between July 2011 and January 2012. The age of the study patients varied from five to 106 years old: 78.7% of patients were in the range 11–60; 3.0% had up to 10 years, and 18.3% were older than 60 years. Of all patients 68.8% had more than 10 years of stay time in the institution and only 15 had evidence of vaccination against HBV. These patients were institutionalized in a care center in the state of Goias, Brazil, where they received multidisciplinary care on the prevention, treatment, basic hygiene, and nutrition due to their partial or total dependence imposed by their disorders (physical, psychiatric, neurological).
A written consent was obtained from the day care center legal authority. The study was approved by the Ethics Committee of the Universidade Federal de Goiás (Protocol 182/11).
Detection of serological markersAll serum samples were tested by ELISA for the presence of anti-HBc (HEPANOSTIKA anti-HBc Uni-Form, bioMérieux, France), anti-HBs (ANTI-SURASE B-96 (TMB) (General Biologicals Corporation, Taiwan)), following the manufacturer's instructions. For HBsAg, two commercial EIA kits were used: SURASE B-96 (General Biological Corporation, Taiwan) and “HBsAg one” (DIA.PRO, Diagnostic Bioprobes SRl, Italy), both with high sensitivity (100%) and specificity (99.5%), according to the manufacturers.
HBV-DNA detectionSerum samples that were positive for any of the HBV serological markers were submitted to DNA extraction using phenol/chloroform20 and subjected to a semi-nested PCR amplification of the preS2/S genomic region. The test has sensitivity to detect three DNA molecules per assay, as previous described.21 The first round of amplification was performed using sense primer PS1 (nt 2826–2845) and two antisense primers S2 (nt 819–841) and S22 (nt 819–841). For second round, sense primer PS1 and antisense primer SR (nt 685–704) were used, generating a 1099 fragment base pairs. To avoid cross-contamination, all procedures were performed in different PCR cabinets, with UV light decontamination before and after each step. Samples with distinct serological profile were tested separately, for each reaction and a negative control was included. In order to confirm the DNA-HBV positive samples, all procedures were repeated. A second blood sample was also obtained from each positive patient and re-tested.
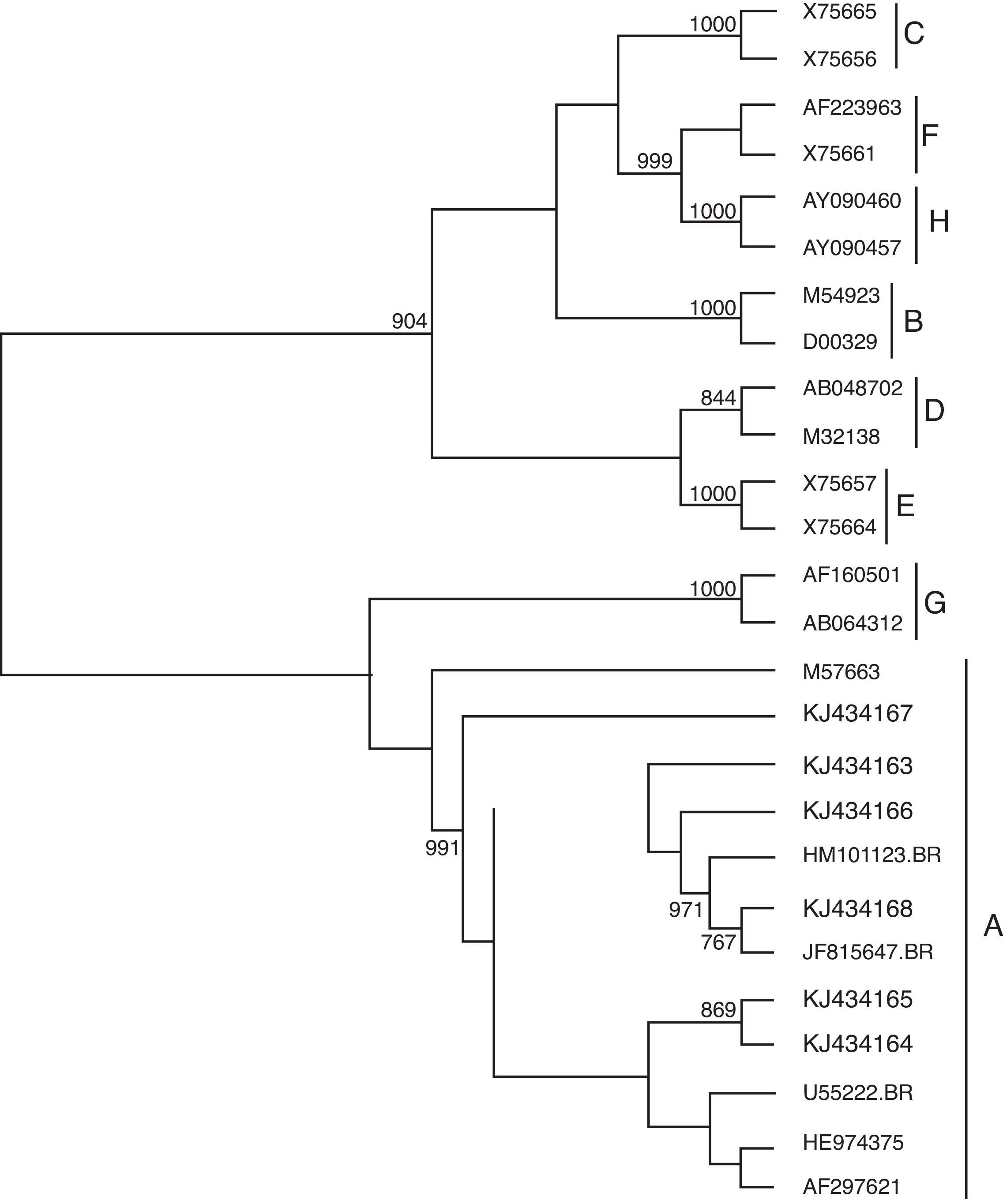
GenotypingThe PCR products were sequenced as previously described,22 using the second-round primers and the ABI Prism Big Dye Terminator 3.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA, USA). After purification using QIAquick PCR Purification Kit (Qiagen, Freigburg, Germany), samples were denatured and directly sequenced using an automated sequencer (ABI 3130 Genetic Analyzer – Applied Biosystems, Foster City, CA). The quality of each electropherogram was evaluated using Phred software,23 and the sequences were aligned by ClustalX software.24 The genotypes were identified by phylogenetic reconstructions using reference sequences from each HBV genotype obtained from GenBank, and the tree was generated using the neighbor-joining algorithm method.25 Genetic distances were determined by the Kimura-2-parameters method26 using the software MEGA v.5.0.27
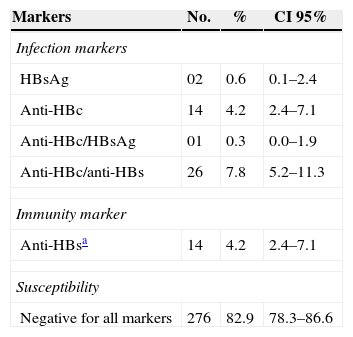
ResultsOut of 333 samples, 57 were positive for at least one HBV serological marker, which included two samples HBsAg positive alone, one HBsAg/anti-HBc, 26 anti-HBs/anti-HBc, 14 anti-HBc alone, and 14 anti-HBs alone (Table 1). Considering the exposure markers (HBsAg and/or anti-HBc) a global prevalence of HBV infection was 12.9% (43/333).
HBV serological markers in 333 long-stay mentally ill patients.
| Markers | No. | % | CI 95% |
|---|---|---|---|
| Infection markers | |||
| HBsAg | 02 | 0.6 | 0.1–2.4 |
| Anti-HBc | 14 | 4.2 | 2.4–7.1 |
| Anti-HBc/HBsAg | 01 | 0.3 | 0.0–1.9 |
| Anti-HBc/anti-HBs | 26 | 7.8 | 5.2–11.3 |
| Immunity marker | |||
| Anti-HBsa | 14 | 4.2 | 2.4–7.1 |
| Susceptibility | |||
| Negative for all markers | 276 | 82.9 | 78.3–86.6 |
Fifty-seven samples were screened for HBV DNA and six of them were positive, with distinct serological profiles: HBsAg/anti-HBc (n=1), anti-HBc/anti-HBs (n=1), anti-HBs alone (n=1) and anti-HBc alone (n=3). Only samples positive for anti-HBc and/or anti-HBs were considered OBI, and a rate of 9.2% (5/54) was observed.
Nucleotide sequencing was performed successfully in all DNA-HBV positive samples. Sequences with 511bp of the pre S2/S partial region (nt113–623) were considered for the comparative analysis, which showed identities values varying from 98 to 99% in relation to the Brazilian isolate U55222, and all of them were characterized as genotype A (GenBank accession numbers KJ434163–KJ434168) (Fig. 1).
Phylogenetic-tree of a partial region of pre-S/S2 region of HBV genome, with reference samples (GenBank) of all HBV genotypes and six isolates from the long-stay mentally ill patients from Brazil (represented in boldface). Bootstrap values (2000 replicates) are shown at the branch nodes; values lower than 80% are not shown.
The participants of the study were diagnosed as mentally ill, associated or not to a physical disorder. Mentally inpatients are at risk for HBV infection due to the special behavior that they present.12,13 These individuals may share personal hygiene objects, such as tooth brushes and raisers. They may also behave aggressively, which could potentially result in minor abrasions or even lesions. Some are immune compromised in addition to their mental problem.28 Furthermore, institutionalization may also increase the risk of HBV transmission29 that appears to be mediated by both prolonged contact between inpatients and behavior due to mental and physical disabilities.
A rate of 12.9% for HBV infection was observed in this study population by serological methods. These data corroborates other studies16,18 although higher rates have been found in previously published studies.14,28,30–32 Our data also revealed a 9.2% (5/54) rate of OBI, reinforcing the notion that HBV infection is underestimated when HBV DNA is not tested in cases in whom the infection is assumed to be resolved (HBsAg negative, anti-HBc and/or anti-HBs positive cases).
The prevalence of OBI varies according to geographical regions as well as distinct populations. The OBI profile has been reported in different regions around of the world with rates ranging from 0% to 50% in healthy patients and blood donors.33–35 It has also been reported in 30–95% of at-risk individuals such as chronic hepatitis C patients.36,37 Considering the OBI data in mentally ill inpatient population, only one study was conducted with similar population in Brazil, which detected HBV-DNA in 13.4% of HBsAg negative samples.14
Among inpatients with OBI it is possible to observe differences in the serum markers profile.5,38,39 Some studies have shown that in general anti-HBc and/or anti-HBs markers are present, however about 20% of patients are negative for both markers.40 In this study, only positive patients for HBV markers were tested for HBV DNA, therefore the rate of OBI could have been underestimated.
Although the anti-HBc/anti-HBs profile is indicative of viral clearance and immunity, when in association with viral DNA positivity it is considered a case of persistent infection.41,42 On the other hand, presence of anti-HBs does not always mean protection against HBV infection, considering the circulation of HBV mutants, for which the anti-HBs antibodies elicited by the HBV vaccine may not be able to exert their neutralizing activity. This fact could explain the occurrence of HBV infection in vaccinated individuals,43 as observed in one inpatient, who was positive for anti-HBs and HBV DNA (Fig. 1 – accession number KJ434164).
Of the patients, only 4.2% were positive for anti-HBs alone (immunity marker), and 82.9% were susceptible to infection. The number of infected individuals (HBsAg and/or DNA positive) highlights the facilitation of the virus transmission in the institution.
The HBV-DNA positive samples were characterized as genotype A (Fig. 1). This genotype has a global distribution and in Brazil it is the most prevalent, followed by genoypes D and F.44–47 It has been suggested that acute infection with HBV genotype A may increase the risk of progression to chronic disease.48,49 Despite the risk factor associated with HBV transmission that the patients may present, the phylogenetic analysis carried out with DNA sequences of six samples showed that they were not identical, indicating no HBV transmission among these patients.
Finally, studies on HBV prevalence that use methodologies that allow for the identification of serologic profiles as well as the presence of viral DNA are essential for identifying infected people in order to minimize complications arising from HBV infection and also to help decreasing viral dissemination.
The presence of occult infection among long-stay mentally ill patients is worrying considering not only the possibility of progression to cirrhosis and carcinoma but also because it may cause viral transmission, due to the living conditions of the individuals. Therefore our data underscores the need for periodic monitoring of inpatients for the possibility of viral transmission and reinforce the importance of the adoption of preventive vaccination against HBV of inpatients and staff.
FundingThis study was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – Brazil) process number 481059/2010-5.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank CNPq for financial support.