Several tests are performed to obtain better accuracy when diagnosing American tegumentary leishmaniasis (ATL). It is believed that antigens released via secretion, excretion and metabolism are more specific than are antigens released by the lysis of Leishmania parasites. Such antigens are known as exo-antigens (exo-Ag) and are formed from products released by cultured parasites in a way that is similar to that in which they cause infections in hosts.
ObjectiveWe attempted to validate a Leishmania mexicana ELISA exo-Ag for ATL diagnosis in Midwestern Brazil.
MethodsA total of 281 patients were included in the study. We analysed pre-treatment blood from 98 ATL patients; out of those, 85.7% and 14.3% had cutaneous and mucosal forms, respectively.
ResultsThe exo-Ag accuracy was 83.99% (95% CI=79.24–87.81) with a sensitivity value of 90.82% (95% CI=83.46–95.09) and an overall specificity value of 80.33% (95% CI=73.97–85.44). The positive predictive value and negative predictive value were 71.20% (95% CI=62.72–78.41) and 94.23% (95% CI=89.40–96.94), respectively. Among healthy controls, exo-Ag had a specificity of 91.25% (95% CI=83.02–95.70); additionally, the test had specificity rates of 66.67% (95% CI=46.71–82.03) in Chagas disease patients, 60.61% (95% CI=43.68–75.32) in patients with rheumatic diseases, 76.92% (95% CI=49.74–91.82) in pemphigus foliaceus patients, 87.50% (95% CI=52.91–97.76) in leprosy patients, 87.50% (95% CI=63.98–96.50) in VRDL-positive patients, and 77.78 (95% CI=45.26–93.68) in deep mycosis patients.
ConclusionBased on the indicators of validity, we conclude that the results obtained in this study enable the recommendation of the exo-Ag ELISA for ATL diagnosis once it presented a reasonable accuracy compared to classical methods. Cost evaluations are necessary to completely define the role of this technique in large scale.
American tegumentary leishmaniasis (ATL) is an infectious and difficult-to-control disease that is caused by parasites of the genus Leishmania. ATL causes considerable socioeconomic losses, as it affects subjects at their most productive ages.1
Several complimentary tests are used to diagnose ATL, all of which have limitations. The diagnostic tests include parasite detection techniques (e.g., direct examination, cultures, histopathological examinations and PCR) and immunodiagnostic techniques (e.g., cellular immune response detection, including the Montenegro skin test (MST), antibody detection, including the fluorescent antibody test (IFAT), ELISA, and immunocomplex antigen detection).2,3 Serological tests have been given considerable importance in epidemiological investigations. However, for diagnostic purposes, those methods can be associated with a relatively high proportion of false-positive results.
ELISAs have a great advantage among other serological tests because of their higher specificity. In addition to quickly generated results, ELISAs are also relatively low-cost tests.4,5 The antigens most commonly used in leishmaniasis diagnostic immunoenzymatic assays are obtained from intact parasites. The sensitivities of these assays fluctuate between 85% and 100% for crude antigens.6 Crude antigens from Leishmania (Leishmania) amazonensis and Leishmania (Viannia) braziliensis, when separated by electrophoresis and subjected to Western blotting, can be recognized by sera from patients with Chagas disease.7 This phenomenon is believed to occur because of interactions with Trypanosoma and Leishmania common antigens.8
On the other hand, it is believed that antigens released via secretion, excretion and metabolism are more specific than are antigens released by the lysis of Leishmania parasites.9,10 Such antigens are known as exo-antigens (exo-Ag) and are formed from products released by cultured parasites in a way that is similar to that in which they cause infections in hosts.11 An ELISA with Leishmania (Leishmania) mexicana (L. mexicana) promastigote antigens, used to detect IgM and IgG antibodies in sera from Brazilian Leishmania-infected patients, had a sensitivity of 92.3% and was reactive when tested in 10 patients with ATL via Western blotting.12
ELISA with an exo-Ag from Leishmania parasites cultured in protein-free medium is thought to be an improved method with increased accuracy; therefore, we intended to validate this technique for ATL diagnosis in Midwestern Brazil.
Materials and methodsThis study was conducted from August 2007 to July 2010 at the Hospital Universitário de Brasília, Brasília, Brazil, a reference centre for ATL in Midwestern Brazil. Ninety-eight consecutive patients with cutaneous (CL) and mucocutaneous (MCL) disease forms, who were specific treatment naive during the previous six months, were included in a cross-sectional study for diagnostic test accuracy.
ATL diagnosis was performed according to a previously validated composite reference standard formed by clinical and laboratory criteria (direct examination, culture, histopathological examination, PCR from lesion fragments, MST and IFAT).13Leishmania subgenus identification was performed at the Laboratory of Dermatology, Hospital das Clínicas, University of São Paulo, Ribeirão Preto, Brazil, using restriction fragment length polymorphism (RFLP) as described elsewhere.13
Additionally, the study included a convenience sample of 80 healthy patients with no epidemiological history of leishmaniasis, 24 patients with Chagas disease, 13 patients with American pemphigus foliaceus, 8 patients with lepromatous leprosy, 9 patients with deep mycosis, 16 VRDL-positive patients at a minimum dilution of 1:8, and 33 patients with rheumatic disease who were positive for at least one rheumatic marker test, including anti-streptolysin O (ASO), C-reactive protein (CRP), and rheumatoid factor (RF).
SamplingTwo millilitres of patient serum, obtained through venipuncture, was used. After clot retraction, the samples were centrifuged and stored in labelled tubes at −20° C until the ELISA exo-Ag analyses were performed.
L. mexicana exo-antigen ELISAA manufactured kit was used for the ELISA reactions. The kit, developed by the Cellabs laboratory (Brookvale, Australia), contained the following components: one ELISA plate with 12 detachable strips, each of which contained eight wells pre-coated with Leishmania exo-antigens; one vial of washing buffer (PBS-Tween, 20× concentrate); one vial of peroxidase-conjugated anti-human IgG (100× concentrate); one vial of substrate (20× concentrate); one vial of substrate buffer; one vial of stop solution; one vial of positive control serum; and one vial of negative control serum.
The patients’ sera and the positive and negative controls were diluted 1:200 in the washing solution and pipetted into an ELISA plate that had been pre-coated with L. mexicana secretory, excretory, and metabolic antigens. The plate was subsequently incubated for 60min in a humid chamber. After washing the plate four times with PBS plus Tween 20 (0.05%), the peroxidase-conjugated anti-human IgG (diluted 1:100 in washing solution) was added to the plate. Next, the plate was incubated again for 30min at room temperature, and the plate was washed four more times with PBS-Tween. One millilitre of chromogenic substrate (TMB) pre-diluted in substrate buffer was added to the wells, and the plate was immediately covered with aluminium foil. After a 30-min incubation at room temperature, 100μL of stop solution (H2SO4) was added to each well. The reactions were observed with an ELISA reader (Spectramax Plus, Molecular Devices LLC, Sunnyvale, CA, USA) that was fitted with a 450/620-nm absorbance filter.
Samples with absorbance values above the cut-off point (0.3%; above the grey zone) were considered positive. The ELISA reactions were performed and results were evaluated by a specialized biomedicist who was blind to the real condition of patients included.
Sample sizeThe sample size was calculated based on the hypothesis test for a proportion, available in Epi Info version 3.3.2 (CDC, Georgia, USA) software. According to the sensitivity of ELISA tests for ATL in previously published studies,12,14 considering a confidence level of 95% and an absolute precision of 5%, the number of patients to be included for serological tests was defined as 73 patients and 73 controls.
Statistical analysisThe test properties (sensitivity and specificity values, the positive predicted value, and the negative predicted value, and accuracy) were evaluated using OpenEpi® version 3.01 (Emory University, Rollins School of Public Health, Atlanta, Georgia, USA). Confidence intervals were set at 95% (95% CI).
This study was approved by the Ethics in Research Committee of the College of Medicine – University of Brasília – UnB (Process number 046/2007). All patients included signed the informed consent form and the study was in accordance to the Declaration of Helsinki, as revised in 2013.
ResultsEpidemiological and clinical aspectsNinety-eight ATL patients were included, of whom 67.4% were men and 32.6% were women; 70.4% patients had only one skin lesion, while 22.4% had two-four lesions and only three (3.1%) had five or more skin lesions. Regarding the clinical disease forms, 85.7% had CL, while 14.3% had MCL. Additionally, 81.6% of the patients had initial infections, while 12.2% had recurrent disease, and no information was available for six patients.
When assessing the sensitivity of the composite reference standard tests, MST was the most sensitive (88.5%), followed by PCR (75.9%) and IFAT (73.1%) (Table 1). RFLP-PCR was performed for samples obtained from 58 patients (Table 1). The subgenera Viannia was identified in 95.5% of the 44 positive samples, and the subgenera Leishmania was identified in two patients (4.5%).
Sensitivity of assays used to diagnose samples from 98 patients with American cutaneous leishmaniasis who were treated at the University Hospital of Brasília from August 2007 to July 2010.
| Result | Culture | DE | IFAT | MST | PCR | HE | Exo-Ag ELISA |
|---|---|---|---|---|---|---|---|
| Positive | 47 | 45 | 68 | 62 | 44 | 19 | 89 |
| Negative | 43 | 46 | 24 | 8 | 14 | 73 | 9 |
| NP | 8 | 7 | 6 | 28 | 40 | 6 | 0 |
| Sensitivity | (52.2) | (49.5) | (73.9) | (88.5) | (75.9) | (20.7) | (90.8) |
NP, exam not performed; DE, direct examination; IFAT, immunofluorescence antibody test; MST, Montenegro skin test; *HE, histopathological examination with the presence of amastigote forms.
The exo-Ag ELISA overall accuracy was 83.99% (95% CI=79.24–87.81) with a sensitivity value of 90.82% (95% CI=83.46–95.09) and an overall specificity value of 80.33% (95% CI=73.97–85.44). The positive predictive value and the negative predictive value were 71.20% (95% CI=62.72–78.41) and 94.23% (95% CI=89.40–96.94), respectively.
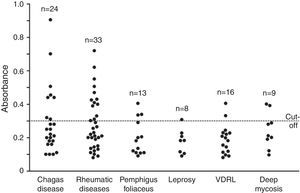
The exo-Ag ELISA specificity varied according to the group studied: healthy patients, patients with other diseases, and also in VDRL-positive sera (Table 2). Fig. 1 shows the exo-Ag ELISA reaction results for the groups of patients with other diseases and in VDRL-positive sera (minimum cut-off value, 0.3) (Fig. 1). The exo-Ag ELISA showed false positive results in 13 of the 33 patients with rheumatic diseases (Table 3).
Leishmania mexicana exo-Ag ELISA specificity according to the group of control subjects evaluated.
| Group | Samples (n) | False positive (n) | Specificity: (95% CI)a |
|---|---|---|---|
| Healthy subjects | 80 | 7 | 91.25 (83.02–95.70) |
| Chagas disease | 24 | 8 | 66.67 (46.71–82.03) |
| Pemphigus foliaceus | 13 | 3 | 76.92 (49.74–91.82) |
| Leprosy | 8 | 1 | 87.50 (52.91–97.76) |
| Deep mycosis | 9 | 2 | 77.78 (45.26–93.68) |
| VRDL-positive patients | 16 | 2 | 87.50 (63.98–96.50) |
| Rheumatic diseases | 33 | 13 | 60.61 (43.68–75.32) |
| Total | 183 | 36 | 80.33 (73.97–85.44) |
Results of Leishmania mexicana exo-Ag ELISA among 33 rheumatic disease patients, testing positive for at least one rheumatic marker.
| Rheumatic marker | ELISA with Leishmania mexicana exo-antigens results | (n) | Specificity (95% CI) |
|---|---|---|---|
| ASO | Positive | 3 | |
| Negative | 9 | ||
| CRP | Positive | 6 | |
| Negative | 7 | 60.61 | |
| RF | Positive | 4 | (43.68–75.32) |
| Negative | 4 | ||
| Total | 33 | ||
ASO, anti-streptolysin O; CRP, C-reactive protein; RF, rheumatoid factor.
Parasite detection methods are recommended as a way to achieve an accurate diagnosis. Given the low sensitivity of these tests, immunological techniques such as ELISA, IFAT, and MST have also been employed. The exo-Ag ELISA test has been studied as a potentially better option for ATL diagnosis.
Direct examination sensitivity ranges from 14 to 89.7%, depending on the parasite species and the disease evolution period.13 Parasite cultures from ATL patients also yield low and variable positivity rates (28.6–89%).13,15,16 Additionally, the limitations of this technique, including bacterial and fungal contamination and delays to provide the final result (up to 30 days), should be taken into account.
PCR is considered as the most accurate method for ATL.3 However, a variable sensitivity is expected depending on the specific technique used. Our results are aligned with previous data and confirm that Leishmania (Viannia) braziliensis is the most frequent species in the region studied.16–19 Similar to other techniques for immunologic tests in leishmaniasis, such as the MST,13 the decision of using L. mexicana antigens for the ELISA tests is based on the fact that parasites of the Leishmania subgenus are more easily managed in laboratory experiments and grow faster in culture media. This action can have an important impact on cost reduction when considering its reproduction on larger scale.
The exo-Ag ELISA performed well by exhibiting a higher sensitivity than did the IFAT, another highly sensitive serological method that may present highly variable results, with rates ranging from 34 to 82.9% (Table 1).14,20 Additionally, the IFAT has other disadvantages such as not being suitable for automation, high cross-reactivity in patients with Chagas disease, paracoccidioidomycosis, pemphigus foliaceus, and some deep mycoses.21 All those diseases are considered endemic in some parts of South America, especially in Midwestern Brazil.3,22
The exo-Ag ELISA showed similar results when compared to the index of positive tests obtained by other authors with different antigens. The exo-Ag ELISA sensitivity values were close to those of tests that satisfactorily used chromatography-purified antigenic fractions.23,24 As an antigen, the intact parasite contains membrane glycoproteins that act as powerful epitopes due to constant exposure to the host immunological system. Despite comprising glycoproteins that are not present on the parasite membrane, the exo-Ag ELISA sensitivity was similar to that of immunoenzymatic assays that used intact promastigotes.25
The exo-Ag ELISA specificity was not perfect in a control group of apparently healthy patients with no epidemiological history of ATL (Table 2). Although they do not fulfil the composite reference standard for the definition of ATL, it is not possible to completely rule out subclinical Leishmania infections once the disease is presenting a growing incidence in otherwise free areas, such as periurban regions. Other subclinical diseases that could produce nonspecific antibody binding should also be considered.7,26
The specificity was moderate when Chagas patients’ sera were tested (Table 2). Studies have shown that the specificity values for Chagas disease range from a total lack of specificity27 or low values such as 5.5%28 to values as high as 83.33%.24 The latter study used purified glycoprotein antigens that were less likely to cause nonspecific reactions. However, the challenge of cross-reactivity with other trypanosomatids remains and is likely due to the presence of antigenic determinants with similar structures.8,29 Therefore, it is necessary to purify the exo-Ag ELISA antigens in order to improve the test specificity against other parasitic diseases such as Chagas disease.
When the serum samples of patients with rheumatic diseases were studied, substantial numbers of nonspecific reactions were observed in all sera in which rheumatic markers were present (Table 3). We highlight the C-reactive protein that presented a considerable number of false positive results. This protein is present in patients with inflammatory conditions as a result of classical pathway activation, which relies on the presence of immunoglobulins. These immunoglobulins seem to exhibit nonspecific behaviours in these patients, which would explain the high exo-Ag ELISA cross-reactivity.
In samples from patients with deep mycoses, two reactions with absorbances above the cut-off value were observed in sera from patients with sporotrichosis. ATL can be mistaken for sporotrichosis either by clinical manifestations or by immunological test cross-reactions, and therefore the differential diagnosis between these two infections is relevant.30 It is also important to remember the possibility of co-infection by Sporothrix schenkii and Leishmania, as described previously.31
It should be pointed out that the use of L. mexicana antigens, a species not endemic in Midwestern Brazil, can result in higher frequency of false positive and false negative results. However, as previously stated, the relative difficulty in managing Leishmania (Viannia) braziliensis can be an obstacle for species-specific antigens production. By observing the occurrence of nonspecific reactions, we can note the need to study immunoenzymatic reactions with L. mexicana exo-antigen antigenic fractions. Additionally, we might suggest the separation of the proteins that comprise L. mexicana exo-antigens for using in immunoblot tests with sera from patients with other diseases, in order to identify the less reactive bands that provide higher specificities.
Based on the indicators of validity, we conclude that the results obtained in this study allow for the recommendation of the exo-AG ELISA for ATL diagnosis once it presented a reasonable accuracy compared to classical methods. Cost evaluations are necessary to completely define the role of this technique on large scale.
FundingFundação de Amparo à Pesquisa do Distrito Federal; FAP/DF (Process 193.000.332/2007) and Conselho Nacional de Pesquisa; CNPq) (Process 478575/2008-4).
Conflicts of interestThe authors declare no conflicts of interest.
We thank the preceptors and residents of the Dermatology Service of University Hospital of Brasília, the technicians of the Dermatomycology Laboratory of UnB, and Tércio Rodrigues Pereira, Viviane Medeiros da Costa, and Professor Pedro Luis Tauil.