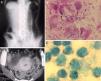
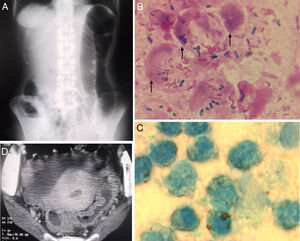
A 57-year-old woman visited to our hospital because of low-grade fever, vague lower abdominal discomfort and frequent small amount of blood-stained mucus with tenesmus for three weeks. She suffered from occasional severe abdominal cramping, and felt severe tenderness in anal canal on rectal examination, suggesting of proctitis. Laboratory findings were normal except for the elevation of CRP (3mg/dL). Supine abdominal X-ray showed narrowed colon and loss of haustration so-called “lead-pipe colon”, which was consistent with repeated mucosal inflammatory process (Fig. 1A). Immediate examination of her mucus by Gram stain (Fig. 1B, arrow) and methylene blue stain (Fig. 1C) showed no bacterial pathogens but many fecal leukocytes, implicating of inflammatory bowel disease. Abdominal CT showed the severe mucosal thickening in the rectum, sigmoid colon (Fig. 1D) and other entire large intestine. By performing colonoscopy, she was diagnosed with total colonic type ulcerative colitis. The fecal leukocyte test is a safe, quick and easy test to explore the chronic inflammatory or infectious process in digestive tract.1,2 The present case reminds us the fact that the presence of fecal leukocytes is a clinical clue to the diagnosis in patients with chronic diarrhea such as ulcerative colitis and Crohn's disease, especially in outpatient settings.2
The authors declare no conflicts of interest.