Highly active antiretroviral therapy (HAART) has significantly improved survival of people living with HIV/Aids (PLWHA). However, poor treatment adherence to HAART and other problems, still cause therapy failure and contribute to increased morbidity and mortality of PLWHA. In this retrospective cohort study (2013–2015), we sought to evaluate the factors associated with mortality of PLWHA failing HAART in 2013, who were receiving care at a reference center for sexually transmitted diseases (STD) and HIV/AIDS. A total of 165 individuals over 18 years of age who were failing antiretroviral therapy were evaluated. In two-year follow-up, 19 (11.5%) deaths were documented. There were a significant association between mortality and report of illicit drug use (53%, p < 0.01), being attended by a larger number of medical professionals (6.3 ± 3.2, p = 0.02), use of firstline non-nucleoside reverse transcriptase inhibitor (74%, p = 0.01), and history of interrupting HAART ≥3 months (90%), p = 0.02). Patients who died had a significantly higher viral load (mean 49,192.4 ± 35,783.6 copies/mL) than survivors (26,389.2 ± 27,416 copies/mm3, p < 0.01), lower mean CD4 cell counts (127.8 ± 145.6 cells/mm3 vs. 303.3 ± 202.4 cells/mm3, p < 0.01), and higher frequency of previous virologic failure (89% vs. 74.7%, p < 0.01). Our results reinforce the importance of early detection and prevention of virologic failure, to reduce the mortality associated with this event.
In 2017, UNAIDS (Joint United Nations Programme on HIV/AIDS) reported the existence of 36.9 million people living with HIV.1 In Brazil, 136,945 cases of HIV infection were reported between 2007 and June of 2016.2 In the same period, the state of Bahia, the most important economy in the Northeastern region, reported 5433 new cases of HIV.3 In the last 10 years, the Northeastern region presented a 34.3% increase in the mortality coefficient, from 3.2 to 4.3 deaths for 100,000 inhabitants.2
In December of 2013, Brazil became the world’s third country to recommend immediate start of highly active antiretroviral therapy (HAART) for people living with HIV/Aids (PLWHA), regardless of CD4 T lymphocyte count. Early treatment of HIV infection may improve quality of life of PLWHA and reduce the risk of virus transmission of HIV patients. However, issues related to adherence to therapy, medication tolerability, and lack of access to health care for PLWHA can increase the risk of virologic failure.4
Advances over time with HAART have resulted in decreased virologic failure rates. However, irregular use of HAART may select viral strains with mutations that allow the maintenance of HIV replication. In this setting, a new antiretroviral regimen is required for an effective treatment. The test used to detect resistance is HIV genotyping, which is not systematically recommended by the Brazilian public health care guidelines. Virologic failure is often associated with progressive increase of HIV viral load, decrease of CD4 T cell count, and progression of opportunistic disease. All these markers are directly associated with higher probability of death.4 Poor adherence to HAART and other problems contribute to therapy failure and increased morbidity and mortality of PLWHA.
In this study, we sought to evaluate the factors associated with mortality of PLWHA failing HAART in 2013.
This was a retrospective cohort study involving PLWA followed at the State Reference Center for Diagnosis, Care and Research (CEDAP), the largest reference center for the treatment of PLWHA, in the city of Salvador, Brazil, where 3500 patients are on therapy. To be included, patients must be over 18 years of age, with a confirmed diagnosis of HIV infection, and presenting virological failure in the period from January to December 2013. Eligible subjects were prospectively followed until December 2015. Sociodemographic, behavioral, clinical, and laboratory data were obtained from clinical records and pharmacy reports of antiretroviral therapy (ART) and in the following databases: (a) Internal Registration CEDAP Laboratory data — CompLab; (b) Logistics Management System Drugs — SICLOM; (c) System Laboratory Tests Control of the National Network of Lymphocyte Count CD4/CD8 and viral load — SISCEL; and (d) Brazilian Information System on Mortality — SIM.
Virological failure was defined as detectable HIV RNA above 1000 copies/mL (Abbot molecular, Illinois, USA) in individuals on ART for at least six months. Information on death was obtained from SIM. The survival time was calculated as the time elapsed between diagnosis of virological failure and date of death or date of last visit to the Center.
Statistical analysis was performed with the Statistical Package for the Social Sciences (SPSS) version 19.0 (IBM Corp. Released 2010). Simple and relative frequencies were estimated for categorical variables. Chi-square test was used to assess the association between categorical variables mortality of PLWHA. Means of continuous variables (age, viral load, CD4 count, number of doctors involved in care, and time between the HIV diagnosis and first virologic failure and failure in 2013), were compared with the Student’s t-test. Results were considered statistically significant at p < 0.05. Variables with a p-value ≤0.20 on univariate analysis were included in the multivariate model. The final model included all variables with p < 0.05. This study was approved by the Research Ethics Committee of the Health Department of Bahia State (SESAB), number 452782.
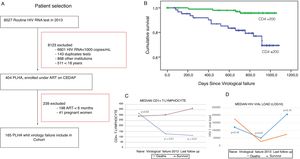
A total of 165 patients with HIV infection and virological failure in 2013 were identified and included in the cohort (Fig. 1A); 53.9% males, 67.3% heterosexuals, and 40.6% had less than four years of education. The mean age was 38.4 ± 9.5 years. Nineteen patients (11.5%) died after being diagnosed with virologic failure. Their sociodemographic characteristics were similar to survivors. Presence of clinical comorbidities (78.9%; diabetes, hypertension, dyslipidemias, neurological illnesses, and psychiatric disorders), user of illicit drug (52.6%), history of other virological failure prior to 2013 (89.5%), patients using firstline non-nucleoside reverse transcriptase inhibitor (NNRTIs) (73.7%), previous non-adherence to ART for longer than three months (89.5%), presence of cryptococcosis (10.5%), Kaposi’s sarcoma (10.5%), other neoplasms (10.5%), and tuberculosis (68.4%) were associated with death. Patients who died had a higher number of infectious diseases specialists involved in their care (6.3 ± 3.2 professionals) and only 10/19 (52.6%) patients had a genotyping test performed. The median CD4 count at the moment of virological failure was 127.8 cells/mm3 (±145.1), lower than that at diagnosis (317.1 cells/mm3; p < 0.01). In the last follow-up visit, only 15.7% had a viral load <50 copies/mL (Table 1). High median viral load and low CD4 count were associated with lower survival (p < 0.01) as shown in Fig. 1B, C and D. After multivariate analysis, all variables previously associated in the univariate analysis remained statistically associated with the occurrence of death. The mean survival after diagnosis of virological failure was 13.0 ± 5.0 months.
(A) Flow chart of patient selection and follow-up; (B) Kaplan-Meier survival curve analysis according to CD4 T > 200 or ≤200 cells/mm3, (C) Mean CD4 T, (D) Mean VL baseline, at virologic failure in 2013 and after two years of follow-up in PLWHA who died (N = 19) and in survivors (N = 146), Salvador, Bahia.
Demographic, clinical, and laboratory characteristics of people living with HIV/Aids diagnosed with virological failure in 2013, State HIV/Aids Reference Center, according to diagnosis of death, Salvador, Bahia,Brazil.
| N = 165 (%) | Death, n (%) | p-value | RR (CI)c | ||
|---|---|---|---|---|---|
| n (%) | Yes (n = 19) | No (n = 146) | |||
| Social and demographic characteristics | |||||
| Age (mean ± SD) | 38.4 (9.5) | 36.9 (9.8) b | 38.6 (9.5)b | 0.33 | |
| Male sex | 89 (53.9) | 12 (63.2) a | 77 (52.7)a | 0.39 | |
| Heterosexual | 111 (67.3) | 13 (68.4) a | 98 (67.1)a | 0.91 | |
| Self-reported blacks | 61 (39.6) | 11 (57.9) a | 50 (34.2)a | 0.08 | |
| Less than 8 years of schooling | 67 (43.3) | 10 (52.6) a | 57 (39.0)a | 0.38 | |
| Living in Salvador | 123 (74.6) | 15 (78.9) a | 108 (74.0)a | 0.64 | |
| Smoking | 56 (33.9) | 8 (42.1) a | 48 (32.9)a | 0.42 | |
| Alcohol consumption | 114 (69.1) | 14 (73.7) a | 100 (68.5)a | 0.64 | |
| Use of drugs | 43 (26.1) | 10 (52.6) a | 33 (22.6)a | <0.01 | 3.1 (1.3–7.2) |
| Laboratory and clinical characteristics | |||||
| First CD4 (mean ± SD) | 293.2 (±224.0) | 317.1 (±278.9) b | 290.0 (±216.8)b | 0.62 | |
| First CD4 ≤ 200 | 67% (±40.6) b | 12 (63.2) a | 55 (37.7)a | 0.03 | 2.5 (1.1–6.0) |
| CD4 in virological failure (mean ± SD) | 283.1 (±204.2) b | 127.8 (±145.1) b | 303.3 (±202.4)b | <0.01 | |
| Last CD4 (mean ± SD) | 333.5 (±272.1) b | 113.4 (±178.4) b | 362 (±269.5)b | <0.01 | |
| First VLd (mean ± SD) | 170,615.1 (±440,167.3) b | 120,789.5 (±160,409.6) b | 177,099.2 (±464,298.4) | 0,18 | |
| VLd in virological failire (mean ± SD) | 29,015.02 (±29,298.5) | 49192.4 (±35783.6) | 26389.2 (±27416.0)b | <0.01 | |
| Last VLd (mean ± SD) | 89,921.5 (± 401,559.6)b | 207,217.5 (±308,210.0) b | 74,657.9 (± 410,548.2)b | 0.10 | |
| Numbers of doctors (mean ± SD) | 4,9 (±3.2) a | 6,32 (±3.2) a | 4,91 (±2,3)b | 0.02 | |
| Comorbiditye | 96 (58.2)a | 15 (78.9) a | 81 (55.5)a | 0.05 | |
| Cytomegalovirus retinitis | 15 (9.1) a | 2 (10.5) a | 13 (9.2) a | 0.82 | |
| Cryptococcosis | 2 (1.2) a | 2 (10.5) a | 0 | <0.01 | 9.3 (6.1–15.0) |
| Hepatitis B | 8 (4.8) a | 0 | 8 (5.7) a | 0.30 | |
| Hepatitis C | 7 (4.2) a | 0 | 7 (5.0) a | 0.33 | |
| Herpes zoster | 48 (29.1) a | 5 (26.3) a | 43 (30.5) a | 0.78 | |
| HTLVf | 1 (0.6) a | 0 | 1 (0.7) a | 0.71 | |
| Other neoplasms | 4 (2.4) a | 2 (10.5) a | 2 (1.4) a | <0.01 | 9.6 (6.1–15.0) |
| Kaposi’s sarcoma | 4 (2.4) a | 2 (10.5) a | 2 (1.4) a | <0.01 | 9.6 (6.1–15.0) |
| Syphilis | 34 (20.5) a | 7 (36.8) a | 27 (19.1) a | 0.06 | |
| CNS toxoplasmosisg | 29 (18.2) a | 4 (21.0) a | 26 (18.4) a | 0.73 | |
| Tuberculosis | 55 (33.3) a | 13 (68.4) a | 42 (29.8) a | <0.01 | 4.3 (1.7–10.8) |
| Other virological failure prior to 2013 | 126 (76.4) a | 17 (89.5) a | 109 (74.7)a | 0.05 | 1.2 (1.1–1.2) |
| HIV Genotyping performed | 96 (58.2) a | 10 (52.6) a | 86 (58.9)a | 0.60 | |
| Use of NNRTIsh (1st line) | 78 (47.3) a | 14 (73.7) a | 64 (43.8)a | 0.01 | 3.1 (1.2–8.3) |
| History of ≥3 months without HAARTi | 109 (66.1%)a | 17 (89.5%) a | 92 (63.0)a | 0.02 | 4.4 (1.1–18.2) |
p < 0.05 and 95%CI for all comparisons.
The overall prevalence of virological failure in this study was 16.1% (165/1023), compared to 10% among adult PLWHA in Brazil as a whole, until October of 2015, according to the Brazilian Ministry of Health.2
During this two-year cohort study, individuals with virologic failure were at higher risk of death. The African cohort study reported by Petersen et al. showed a mortality rate among patients failing HAART of 5.9% in an average follow-up of 2.1 years, which is 2.78 times lower than the rate observed in the present study.5
Presence of comorbities, use of illicit drugs, diagnosis of tubercuolosis, cryptocoocosis, and Kaposi's Sarcomas are association with viral failure and mortality, as described in the literature.6 Mean viral load at the time of virologic failure was higher among patients who died than among survivors, a finding similar to that seen in North American and African cohorts.7,8 Mean CD4 T cell count at baseline was lower than 200 cells/mm3 in patients who died, suggesting late diagnosis of HIV infection. Several studies have shown that baseline CD4 T cell count lower than 200 cells/mm3 is associated with a delayed diagnosis and, consequently, death.7,8
This study also observed that patient non-fidelity to one attending physician and a history of abandoning HAART (prior to the failure in 2013, with a period ≥3 months without ART) were associated with mortality. These two factors influence treatment outcomes and are directly related to virological failure and development of drug resistance.9
In Brazil, there is an estimated prevalence of intermediary transmitted resistance of 8.1%, varying by regions of the country. However, in 2007, Pedroso et al. found a prevalence of 11.4% of transmitted resistance to NNRTIs in the Northeast, especially in Bahia.10 In the present study, the use of NNRTIs was significantly associated with mortality (p = 0.01), with a 3.1 times greater risk than that detected among patients who were taking protease inhibitors. These findings most likely reflect the greater circulation of HIV strains resistant to NNRTIs in Salvador.
The present study is relevant because it is one of the few real-life studies conducted in a reference center for the treatment of HIV/Aids in Brazil. The results reflect the growing concern about the incidence of virological failure and the associated high mortality, underscoring the need for greater attention to this at risk population. This study has some limitations. This observational study was limited to one center and the data used in this analysis were from a secondary source, resulting in incomplete data for some patients. However, we conducted additional data searches in the official database of Brazil (SICLOM, SISCEL, SIM) to improve the quality of information obtained from medical records. Our evaluation was limited to patients who had CD4 count and HIV viral load testing in 2013 available for review. In addition, HIV-1 viral load, considered to be the best predictor of HIV disease progression was the measure used in the present study. Our cohort was not very large; only 165 patients were diagnosed with virological failure for inclusion in the study. On the other hand, the study site was the largest reference center for care of PLWHA in the state of Bahia, and the prevalence of virological failure was high enough to draw relevant conclusions. Another limitation of the study was the inability to follow a parallel group with no virological failure due to inconsistency of the secondary data.
Our findings show that virological failure is associated with mortality. Moreover, factors such as coinfection with tuberculosis, illicit drug use, and low fidelity to one attending physician are risk markers of poor adherence, virologic failure, and higher mortality. Strategies to minimize these problems may result in decreased frequency of virological failure and lower risk of death of HIV infected patients.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.