This study performed at the National Research Institute of Tuberculosis and Lung Disease, Tehran, Iran, aimed to evaluate the effect of concomitant pulmonary hypertension on the outcome of pulmonary tuberculosis.
MethodsNew cases of pulmonary tuberculosis were recruited for the study. Pulmonary hypertension was defined as systolic pulmonary arterial pressure ≥35mm Hg estimated by transthoracic Doppler echocardiography. We assessed the relationship between pulmonary hypertension and mortality during the six-month treatment of tuberculosis.
ResultsOf 777 new cases of pulmonary tuberculosis, 74 (9.5%) had systolic pulmonary arterial pressure ≥35mm Hg. Ten of them (13.5%) died during treatment compared to 5% of cases with pulmonary arterial pressure less than 35mm Hg (p=0.007). Logistic regression analysis showed that pulmonary hypertension and drug abuse remained independently associated with mortality (OR=3.1; 95% CI: 1.44–6.75 and OR=4.4; 95% CI: 2.35–8.17, respectively).
ConclusionA significant association was found between mortality and presence of pulmonary hypertension and drug abuse among new cases of pulmonary tuberculosis.
Pulmonary tuberculosis (TB) continues to be a major health problem worldwide. In spite of effective chemotherapy, excess morbidity and mortality are attributed to TB. Because treatment success in pulmonary TB has been defined as mycobacteriological response, little attention has been paid to the related chronic disabilities in those who survived the disease.1 Despite successful treatment, a significant permanent damage of lung function has been reported in more than 50% of pulmonary TB patients. They may be obstructive or restrictive2 and lead to gas exchange abnormalities and development of pulmonary hypertension.3
Pulmonary hypertension (PH) is a serious disorder with poor prognosis. It is defined as a mean pulmonary arterial pressure (PAP) of more than 25mm Hg at rest.4 Recently, new therapeutic options have been developed for treating PH that improve quality of life and prognosis of the disease.5 Symptoms of PH consisting of dyspnea, palpitations, fatigue, and syncope are vague that postpone detection of it.4 As a result, an appropriate plan for screening PH is necessary among high risk groups of patients.
Few studies described PH in treated TB patients but most of them were conducted during pre-chemotherapy era.6 Studies about PH during active pulmonary TB are very scarce.7 Moreover, according to different definitions of the disease and various screening methods and population groups, the results are widely different.
This study was aimed to evaluate the effects of PH in the outcome of active pulmonary TB. Due to the growing range of therapeutic options, early diagnosis of pulmonary hypertension may change patient survival.
Materials and methodsThis retrospective cohort study was conducted on inpatient new cases of pulmonary tuberculosis that were diagnosed in the National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Tehran, Iran between 2005 and 2009. A diagnosis of TB was made by positive smear and culture results for Mycobacterium tuberculosis or histopathological findings. New cases of TB were defined as those who had received either no anti-TB drugs or less than one month of treatment in the past. TB treatment has been initiated at the time of diagnosis, as recommended by the World Health Organization (WHO) guidelines,8 consisting of isoniazid, rifampin, ethambutol and pyrazinamide for two months as initial phase and isoniazid and rifampin for the next four months as maintenance phase. All the patients were referred to peripheral health centers for continuing medication under the directly observed treatment (DOT) strategy in accordance with our National Tuberculosis Program (NTP). The outcome of treatment was defined according to WHO guidelines. Death due to any reason during the course of tuberculosis treatment was considered.8
For calculation of pulmonary artery pressure firstly tricuspid valve regurgitant jet was identified by color Doppler echocardiography (Vivid 7 dimension; Mann healthcare, GE). Then the trans-tricuspid pressure gradient was calculated using modified Bernoulli equation and right atrium pressure was added to obtained peak pulmonary artery pressure. For this study we considered pulmonary hypertension as peak systolic pulmonary arterial pressure equal or more than 35mm Hg estimated by resting transthoracic echocardiography.
Recorded data of all new cases of pulmonary tuberculosis from our hospital registry were preset for recent study. Demographic, characteristics and other variables were entered in SPSS (version 11.5) software.
The relationship between pulmonary hypertension and the outcome of TB treatment was assessed controlling for confounding factors (age, sex, smoking, drug abuse, symptoms and adverse effects of anti TB drugs) by regression analysis. The χ2 test was used for categorical variables, and whenever necessary, the Fisher exact test was utilized. Continuous variables with normal distribution were analyzed by t-Student test, and Mann–Whitney U test in case of abnormal distribution. A p-value<0.05 was considered statistically significant.
The scientific and ethics committee of the NRITLD approved the study protocol.
ResultsA total of 777 new cases of pulmonary tuberculosis were diagnosed in the study period. Systolic pulmonary arterial pressure more than 35mm Hg was detected in 74 (9.5%) by Doppler echocardiography. Right heart catheterization was not performed.
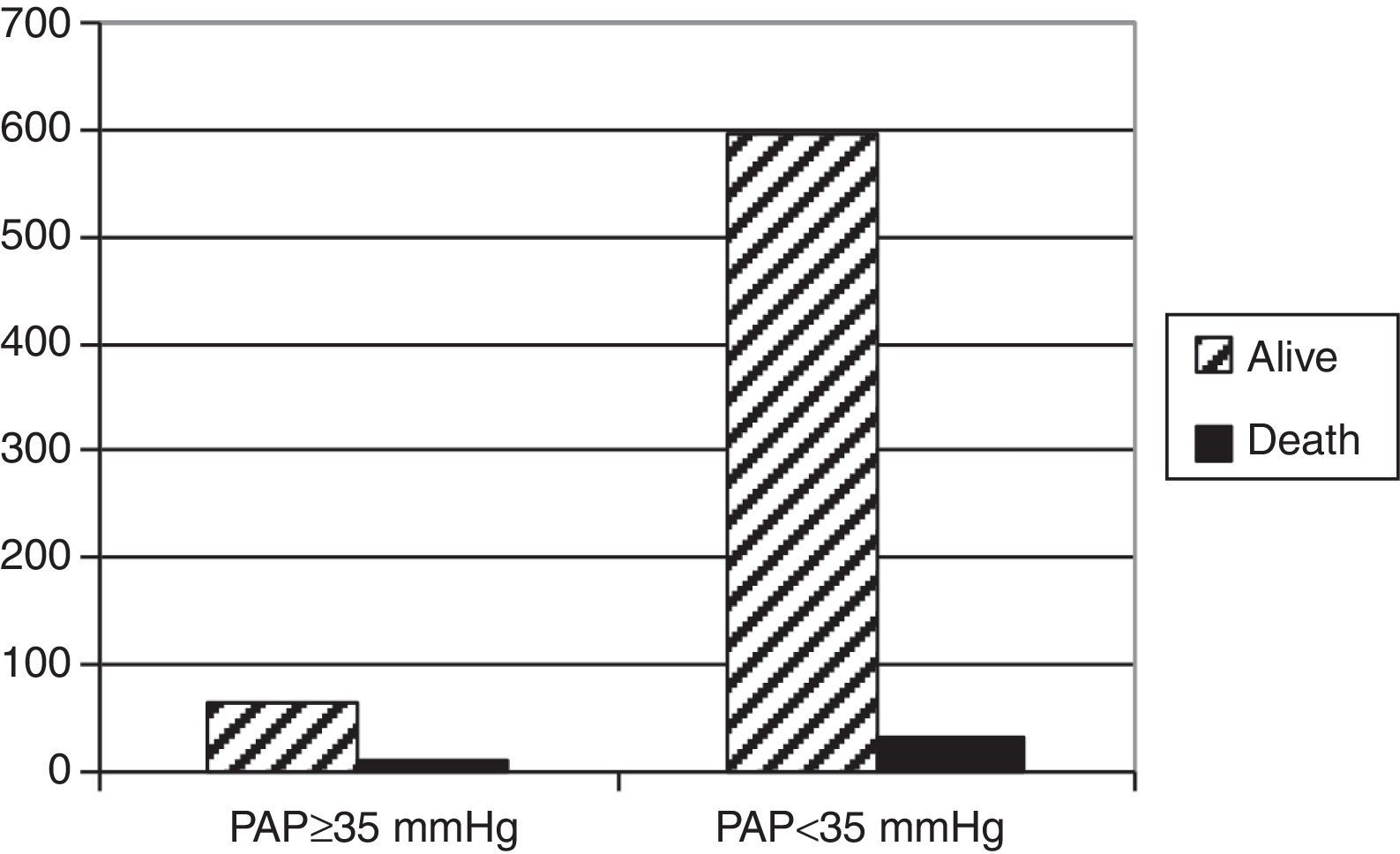
Characteristics of patients and clinical factors for both groups are showed in Table 1.
Characteristics of TB patients with and without pulmonary hypertension.
| Variables | PAP≥35mm Hgn (%) | PAP<35mm Hgn (%) | p-value |
|---|---|---|---|
| Gender | |||
| Male | 34 (45.9) | 323 (45.9) | NS |
| Female | 40 (54.1) | 380 (54.1) | |
| Age (mean±SD) | 68.50±15.56 | 52.99±21.78 | <0.001 |
| Smoker | 23 (31.1) | 183 (26) | NS |
| Opium addiction | 14 (18.9) | 131 (18.6) | NS |
| Hemoptysis | 8 (10.8) | 127 (18.1) | NS |
| Chest pain | 42 (56.8) | 311 (44.3) | 0.049 |
| Dyspnea | 66 (89.2) | 470 (66.9) | <0.001 |
| Total | 74 | 703 | |
PAP, pulmonary artery pressure; NS, not significant.
Males comprised 357 (45.9%). Mean (±SD) age of patients was 54.51±21.73; 84% were of Iranian nationality. HIV test was performed in 309 patients with 36 (4.7% of all cases) positive cases. All TB patients with PAP≥35mm were HIV negative.
There was no significant difference between patients with PAP above and below 35mm Hg concerning gender, smoking status, opium addiction, and history of hemoptysis.
Cases with pulmonary hypertension were older and present dyspnea and chest pain more often.
Adverse effects of anti-TB medications occurred in 26 (35%) patients with PAP≥35mm Hg and in 38% patients of the control (p=0.68). The major adverse effect was drug-induced hepatitis, which was not different between two groups (p=0.18).
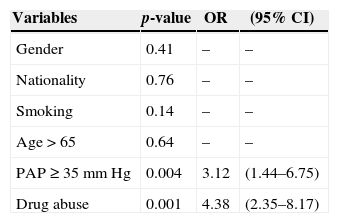
The outcome of TB treatment was known for 700 patients. Ten patients with PAP≥35mm Hg (13.5%) died during treatment in comparison to 5% of cases without PH (p=0.007) (Fig. 1).
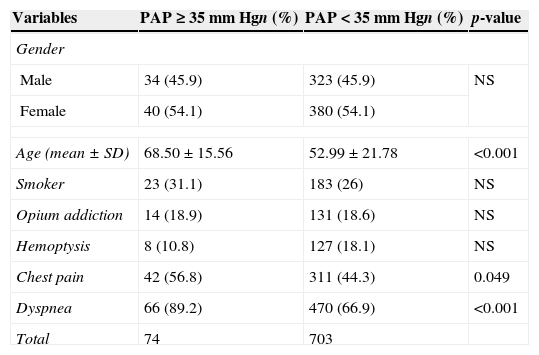
To determine the independent association of risk factors (gender, age>65, nationality, smoking status, and PAP≥35mm Hg) with mortality, a logistic regression was performed. Drug abuse and PAP≥35mm Hg were the factors that remained independently associated with mortality in the final model (Table 2).
Relationship between independent risk factors and death in TB patients.
| Variables | p-value | OR | (95% CI) |
|---|---|---|---|
| Gender | 0.41 | – | – |
| Nationality | 0.76 | – | – |
| Smoking | 0.14 | – | – |
| Age>65 | 0.64 | – | – |
| PAP≥35mm Hg | 0.004 | 3.12 | (1.44–6.75) |
| Drug abuse | 0.001 | 4.38 | (2.35–8.17) |
PAP, pulmonary artery pressure; OR, odds ratio; CI, confidence interval.
Overall, we found a 9.7% prevalence of pulmonary artery pressure equal or more than 35mm Hg among patients with active pulmonary tuberculosis. Patients with higher PAP were older and present with dyspnea more often. Mortality rate was higher among cases with PAP equal or more than 35mm Hg.
Since the 19th century myocardial damage has been found on autopsy studies in pulmonary tuberculosis patients.9 Accentuated 2nd heart sound over the pulmonary area of chronic TB patients is associated with an unfavorable outcome.10
Association of active tuberculosis and pulmonary hypertension has been assessed in few previous studies, in which PH or cor pulmonale was diagnosed either by electrocardiography or post-mortem.6 Cor pulmonale was the cause of death at necropsy in 23% of TB patients in one study with over 50% of these patients with a history of clinical signs related to cardiac failure before death.10
In a cross sectional study Ahmed and colleagues described 14 patients who presented with shortness of breath after successful treatment of pulmonary tuberculosis. PH was considered as pulmonary artery systolic pressure ≥40mm Hg estimated by Doppler echocardiography. Most of them had fibro cavitary or fibrotic changes in the chest X-ray. Their work is different from ours as none of their cases had active TB and the mean interval since TB diagnosis was 9.4 years.6
In a study with 52 new cases of pulmonary tuberculosis 44.2% had systolic pulmonary artery pressure above 25mm Hg by echocardiography. All the patients were young and majority of them had disseminated disease or involvement of intra-thoracic lymphatics.7
In our study, death was significantly higher among patients who had PAP≥35mm Hg. This finding is not in line with the results obtained by Tomono showing no association between PH and late sequela of TB. Comparison of these results to the present study may be problematic as we investigated active TB cases and short-term outcome as opposed to old TB cases and long-term outcomes of the Japanese study.11
Pathogenesis of pulmonary arterial hypertension among TB patients is not clear. In the past some suggested that repeated secondary infections in residual cavities and scar lesions of healed TB might have a role. Exudative secretions cause respiratory passage blockage, impairment in gas exchange and ultimately rising cardiac output.9 Nonetheless, this theory does not justify the reason for high pulmonary arterial pressure of active and new cases of TB. Active tuberculosis by unknown mechanisms may be directly responsible for rising PAP. Moreover, PH may be related to parenchymal destruction and hypoxia in the course of the disease especially in case of delayed diagnosis and initiation of anti-TB treatment. Concomitant lung diseases such as COPD as well as myocardial involvement could be the cause of PH.
The overall findings of our study corroborate the results of previous studies concerning the relevance of PH in TB patients, but our study was conducted in active TB cases and evaluated short-term outcomes. Although the current study has some strong points such as large number of cases, there are some important limitations. First, echocardiography had not been performed in all cases, which may have underestimated diagnosis of PH. Second, other causes of PH such as concomitant pulmonary disease have not been ruled out. Finally, diagnosis of PH had not been confirmed by right heart catheterization (RHC). Although RHC is the gold-standard procedure and necessary for PH confirmation,12 it is an invasive and expensive procedure, unsuitable as a screening tool. Transthoracic Doppler echocardiography has been shown to be a safe, sensitive and specific method for screening PH in patients with systemic diseases like systemic sclerosis and lupus erythematosus.13,14 Measurement of PAP by echocardiography in patients with severe tricuspid regurgitation may lead to underestimation. Also overestimation is common.15 So echocardiography may be not a suitable screening tool for asymptomatic patients with mild PH.12 Several cut-off points of PAP were used by investigators when screening for PH with Doppler echocardiography, such as 30mm Hg,13 40mm Hg,6 and 50mm Hg.14 The European Society of Cardiology and the European Respiratory Society suggest arbitrary criteria for diagnosing PH based on Doppler calculation and other echocardiographic findings.12
Although our study shows the relevance of PH in active pulmonary tuberculosis, there remains many unresolved issues: what are the risk factors of PH among TB patients? Is screening of PH indicated for the cases of pulmonary TB, minimally for those who are high risk for PH? What is the optimal tool for such screening? After detection of PH, is there any intervention that could improve outcome of TB patients? Prospective well-designed studies are necessary to respond these questions.
ConclusionPulmonary hypertension is common among active pulmonary tuberculosis patients and needs more attention. Higher pulmonary artery pressure in Doppler echocardiography is significantly associated to mortality among new cases of pulmonary tuberculosis.
Conflicts of interestThe authors declare no conflicts of interest.