This study describes the characteristics of 31 children with congenital toxoplasmosis children admitted to the University Hospital of Londrina, Southern Brazil, from 2000 to 2010. In total, 23 (85.2%) of the mothers received prenatal care but only four (13.0%) were treated for toxoplasmosis. Birth weight was <2500g in 37.9% of the infants. During the first month of life, physical examination was normal in 34.5%, and for those with clinical signs and symptoms, the main manifestations were hepatomegaly and/or splenomegaly (62.1%), jaundice (13.8%), and microcephaly (6.9%). During ophthalmic examination, 74.2% of the children exhibited injuries, 58.1% chorioretinitis, 32.3% strabismus, 19.4% microphthalmia, and 16.2% vitreitis. Anti-Toxoplasma gondii IgM antibodies were detected in 48.3% of the children. Imaging brain evaluation was normal in 44.8%; brain calcifications, hydrocephaly, or both conditions were observed in 27.6%, 10.3%, and 17.2%, respectively, of the patients. Patients with cerebrospinal fluid protein≥200mg/dL presented more brain calcifications (p=0.0325). Other sequelae were visual impairment (55.2% of the cases), developmental delay (31.0%), motor deficit (13.8%), convulsion (27.5%), and attention deficit (10.3%). All patients were treated with sulfadiazine, pyrimethamine, and folinic acid, and 55.2% of them exhibited adverse effects. The results demonstrate the significance of the early diagnosis and treatment of toxoplasmosis during pregnancy to reduce congenital toxoplasmosis and its consequences.
Toxoplasmosis is a worldwide infection caused by the protozoan Toxoplasma gondii (T. gondii), an obligatory intracellular parasite.1 In Central and South America, 50–80% of individuals are seropositive for IgG antibodies against T. gondii, indicating their previous exposure to this parasite.2 The prevalence of this infection acquired during pregnancy ranges from 10.3% to 75.2% in different countries.3–7 In Brazil, the seroprevalence of anti-T. gondii IgG antibodies ranges from 49.2% to 91.6%,8–10 and the incidence of congenital toxoplasmosis varies from 0.3 to 5.0 per 1000 births.11–13
The risk of fetal transmission depends on factors, such as the maternal immune response, the gestational age at infection, and the parasite virulence. The risk of congenital transmission varies from up to 2% at the periconceptional period, 10–25% in the first trimester of pregnancy, 30–45% in the second trimester, 60–65% in the third trimester, and up to 80% before childbirth.1 However, the severity of congenital disease is high when transmission occurs in the beginning of the pregnancy and decreases with gestational age.1,2,4,7,8
The diagnosis of toxoplasmosis acquired during pregnancy is based on laboratory tests because more than 90% of infected pregnant women are asymptomatic. When clinical manifestations are present, in general, they are nonspecific and include fever, headaches, myalgia, lymphadenopathy, and rash.14
The majority of children with congenital toxoplasmosis do not exhibit signs or symptoms at birth, presenting instead as subclinical infections; nevertheless, infected children are at risk of developing late sequelae, mainly ocular and neurological. For the symptomatic children, the severity of clinical manifestations is related to the trimester of pregnancy when transmission occurred, as follows: fetal death in the first trimester; retinochoroiditis, microcephaly, and mental retardation in the second trimester; and lymphadenopathy, hepatosplenomegaly, eye injuries, and brain calcifications in the third trimester.15 All of the children whose mothers presented acute toxoplasmosis during pregnancy, symptomatic or not, may have congenital toxoplasmosis. Children born with signals or symptoms of congenital disease are also at risk and should undergo serological investigation to detect specific anti-T. gondii antibodies.15
The purpose of this study was to describe the demographic, clinical, and laboratory characteristics of children with congenital toxoplasmosis that received treatment for congenital toxoplasmosis at one medical center in southern Brazil.
Materials and methodsPopulation and study designThe study included a retrospective cohort of 236 medical records of suspected congenital toxoplasmosis from the Outpatient Reference Centre for Pediatric Infectious Diseases, which is the reference service for congenital toxoplasmosis at the Outpatient Clinical Hospital, University of Londrina, Paraná State, Brazil. The study identified 31 cases of congenital toxoplasmosis that occurred from January 2000 to December 2010. This study was approved by the Ethical Committee Involving Humans from the University of Londrina, Londrina, Paraná, Brazil.
Diagnostic criteriaCases were defined as congenital toxoplasmosis when the infant exhibited one of the following features: anti-T. gondii IgM and/or IgA antibodies after 10 days of life, persistently elevated or increasing titers of IgG anti-T. gondii (after three-week intervals between the samples), seropositive for IgG after 12 months of life, retinochoroiditis and/or hydrocephaly/cerebral calcifications, and anti-T. gondii IgG seropositivity and response to specific treatment.16
During the period of the study, anti-T. gondii IgG antibodies were detected by indirect immunofluorescence (IFI) with T. gondii fixed on a glass slide.17 For the detection of anti-T. gondii IgM antibodies, the methods varied in the period evaluated, but included indirect enzyme immunoassay (ELISA), chemiluminescence, and IgM capture ELISA.
Statistical analysisData were recorded in a database, and the statistical analysis was performed using the Epi Info 3.4.3 and GraphPadPrism 5.00 software. Continuous variables were expressed in minimum and maximum values, mean, standard deviation, and median. Categorical variables were reported in absolute frequency (n) and percentage (%). Comparisons between groups of categorical variables were performed by Chi-square analysis or Fisher's exact test, when appropriate. An odds ratio (OR) and 95% confidence interval (CI) were also calculated. The results were considered significant when the p-value was less than 0.05 (5%).
ResultsDescription of the populationOf the 31 children evaluated, 20 (64.5%) were male and 11 (35.5%) were female. Their birth weights ranged from 1150 to 3800g (median 2585g), and 11 children (37.9%) had birth weights<2500g. Gestational age at delivery ranged from 26.2 to 41 weeks (median 36 weeks). Maternal age ranged from 14 to 42 years (median 26 years), and 23/31 (85.2%) pregnant women received prenatal care.
Clinical analysis of pregnant womenAmong the 31 pregnant women evaluated, 16 (51.6%) did not have a record of any clinical symptom, eight (25.8%) were asymptomatic, and seven (22.5%) showed symptoms, such as fever (6.5%), adenomegaly (6.5%), flu-like symptoms (6.5%), and myalgia (3.2%). The toxoplasmosis infection was not diagnosed in 20/31 (64.5%) during pregnancy. Four women (12.9%) had not received prenatal care, and 16 (51.6%) had a serology requested. Eleven (35.5%) pregnant women were suspected cases of recent T. gondii infection, indicated by positive tests for IgM anti-T. gondii. However, this suspicion was not confirmed by other tests or serial samples, and they were not treated for toxoplasmosis. Only four (12.9%) pregnant women infected with T. gondii received specific treatment (two with sulfadiazine, pyrimethamine, and folinic acid, and two with spiramycin). The other 27 (87.0%) pregnant women received no toxoplasmosis treatment.
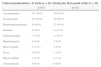
Clinical analysis of childrenTwenty children (64.5%) were examined at birth, and nine (29.0%) were evaluated in the first month of life. Two children (6.5%) were referred without any record of signs or symptoms. One child (3.2%) was evaluated for the first time after nine months of life with chorioretinitis, cataract, and microphthalmia. One child (3.2%) was first evaluated at five years of age and presented with sequelae of congenital infection, such as scars of chorioretinitis, hyperactivity, attention deficit, and precocious puberty. The frequency of clinical manifestations of congenital toxoplasmosis at birth and during the first month of life is shown in Table 1.
Clinical manifestations presented by children with congenital toxoplasmosis attended at the Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| Clinical manifestations | At birth (n=20) | During the first month of life (n=29) |
|---|---|---|
| n (%) | n (%) | |
| Asymptomatic | 10 (50.0) | 10 (34.5) |
| Symptomatic | 10 (50.0) | 19 (65.5) |
| Hepatosplenomegaly | 8 (40.0) | 13 (44.8) |
| Jaundice | 0 (0.0) | 4 (13.8) |
| Esplenomegaly | 1 (5.0) | 3 (10.3) |
| Hepatomegaly | 0 (0.0) | 2 (6.9) |
| Microcephaly | 1 (5.0.) | 2 (6.9) |
| Fever | 0 (0.0) | 1 (3.4) |
| Macrocephaly | 1 (5.0) | 1 (3.4) |
| Adenomegaly | 0 (0.0) | 0 (0.0) |
The clinical classification of the disease presented by these 31 children were as follows: 29 (93.5%) were classified in first month of life; four (13.8%) were subclinical without signs or symptoms during infancy; 24 (82.8%) exhibited neonatal disease with clinical manifestations, such as ocular lesion (chorioretinitis) and/or neurological impairment (hydrocephaly and/or calcification); and one (3.2%) was initially asymptomatic but presented fever and splenomegaly at four months of age without neurological or ophthalmic impairment. Among the children with subclinical infections, one (3.2%) had strabismus and convulsions at four years of age.
The ophthalmic manifestations observed in the children during the first month of life and after this period are described in Table 2.
Ophthalmologic manifestations observed during the first month and after the first month of life in children with congenital toxoplasmosis treated at the Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| Ophthalmologic manifestations | During the first month of life (n=29) | After the first month of life (n=31) |
|---|---|---|
| n (%) | n (%) | |
| No manifestationsa | 9 (31.0) | 8 (25.8) |
| Chorioretinitis | 16 (55.2) | 18 (58.1) |
| Strabismusb,c | 1 (3.5) | 10 (32.3) |
| Microphthalmia | 2 (6.9) | 6 (19.4) |
| Vitreitis | 5 (17.2) | 5 (16.2) |
| Uveitis | 3 (10.3) | 3 (9.7) |
| Cataractd | 1 (3.5) | 3 (9.7) |
| Nystagmuse | 0 (0.0) | 3 (9.7) |
One (3.5%) patient exhibited association of strabismus, cataract, and microphthalmia in the first month of life;
Of all the patients, one (3.2%) child was exposed but uninfected with HIV-1, and one (3.2%) was co-infected with HIV-1. One child (3.2%) was co-infected with HIV-1 and cytomegalovirus (CMV), and three children (9.7%) were co-infected with CMV. In one infant with persistent hepatitis, a CMV infection was diagnosed by polymerase chain reaction; out of three infants with anti-CMV IgM antibody, one presented with giant cell hepatitis.
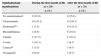
The frequency of sequelae was elevated among the children with congenital toxoplasmosis, as described in Table 3. Two (6.2%) children presented with endocrine dysfunctions, one with central precocious puberty and the other with secondary hypothyroidism.
Sequelaes detected in children with congenital toxoplasmosis attended at Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| Sequelae | Children (n=29) | |
|---|---|---|
| n | % | |
| Not detectablea | 9 | 31.1 |
| Detectable | 20 | 68.9 |
| Visual | 16 | 55.2 |
| Delay of psychomotor development | 9 | 31.0 |
| Convulsionb | 8 | 27.5 |
| Motor dysfunction | 4 | 13.8 |
| Hyperactivity and/or deficit of attention | 3 | 10.3 |
| Precocious puberty | 2 | 6.9 |
| Hypothyroidism | 1 | 3.4 |
| Ventricular peritoneal shunt | 1 | 3.4 |
| Hearing damagec | 3 | 50.0 |
Lumbar puncture for cerebrospinal fluid (CSF) collection was performed on 21 (67.7%) children. In the CSF, leukocytes ranged from 2 to 149cells/mm3 (median 19cells/mm3), erythrocytes ranged from 3 to 26,400cells/mm3 (median 56/mm3), and the protein concentration ranged from 34 to 1594mg/dL (median 104mg/dL). Although six (28.6%) CSF samples presented elevated erythrocyte count (>1000/mm3), high CSF protein observed could not be explained only by the presence of these cells. Six patients (28.6%) presented CSF protein >180mg/dL, but erythrocyte counts were>2500cells/mm3 in only one patient (erythrocyte=26,400cells/mm3 and protein=879mg/dL). Of the two patients (9.5%) with CSF protein >1g/dL, the erythrocyte count was lower than 35cells/mm3. In total, 19 patients (90.4%) who underwent lumbar puncture for CSF collection also performed imaging exams. Of these patients, 10 (52.6%) had brain calcifications, and two (10.5%) presented with brain calcifications associated with hydrocephaly. There was an association between the presence of ≥200mg/dL protein in CSF and brain calcifications (p=0.0352) (Table 4).
Results of imaging brain exams from children with congenital toxoplasmosis, according to the cerebrospinal fluid protein levels, attended at Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| CSF protein (mg/dL)a | Imaging brain exams | Odds ratio (95% CI) | p valueb | |
|---|---|---|---|---|
| With calcification n/total of cases (%) | Without calcification n/total of cases (%) | |||
| ≥200<200 | 5/5 (1000)5/14 (35.7) | 0/5 (0.0)9/14 (64.3) | 19.000.8729–413.6 | 0.0325 |
| ≥180<180 | 5/6 (83.3)5/13 (38.5) | 1/6 (16.7)8/13 (61.5) | 8.000.7107–90.05 | 0.1409 |
| ≥150<150 | 6/8 (75.0)4/11 (36.4) | 2/8 (25.0)7/11 (63.6) | 5.250.6979–39.50 | 0.1698 |
CSF, cerebrospinal fluid.
Brain computed tomography (CT) and ultrasonography (USG) results are presented in Table 5.
Results obtained in brain computed tomography and ultrasonography performed during the first month of life of children with congenital toxoplasmosis, attended at Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| Results | Brain CT (n=24) | Brain USG (n=13) | Odds ratio (95% CI) | p value |
|---|---|---|---|---|
| n (%) | n (%) | |||
| No changes | 11 (45.8) | 6 (46.1) | 1.182 (0.2950–4.735) | 0.8134* |
| Hydrocephalus | 0 (0.0) | 6 (46.1) | 0.02355 (0.00118–0.4688) | 0.0007† |
| Calcification | 8 (33.3) | 0 (0.0) | 13.91 (0.7337–263.7) | 0.0324† |
| Hydrocephalus and calcification | 5 (20.8) | 0 (0.0) | 7.615 (0.3877–149.6) | 0.1398† |
CT, computed tomography; USG, ultrasonography; CI, confidence interval.
Fifteen of the 23 (65.2%) patients presented ophthalmic injuries and concomitant brain lesions, while 2/17 (11.8%) patients did not present ophthalmic injuries but showed CNS lesions (p=0.1897, OR: 4.68, 95% CI: 0.73–29.85). There was no association between the presence of eye injuries and changes in brain imaging (hydrocephaly and calcifications). In 20 male patients, 15 (75%) showed eye injuries, while among 11 female patients, nine (81.8%) showed eye injuries (p=1.00, OR: 0.66, 95% CI: 0.10–4.18).
Overall, 15 (48.3%) children showed detectable serum levels of anti-T. gondii IgM antibodies. Two patients were seronegative for anti-T. gondii IgM in the first sample and seropositive in the second sample. The serum levels of anti-T. gondii IgG were obtained during the first week and the first, 3rd, 6th, 9th and 12th months of life. During the first week of life, the values ranged from 1:16 to 1:128,000 [mode=1:64 (20%) and 1:4000 (20%)]; in the 2nd sample, the levels ranged from 1:1024 to 1:128,000 [mode=1:8000 (33.3%)]. In the 3rd serial blood sample, the values ranged from 1:16 to 1:64,000 [mode=1:64,000 (27.3%)], and in the 4th serial blood sample, they ranged from 1:16 to 1:128,000 [mode=1:32,000 (20%)]. In the 5th serial blood sample, the values ranged from 1:256 to 1: 16,000 [mode=1:4000 (40%)], and in the 6th serial sample, they ranged from 1:16 to 1:32,000 [mode=1:16 (33.3%)]. During serological evolution of the patients, the rebound effect was detected in nine patients after discontinuing treatment and was detected by an increased level of serum anti-T. gondii IgG between 15 and 18 months of life, ranging from 1:16 to 1:128,000 [mode=1:1024 (28.6%)].
Treatment dataChildren's age for initiation of toxoplasmosis treatment ranged from one day to nine months (median age, one month). Among the 29 infants who received specific therapy, 28 (90.3%) received sulfadiazine, pyrimethamine, and folinic acid, and one (3.2%) received spiramycin. Ten infants (34.5%) were treated with corticosteroids (prednisone) associated with specific therapy when their CSF protein was ≥1g/dL and/or when they presented chorioretinitis with macular injury. Two children (6.5%) were not treated. One five-year-old child was referred to the reference service but the mother of the other child refused treatment, and the infant had no clinical follow-up. The infant who was treated with spiramycin for three months at another health service was switched to put on sulfadiazine, pyrimethamine, and folinic acid. Among the 29 (93.5%) treated infants, the treatment was temporarily modified in nine (31.0%): two children (6.9%) were treated with clindamycin, one (3.5%) with pyrimethamine and folinic acid, and six (20.7%) were treated with spiramycin.
Regarding the use of associated therapies, three children were treated with ganciclovir, two with zidovudine (AZT), and one with ganciclovir associated with AZT.
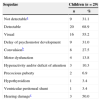
During the treatment for toxoplasmosis, 16 of the 29 patients (55.2%) presented adverse effects (Table 6). Six patients (37.5%) received a combination of therapies. Four patients received AZT, and three patients received ganciclovir. One infant treated with spiramycin was presented with frequent vomiting that improved with the reintroduction of sulfadiazine, pyrimethamine, and folinic acid. Hematological changes, including mild neutropenia and/or mild anemia, were reversed with an increased daily dose of folinic acid. When reverted to sulfadiazine, pyrimethamine, and folinic acid therapy, patients who temporarily received modified treatment because of adverse effects were treated with a higher daily dose of folinic acid.
Major adverse effects observed among children with congenital toxoplasmosis during the treatment with sulfadiazine, pyrimethamine, and folinic acid, attended at Outpatient Clinic Hospital of the State University of Londrina, Londrina, Paraná, from January 2000 to December 2010.
| Adverse effects | Children (n=29) | |
|---|---|---|
| n | % | |
| Mild neutropeniaa (1001–1499cells/mm3) | 4 | 13.8 |
| Moderate neutropenia b (501–1000cells/mm3) | 7 | 24.1 |
| Severe neutropeniac (≤500cells/mm3) | 2 | 6.9 |
| Mild megaloblastic anemia (Hemoglobin: 10.1–11.9g/dL) | 1 | 3.5 |
| Moderate megaloblastic anemia (Hemoglobin: 8.1–10.0g/dL) | 0 | 0.0 |
| Severe megaloblastic anemiac (Hemoglobin: ≤8.0g/dL) | 1 | 3.5 |
| Mild thrombocytopeniac (platelets 101,000–140,000/mm3) | 1 | 3.5 |
| Moderate thrombocytopeniad (platelets 51,000–100,000/mm3) | 1 | 3.5 |
| Severe thrombocytopenia (platelets≤50,000/mm3) | 0 | 0.0 |
| Mild hepatitis (AST and/or ALT≤two times the reference value) | 3 | 10.3 |
| Moderate hepatitis (AST and/or ALT>two times the reference value, and normal protrombine time test) | 1 | 3.5 |
| Severe hepatitis (protrombine time test<50.0% or INR>1.3) | 0 | 0.0 |
AST, aspartate aminotransferase; ALT, alanine aminotransferase; INR, international normalized ratio.
As clinical signs and symptoms in pregnancy are limiting factors for diagnosis, systematic serological screening tests during pregnancy are important yet controversial tools, particularly in regions where immunoreactivity before pregnancy is low and the risk for seroconversion during the pregnancy is high. However, early diagnosis of T. gondii infection and appropriate anti-parasitic treatment are measures that can reduce transmission and the severity of fetal consequences, which justifies the screening of all pregnant women with serological tests that detect anti-T. gondii IgG and IgM antibodies.15,18 A study from southern Brazil showed that 47.8% of pregnant women were seropositive for T. gondii, indicating previous exposure to the parasite, and 27.2% were not correctly diagnosed for T. gondii during pregnancy due to some factors, such as lack of prenatal care or because the serological tests were not performed.13 Despite the good prenatal care for pregnant women evaluated in the present study, serological investigation for toxoplasmosis was not performed in the majority of pregnant women.
The high frequency of prematurity and the low birth weight of infants observed in the present study are consistent with previous Brazilian studies that showed birth weight of infected children varying from 1290 to 3790g.13,19–24
Congenital toxoplasmosis may present different clinical forms, including subclinical infection, disease during the neonatal period, severe disease, mild disease in the first month of life, sequelae or reactivation of previously undiagnosed infection.15
In newborns and symptomatic infants, clinical presentation is divided into neurological and generalized forms. One neurological form, Sabin's tetrad, results from fetal infection at the beginning of the pregnancy and produces diffuse cerebral calcifications, chorioretinitis, convulsions, hydrocephaly or microcephaly. The generalized form results from infection during late pregnancy and is characterized by chorioretinitis, changes in CSF, hepatosplenomegaly, jaundice, lymphadenomegaly, thrombocytopenia, and anemia.15,18
Brazilian studies carried out between 1990 and 2010 showed that early clinical manifestations were present in 56–100% of the children evaluated. Chorioretinitis was present in 67–80%, and brain calcifications were observed in 11–100% of the cases, many of them without prenatal treatment.13,19–25 Other studies reported the presence of hydrocephaly in 6.3–21% of children and microcephaly in 5.3% of the evaluated children.24,26
Ocular injuries are not totally dependent on the gestational age of maternal infection; they may result in severe cases of chorioretinitis, even if the infection is acquired in the second half of the pregnancy. Furthermore, the risk of chorioretinitis – the most frequent sequela – persists for many years.27 Of the ocular manifestations among Brazilian children with congenital toxoplasmosis, 29–100% presented chorioretinitis during the evolution of the disease, with 12–84% presenting bilateral injuries. Frequent symptoms include microphthalmia (9–25% of cases), strabismus (12–60%), nystagmus (3–47%), cataract (1–14%), vitreitis (3–50%), and visual damage (50–100%).13,19–28 Therefore, the results of the present study are in line with other Brazilian studies; however, it showed higher frequency of symptomatic children at birth and with ocular manifestations than other studies carried out with children from Europe and North America.27 One possible explanation for this result may be the presence of more virulent strains of T. gondii in Brazil.29
The risk factors associated with the development of chorioretinitis include female gender, brain calcifications, and delay of maternal treatment after seroconversion.18,30 In the present study, ocular injuries was neither associated with child gender nor with the presence of brain calcifications.
In agreement with other studies conducted in the pre-treatment period among Brazilian and American children,18 the present study showed that 55.2% of infants exhibited neurological injuries in imaging exams, with calcification in 44.8% of cases.
Asymptomatic infants at birth may progress with no infection sequelae, but may also develop visual damage, delayed neuropsicomotor development, hydrocephaly, convulsions or deafness months or years after birth.15,18,20 Sequelae were identified in 68.9% of patients evaluated in this study, and the most frequent sequelae were visual impairment and neurological damage.
One of the benefits of treatment is the decrease in ocular and neurological sequelae in T. gondii-infected children.18,31 Early treatment prevents ocular damage in children, as shown in two longitudinal studies where a new lesion during the follow-up was detected in 72% of untreated children compared to 31% of treated children.32,33
Studies suggest that CT is more sensitive than USG for detecting brain calcifications.34 However, a study comparing brain CT and USG in 33 children with congenital toxoplasmosis found 94% agreement between these imaging exams.35
In the present study, CT was more sensitive for detecting brain calcifications, and USG was more sensitive for detecting hydrocephaly. However, specific treatment for toxoplasmosis provided during the period between USG and CT evaluations may have been responsible for missing hydrocephaly in CT that was shown with USG. The majority of USG evaluations were performed during the first month of life. The higher number of cases with brain calcifications observed by CT compared to those observed by USG may be explained by the natural evolution of the CNS lesions.
Congenital toxoplasmosis can be transmitted by pregnant women infected with HIV-1 who are those chronically infected with T. gondii;29,36 there are also reported cases of CMV and T. gondii co-infection.15,37 In the present study, the four infants co-infected with CMV showed clinical improvement when ganciclovir was added to the specific therapy for toxoplasmosis. This result demonstrates the importance of excluding other associated infections in patients with congenital toxoplasmosis.
Among the adverse effects of toxoplasmosis treatment, the most harmful is neutropenia caused by the myelotoxicity of sulfadiazine and pyrimethamine.15 In the present study, severe and moderate neutropenia were observed in a few cases, and the majority of them had been treated with other myelotoxic drugs associated with toxoplasmosis treatment, although all adverse effects were reversible with increased folinic acid doses and temporary interruption of the treatment. Reversible neutropenia was also observed in a cohort of patients, evaluated from 1981 to 2004 in North America, with daily doses of pyrimethamine for two or six months.31
In the present study, anti-T. gondii IgM seroprevalence was lower than observed in previous studies that confirmed T. gondii infection by the detection of IgM antibodies in 50–75% of newborns.15,22,38 The presence of anti-T. gondii IgG antibodies in a newborn serum sample is not evidence of infection because maternal IgG antibodies are passively transmitted. The half-life of this immunoglobulin is 23 days and maternal antibodies may persist in the newborn circulation for one year, and about three months are necessary for a 10-fold reduction in titer. Therefore, anti-T. gondii IgG antibodies must be assayed in serial samples from the child to confirm a congenital infection.15,26 However, in the present study due to wide variation (ranging from 1:16 to 1:128,000) serum anti-T. gondii IgG was of little help to diagnose congenital disease. Other serological methods are necessary to identify cases with false negative results for anti-T. gondii IgM.
Although the quality of prenatal care for suspected cases of toxoplasmosis in Londrina and northern Paraná in 2006 was not ascertained, a robust multi-professional team, with the support of governmental institutions, started discussions about this important public health problem, which resulted in the implementation of the Surveillance Program of Congenital Toxoplasmosis, first in the Basic Health Units of Londrina, north of Paraná, and afterwards in other locations in Paraná state.39,40 Its objective is to inform, standardize, and guide the management of medical professionals in caring for pregnant women with suspected or confirmed toxoplasmosis and children with congenital toxoplasmosis. To date, there has been excellent adherence to the proposed program in the primary health care units, decreasing the number of pregnant women and children unnecessarily referred to reference centers for diagnosis and treatment of toxoplasmosis by 63.9% and 42.6%, respectively, at the University of Londrina Hospital. Furthermore, the incorrect use of sulfadiazine was decreased by 67.4% after the program was implemented.39,40
Altogether, the results of the present study demonstrated that from 2000 to 2010, the majority of pregnant women whose children presented congenital toxoplasmosis and had received care at the reference center for Pediatric Infectious Diseases of the Outpatient Clinical Hospital of State University of Londrina, were given no treatment for toxoplasmosis during the pregnancy because no diagnostic tests for toxoplasmosis had been requested. The majority of children were symptomatic in the first month of life, and chorioretinitis was the most frequent ocular damage. A high frequency of sequelae was also observed in this cohort of patients. These data reinforce the importance of diagnosis and treatment of toxoplasmosis acquired during pregnancy to reduce the occurrence of congenital toxoplasmosis and its complications in the child. Continuous assessment, consolidation, and expansion of the Surveillance Program of Congenital Toxoplasmosis39,40 can contribute to the improvement of health care for pregnant women with suspected toxoplasmosis and for the reduction of congenital toxoplasmosis in the Brazilian population.
Conflicts of interestThe authors declare no conflicts of interest.