Human papillomaviruses (HPV) is from the genus Alphapapillomavirus, family Papillomaviridae. Of the over 120 HPV types that have been identified, about a dozen types are called “high-risk” types (HR-HPV) because they can lead to cervical cancers. Therefore, early diagnosis of HPV infection and characterize the HPV types becomes a key issue for cervical cancer prevention.1,2 Our study characterized the HR-HPV infections and genotypes in Jining, a medium sized city located in the east part of China, with a RT-PCR and hybridization method.
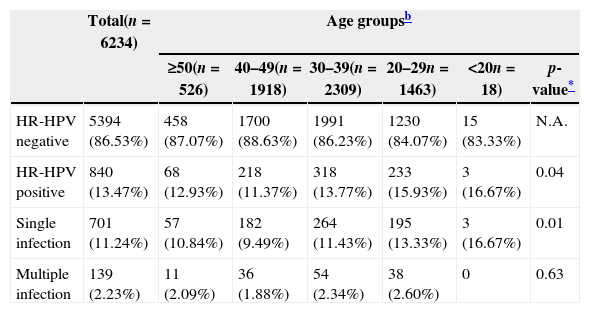
The study population consisted of 6234 women who attended the Affiliated Hospital of Jining Medical College for cervical smears between January 2010 and May 2012. The average age of the participants was 37 years old (range: 14–79 years). Overall 13.47% (840/6234) of the tested women were found to be positive for HR-HPV infection. Out of the 840 women infected with HR-HPV, 701 women (11.24%) were infected with a single HR-HPV genotype and the remaining 139 women (2.23%) were infected with multiple genotypes. Analysis of the relationship between age and HR-HPV genotype showed that younger woman had a higher rate of infection. In the study populations of woman aged over 50 and aged between 40 and 49 years old, the HR-HPV infection rate were 12.93% and 11.37%, respectively. The rates rose to 15.93% and 16.67% for woman aged 26–29 years old and for teenage women, respectively (p<0.05). When single infection and multiple infection were analyzed separately, although there was no multiple infection cases were found among teenage women, which might be due to the small study sample from this group, both single infection and multiple infection showed the same trend.
When the HR-HPV genotypes were considered separately, HR-HPV 16 was the most prevalent type (361/6234=5.79%), and HR-HPV 58 (2.58%) and 52 (2.50%) ranked the second and the third, respectively, followed by 33, 31, 18 and 39. The prevalence of each HR-HPV type in each age group was determined too (Table 1). In all of the five study groups, HR-HPV 16 ranked first. While HR-HPV 52 ranked second in populations aged over 50 and aged between 30 and 39 years old, HR-HPV 58 ranked second in the remaining age strata, and HR-HPV 52 ranked third.
The prevalence of HR-HPV.a
| Total(n=6234) | Age groupsb | ||||||
|---|---|---|---|---|---|---|---|
| ≥50(n=526) | 40–49(n=1918) | 30–39(n=2309) | 20–29n=1463) | <20n=18) | p-value* | ||
| HR-HPV negative | 5394 (86.53%) | 458 (87.07%) | 1700 (88.63%) | 1991 (86.23%) | 1230 (84.07%) | 15 (83.33%) | N.A. |
| HR-HPV positive | 840 (13.47%) | 68 (12.93%) | 218 (11.37%) | 318 (13.77%) | 233 (15.93%) | 3 (16.67%) | 0.04 |
| Single infection | 701 (11.24%) | 57 (10.84%) | 182 (9.49%) | 264 (11.43%) | 195 (13.33%) | 3 (16.67%) | 0.01 |
| Multiple infection | 139 (2.23%) | 11 (2.09%) | 36 (1.88%) | 54 (2.34%) | 38 (2.60%) | 0 | 0.63 |
Among the 132 multiple infection cases, 122 women were infected by dual infections (122/6234=1.96%) and 15 women had triple infections. While no cases were infected by four HR-HPV genotypes, 2 women, in the age-groups of 30–39 and 20–29, respectively, were infected by five HR-HPV genotypes. The rates of infection with multiple HR-HPV were higher in the younger age groups than in the older groups. In the 20–29 year age group, 2.6% (38/6234) were found to be infected with more one type of HR-HPV. The rated decreased to 1.88% (36/1918) and 2.09% (11/526) in the 40–49 age group and over 50 age group, respectively. In the multiple HR-HPV infected population, HR-HPV 16, 52 and 58 ranked as the first three most common genotypes with minor variation in different age groups.
Previous studies showed that infection with high-risk HPV is the predominant cause of cervical cancers.1,2 The launching of HPV vaccines greatly benefits the women by reducing the HPV infection rate. The two available vaccines, which are the quadrivalent vaccine and the bivalent vaccine, differ in that the quadrivalent vaccine contains VLPs from recombinant HPV 6, 11, 16 and 18, and aims at preventing cervical cancer intraepithelial neoplasia (CIN2, 3), cervical cancer and genital warts, while the latter only contains recombinant VLPs against HPV 16 and 18 and, therefore cannot confer protection against genital warts.3,4 Since the geographical distribution of HPV types coevolved with human population migration and behavioral changes, early diagnosis and characterization the HPV types is an important step toward the development of optimal protective strategies. The result of this study will provide important information for the application of future prophylactic vaccine program.5
Conflict of interestThe authors declare to have no conflict of interest.