The increase in life expectancy for patients living with human immunodeficiency virus (HIV) infection has resulted in health complications related to a chronic disease.
ObjectivesTo evaluate the prevalence of bone mineral density (BMD) alterations and vitamin D concentrations in HIV-infected children and adolescents and to verify the variations in those parameters during a 12-month interval.
MethodsA prospective cohort study with a dual period of evaluation was conducted in 57 patients perinatally HIV-infected and one patient with sexual abuse in early infancy. Demographic, anthropometric, pubertal stage, viral load, T CD4+ cell count and antiretroviral therapy were evaluated. Biochemical tests and total body (TB) and lumbar spine (L1–L4) bone density evaluations by dual X-ray absorptiometry (DXA) were performed. Calcium or vitamin D supplements were prescribed if reduction in BMD or deficiency for vitamin D was detected.
Results58 patients (ages 5.4–18.3 years; 60.3% girls) were included (T0); 55 patients were reevaluated after 12 (±3) months (T1). Low bone mass for chronological age was found in 6/58 (10.4%) and 6/55(10.9%) patients at T0 and at T1, respectively. There was no statistical relationship between z-scores for BMD (BMD z-score) and the variables sex, fracture history, family history of osteoporosis, physical activity and pubertal stage. There was a relation between BMD z-score alterations for TB and HIV viral load at T1 (p=0.016). There was no association between duration or classes of antiretroviral therapy and bone density. The mean value of vitamin D in T0 was 23.43ng/mL±2.015 and in T1 22.1ng/mL±0.707 and considered insufficient levels for this population.
ConclusionPatients infected with HIV are at risk for BMD alterations and lower vitamin D serum concentrations; both of these variables should be evaluated at routine examinations in order to improve both prevention and therapeutic planning.
The use of combined highly-active antiretroviral therapy (HAART) has significantly reduced opportunistic infections and the mortality rate in patients infected with human immunodeficiency virus (HIV), allowing for the onset of related comorbidities, including bone mineral density (BMD) alterations.1,2 Several mechanisms are involved in the genesis of bone alterations during HIV infection, such as the action of the virus itself, which results in inflammatory effects mediated by cytokines in osteoblast and osteoclast activity, and exposure to antiretroviral agents (in particular the nucleoside reverse transcriptase inhibitor tenofovir and protease inhibitors).3
The acceleration of bone reabsorption culminating in osteopenia and osteoporosis has been reported in patients infected with HIV who are not receiving antiretroviral treatment, as well as in patients undergoing HAART.4 Nutritional alterations, changes in vitamin D metabolism, hormonal disorders, decrease in physical activity, and presence of opportunistic diseases associated with HIV can also contribute to the process leading to abnormal BMD.5
The purpose of this study was to evaluate, in a cohort of children and adolescents mainly perinatally infected with HIV, the prevalence and change over a 12 (±3) month period of alterations in BMD and in vitamin D concentrations.
MethodThis prospective study was approved by the Ethics in Research Committee of the UNIFESP/EPM. Eligible patients (age >8 years) or their legal guardians signed the informed consent form. A total of 58 children and adolescents (between 5 and 20 years of age and of both sexes) infected with HIV were included in the study and followed at the CEADIPe UNIFESP/EPM (Division of Pediatric Infectious Diseases). Fifty-seven patients were perinatally infected and one patient was sexually abused in early infancy. The evaluations were performed at two different times (T0 and T1), with a 12 (±3) month interval between the evaluations. Exclusion criteria included patients who were taking corticosteroids, calcium, vitamin D or a bisphosphonate, or those who had interrupted these therapies less than three months prior to the study.
The following data was collected for each study participant: demographics, anthropometrics, pubertal stage, class and duration of antiretroviral treatment, and duration of HIV infection. At both timepoints (inclusion and 12 months thereafter), HIV viral load, CD4+ T-cell counts and biochemical tests were performed, and the serum concentration of vitamin D was determined. Total body (TB) and lumbar spine (L1–L4) BMD were assessed using dual-energy X-ray absorptiometry (DXA) (LUNAR DPX-MD plus; Lunar Radiation Corporation, Madison, WI, USA) with software for performing pediatric exams (version 8.5). The main author, previously trained by a nutrition team, elaborated a food intake record for each patient over a period of four consultations during the study. The frequency of intake of foods containing calcium and vitamin D was evaluated using the software NUTWIN/UNIFESP (São Paulo, Brazil).6
According to the International Society for Clinical Densitometry, the diagnosis of osteoporosis in children and adolescents, in the absence of vertebral compression (crush) fractures, is indicated by the presence of both a clinically significant fracture history and BMD z-score≤−2.0. Osteopenia is defined as z-score BMD in children and adolescents between −1 and −2.
In the event that a reduction in BMD was detected at the first evaluation, calcium (500–1000mg/d) and vitamin D (400–800IU/d) supplements were prescribed, with doses depending on patients’ daily consumption (for calcium) and patient age and severity of deficiency (for vitamin D). The occurrence of hypercalciuria was monitored by using a urine sample after a month on supplements. Height and weight measurements were taken on the same day as the laboratory tests (T0 and T1) and were used to calculate and classify BMD z-scores.
Biochemical evaluation included serum total protein and fractions, calcium and phosphate totals, creatinine, urea, alkaline phosphatase, parathyroid hormone (PTH), and 25-hydroxy (OH) vitamin D (25-OHD). The serum level for 25-OHD was determined in duplicate using a commercial radioimmunoassay kit (Nichols Institute Diagnostics, CA, USA), which detects 25-OH-D2 and 25-OH-D3. Variations of up to 5% between the two measurements were acceptable. Results were interpreted according to the cutoffs proposed by Holick et al.,7 with <20ng/ml being considered deficiency, 21–29ng/ml insufficiency, and >30ng/ml adequate level.
All DXA measurements were performed by the same trained technician under the supervision of an experienced physician of the bone density discipline of the rheumatology division of UNIFESP. The variation coefficient, measured daily according to the manufacturer's recommendation, was 2% for both L1–L4 and TB BMD. For patients with a short stature, BMD evaluation was performed taking age stature into consideration. BMD z-scores>−1 SD were considered normal, and BMD z-score<−2 SD were considered low BMD according to chronological age.8
The software Statistical Package for the Social Sciences (SPSS) version 21 (Chicago, USA) was used for statistical analysis. Categorical variables are presented as absolute frequencies (n) and percentages (%). For quantitative variables are summarized as medians and SDs. The Student's t-test was applied for comparison of means of quantitative variables (measured on comparable scales) of independent and paired samples (difference between T1 and T0) that followed a normal distribution. Otherwise non-parametric Wilcoxon test was used as an alternative.
The alterations in proportions between the periods T1 and T0 were assessed using the McNemar test. In order to determine the extent of the linear relation between two quantitative variables, the correlation tests by Pearson or Spearman were used. For the independent variables associated with BMD z-scores for TB and L1−L4, a binominal logistic regression was used. The significance level used on all tests was 5%.
ResultsThe initial study sample included 61 patients, three of whom were excluded due to technical difficulties for determining BMD. Thus, 58 patients between 5.8 and 18.3 years of age (median, 14.2 years) formed the study sample during the period of June 2011 to September 2011. Thirty-five patients (60.3%) were female. Of the 58 patients evaluated at the first timepoint (T0), 55 were re-evaluated after 12 months (at T1); three patients were excluded.
Patients with moderate clinical symptoms (classification B) and in immunological category 2, according to the Centers for Disease Control and Prevention (CDC) classification system, represented 63.8% and 46.6% of the study sample, respectively. Forty-five (77.6%) of the participants were already pubertal at T0 and 47 (85.5%) at T1. Table 1 shows the means of HIV transmission, sex, pubertal stage, and clinical and immunological classifications of the patients. Seven (12.1%) patients had a history of low impact traumatic fractures, nine (15.5%) had a family history of osteoporosis, two (3.4%) presented with bone pain, and 22 (37.9%) participated in sports one to three times a week. There was no significant association at T0 and T1 between BMD z-scores for TB and L1−L4 and the variables sex, trauma history, family history of osteoporosis, bone pain, physical activity, and pubertal stage.
Patients characteristics at time zero (T0) and time one (T1).
| T0 (N=58) | T1 (N=55) | ||||
|---|---|---|---|---|---|
| Variables | Category | n | % | n | % |
| Type of transmission | Vertical | 56 | 96.6 | ||
| Sexual | 1 | 1.7 | |||
| Unknown | 1 | 1.7 | |||
| Sex | Female | 35 | 60.3 | 34 | 61.8 |
| Male | 23 | 39.7 | 21 | 38.2 | |
| Pubertal stage | Pubertal | 45 | 77.6 | 47 | 85.5 |
| Not pubertal | 13 | 22.4 | 8 | 14.5 | |
| CDC clinical classification | N | 3 | 5.2 | 3 | 5.5 |
| A | 6 | 10.3 | 6 | 10.9 | |
| B | 37 | 63.8 | 35 | 63.6 | |
| C | 12 | 20.7 | 11 | 20 | |
| CDC immunological classification | 1 | 10 | 17.2 | 10 | 18.2 |
| 2 | 27 | 46.6 | 24 | 43.6 | |
| 3 | 21 | 36.2 | 21 | 38.2 | |
CDC, Centers for Disease Control and Prevention.
Regarding viral replication and immunological status, there were no statistical differences between T0 and T1 (p=0.489 and p=0.384, respectively). Low bone mass for chronological age was found in 6/58 (10.4%) and 6/55 (10.9%) patients at T0 and T1, respectively (Table 2).
Absolute number and percentage of patients with total body (TB) and lumbar spine (L1–L4) BMD z-score≥−2, z-score<−2 at time zero (T0) and after 12 months (T1).
| T0 (N=58) | T1 (N=55) | |||
|---|---|---|---|---|
| Variables | n | % | n | % |
| BMD z-score normal (TB+L1–L4) | 52 | 89.6 | 49 | 89.1 |
| BMD z-score altered (TB+L1–L4) | 6 | 10.4 | 6 | 10.9 |
| z-Score<−2 (TB) | 2 | 3.5 | 1 | 1.8 |
| z-Score<−2 (L1–L4) | 4 | 6.9 | 5 | 9.1 |
BMD, bone mineral density; TB, total body; L1–L4, lumbar spine L1–L4.
At T0, CDC immunological classification (CDC 1994) was significantly associated with BMD TB z-scores between −1 and −2 SD (p=0.041); CD4+ T-cells ≤500cells/mm3 was associated with TB and L1–L4 BMD z-scores alteration (p=0.02 and p=0.016, respectively). Also, at T1, there was an association between BMD L1–L4 z-scores alteration and detectable viral load (p=0.042).
There was no association at T1 between BMD z-score alteration and pubertal stage (p=0.20), duration of HIV infection (p=0.81), duration of antiretroviral therapy, different classes of antiretroviral drugs (p=0.84), and race (p=0.41).
Patients had received antiretroviral treatment with nucleoside reverse transcriptase inhibitors for an average of 113 months, with non-nucleoside reverse transcriptase inhibitors for an average of 55.2 months, and with protease inhibitors for an average of 68.2 months. The median time of use of tenofovir, efavirenz, and stavudine, as evaluated at T0, were 42 months, 45.2 months, and 57 months, respectively, with no statistical differences compared to T1.
Table 3 shows the number of patients who presented with alterations in one or both assessed areas (TB and L1–L4) according to clinical parameters, viral load values, CD4+ T-cells, vitamin D serum level and number used antiretroviral agents at T0 and T1. No statistical associations between TB and L1–L4 BMD z-scores and biochemical laboratory parameters (such as calcium, alkaline phosphatase, vitamin D, or calciuria) were found.
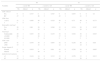
Total body (TB) and lumbar spine (L1–L4) BMD z-score, according to the clinical and immunological classification for HIV infection, viral load, absolute number of CD4+ T-cells, vitamin D serum concentration, and number of antiretroviral regimens.
| T0 | T1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | z-score TB | z-score L1–L4 | z-score TB | z-score L1–L4 | ||||||||
| NL | Altered | p | NL | Altered | p | NL | Altered | p | NL | Altered | p | |
| CDC clinical | ||||||||||||
| NA | 9 | 0 | 0.537 | 8 | 1 | 0.587 | 9 | 0 | 0.655 | 9 | 0 | 0.3 |
| BC | 47 | 2 | 46 | 3 | 45 | 1 | 41 | 5 | ||||
| CD4 class | ||||||||||||
| 1 and 2 | 51 | 2 | 0.658 | 49 | 4 | 0.524 | 49 | 1 | 0.75 | 46 | 4 | 0.373 |
| 3 | 5 | 0 | 5 | 0 | 5 | 0 | 4 | 1 | ||||
| Detectable viral load | ||||||||||||
| Yes | 29 | 1 | 0.96 | 29 | 1 | 0.268 | 32 | 0 | 0.234 | 30 | 2 | 0.387 |
| No | 27 | 1 | 25 | 3 | 22 | 1 | 20 | 3 | ||||
| Viral load | ||||||||||||
| Undetectable | 29 | 1 | 0.835 | 29 | 1 | 0.235 | 32 | 0 | 0.016 | 30 | 2 | 0.645 |
| <10,000 | 20 | 1 | 18 | 3 | 17 | 0 | 15 | 2 | ||||
| ≥10,000 | 7 | 0 | 7 | 0 | 5 | 1 | 5 | 1 | ||||
| CD4 count | ||||||||||||
| ≤500 | 41 | 1 | 0.479 | 39 | 3 | 0.697 | 42 | 0 | 0.236 | 40 | 2 | 0.08 |
| >500 | 15 | 1 | 15 | 1 | 12 | 1 | 10 | 3 | ||||
| Serum vitamin D | ||||||||||||
| Normal | 5 | 0 | 0.834 | 5 | 0 | 0.69 | 42 | 0 | 0.236 | 38 | 4 | 0.663 |
| Altered | 51 | 2 | 49 | 4 | 12 | 1 | 12 | 1 | ||||
| Antiretroviral regimens | ||||||||||||
| <3 | 13 | 1 | 0.434 | 14 | 0 | 0.312 | 13 | 1 | 0.259 | 13 | 1 | 0.613 |
| ≥3 | 42 | 1 | 39 | 4 | 40 | 0 | 36 | 4 | ||||
NL, normal; BMD, bone mineral density; CDC, Centers for Disease Control and Prevention; HIV, human immunodeficiency virus; L1–L4, lumbar spine L1–L4; TB, total body.
Sufficient bone mass gain by 12 months was defined as an increase in 5% in prepubertal patients and between 10 and 15% in pubertal ones. Although most patients had normal BMD z-scores, the bone mass gain was not adequate in 65.5%.
At T0 serum phosphate levels (p<0.001) and vitamin D concentrations (p=0.021) were increased whereas PTH (p<0.001) and alkaline phosphatase (p<0.001) were reduced in relation to T1 values. There was no association between race and vitamin D alteration (p=0.27).
Regarding vitamin D serum concentrations, 21 (36.2%) and 37 (67.3%) patients had insufficient concentrations at T0 and T1, respectively, and 29 patients (50%) had deficient vitamin D concentrations at T0 and 13 (23.6%) at T1.
Calcium and vitamin D intakes were deficient in 54 (98.2%) and 24 (43.6%) patients, respectively. There was no association between TB and L1–L4 BMD z-scores at T0 and T1 with calcium, magnesium, phosphate, caffeine, or calorie and protein intakes. Insufficient intake of vitamin D was associated with low TB (p=0.04) and low L1–L4 (p=0.017) BMD z-scores. Insufficient intake of vitamin A was associated with low TB (p=0.04) BMD z-score.
DiscussionIn this cohort of children and adolescents with HIV infection (predominantly vertical infection), with a long follow-up period and exposure to antiretroviral drugs, the majority did not present with low bone mass (defined as a BMD z-score<−2 SD) during the study.
The results of the present study differ from those previously published, as we found a smaller frequency of alteration in bone mass. Puthanakit et al. found 24% of adolescents infected with HIV had L1–L4 BMD z-scores≤−2 SD. The factors associated with such alteration were undetectable viral load and disease severity.9
Likewise, we found an association between low BMD and higher HIV viral load. Bunders et al. evaluated BMD in HIV-infected children (two to three years of age) and noticed an association between increased BMD z-scores and higher viral loads.10 Battalora et al. reported, in three longitudinal studies, a reduction in TB BMD.11 Lima et al. found no association between calcium intake, immunological classification, or detectable viral load and BMD alterations. However, the group of patients who were included in this study had less immunosuppression.12 Viral replication is an antigenic stimulus for the release of inflammatory cytokines. Increase of viral HIV proteins (gp120, tat and Vpr) and cytokines have been associated with decreased osteoblast function and increased osteoclast activity.13
Viral proteins can also be associated with apoptosis of osteoblasts and disregulation of RANK.11 Jacobson et al. found lower BMD z-scores in HIV infected patients compared to uninfected patients and found a significant association between lower BMD z-scores and CDC B or C classification and age above 8 years.14
In this study BMD alterations were not related to neither type and duration of antiretroviral therapy nor to duration of infection. Some authors have reported an association between BMD z-scores and antiretroviral therapy.10,15 A Brazilian study involving 74 HIV infected adolescents found 32.4% lower bone mass and lower TB and L1–L4 BMD among patients who received tenofovir.16 Studies with adult patients on tenofovir found BMD alteration secondary to hypophosphatemia, which may be due to drug nephrotoxicity.13,17
Evaluation of young HIV infected adults (25–45 years) showed a positive correlation between duration of the infection (in years) and BMD, which suggests that the virus has a deleterious effect on bone metabolism independent of antiretroviral therapy.5
There were no bone fractures in this study which may have been due to the low number of patients with BMD z-scores≤−2 SD and to the improvement in bone quality during childhood. In adults, the risk of fractures is 50% higher in HIV infected patients than in uninfected individuals.11
Several studies have reported a high prevalence of patients with deficient or insufficient vitamin D levels,2,18–23 which was not confirmed in the present study.
Prolonged exposure to protease inhibitors and efavirenz can also result in alterations of vitamin D concentration.24 However, we found no association between decreased vitamin D concentration with neither use of antiretroviral drugs nor race.
On the other hand, an association between low vitamin D concentration and detectable viral load was observed, in agreement with a study by Kim et al. These authors attributed the association to possible interactions between HIV viremia and lipopolysaccharides, pro-inflammatory cytokines, and toll-like receptors that induce 25-hydroxyvitamin D 1a-hydroxylase, resulting in a decreased vitamin D levels.25,26
Some of the limitations encountered in this study are related to the absence of a control group and to the small sample size. Furthermore, other factors that might have influenced bone health such as breastfeeding, prematurity, and low weight gain during the first years of life, were not taken into account. Another important factor that was not considered was the duration of undetectable viral load, which could be associated with different degrees of inflammation.
A low bone mass gain during the course of a year indicates that dietary guidance, physical activity, and exposure to sunlight, as well as administration of calcium and vitamin D supplements, must be reinforced. As it is the case with other chronic diseases, with the decrease in mortality from HIV infection, the challenges become controlling morbidity and preventing future health complications.
FundingFundação de Auxílio à Pesquisa do Estado de São Paulo n° 2011/20882-2.
Conflict of interestThe authors declare no conflicts of interest.