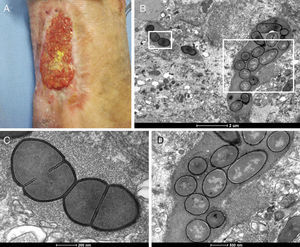
Venous leg ulcer (VLU) is a type of chronic wound that can take a long time to heal, being the most advanced presentation of chronic venous insufficiency (CVI).1 VLUs are usually recurrent, affecting work productivity, quality of life and high public health care treatment costs. It is estimated that VLUs affect up to 1% of the adult population.1 These chronic wounds are usually infected by a diverse microbial flora, which may probably contribute to the nonhealing phenotype.2 A study developed at the university hospital of the Federal University of Minas Gerais, Belo Horizonte, Brazil, included patients with VLU to investigate the presence of bacterial biofilm. A VLU biopsy was performed in a total of 45 patients who had not used antibiotics and presented signs of CVI, such as edema, varicose veins, hyperpigmentation, and lipodermatosclerosis (Fig. 1A). The samples were submitted to bacteriological tests to characterize the bacterial flora and examined by transmission electron microscopy (TEM) to assess the presence of biofilm. The presence of one or two of following bacterial species was identified: Staphylococcus aureus, Pseudomonas aeruginosa, Proteus mirabilis, and Escherichia coli. TEM showed the presence of numerous spherical and/or rod-shaped bacteria (Fig. 1B). Biofilm synthesis was evidenced by a dense extracellular matrix closely associated with bacterial cells (Fig. 1C and D). This matrix contained bacterial polysaccharides, proteins and DNA, providing structural protection and increasing bacterial resistance to natural antibodies, phagocytic inflammatory cells, antibiotics and antiseptics.3 Cell septum formation was also observed indicating that bacterial cells were dividing and bacterial colonization was well-established in wounds (Fig. 1C). The presence of bacterial biofilm in chronic wounds may explain why they do not heal despite adequate care and it may give us new insights for investigations that may lead to new treatments.
Bacterial biofilm in chronic venous ulcer. (A) Venous leg ulcer of a 33-year-old woman with a history of deep vein thrombosis in the left leg and pulmonary embolism. This wound was present in left medial malleolus for two years, showing 15.37cm2 and 40% of yellow necrotic tissue. (B) Bacterial colonies showing spherical and rod-shaped cells seen by transmission electron microscopy. (C and D) Bacteria surrounded by a dense extracellular matrix.
The authors declare no conflicts of interest.
FAPEMIG.