Evaluate the association of Helicobacter pylori infection with anti-parietal cell antibodies (APCA) and anti-intrinsic factor antibodies (AIFA) and their impact on vitamin B12 serum level.
Patients and methodsOne hundred patients (M/F: 43/57; age 46.5±17.5 years) who underwent upper gastrointestinal endoscopy at King Abdullah University Hospital, Irbid, Jordan were enrolled in the study. The patients were grouped as H. pylori-infected (n=81) or H. pylori negative (n=19) by histopathological examination. Fasting serum vitamin B12 levels, anti-parietal cell antibodies and anti-intrinsic factor antibodies for patients and controls were determined.
ResultsAnti-parietal cell antibodies and anti-intrinsic factor antibodies were positive in 9.9% and 18.5% of H. pylori-positive patients respectively. None of the H. pylori negative subjects had anti-parietal cell antibodies or anti-intrinsic factor antibodies. Serum vitamin B12 level was lower in the H. pylori-infected patients (275±70.4pg/mL) than in controls (322.9±60.7pg/mL; p<0.05). H. pylori was positive in 94% of the low-vitamin B12 group compared with 64.6% of the normal-vitamin B12 group (p<0.5).
ConclusionPatients with H. pylori infection are more likely to have anti-parietal cell antibodies and anti-intrinsic factor antibodies. There was an association between H. pylori infection and lower vitamin B12 levels. H. pylori infection might be a significant factor in the pathogenesis of autoimmune gastritis.
Helicobacter pylori is a Gram negative bacterium that colonizes the stomach. Prevalence rates of H. pylori infection varies by age, country of origin, and socioeconomic status. The prevalence of H. pylori infection in northern Jordan is 82%.1 Worldwide, H. pylori infection affects 50% of the population.2H. pylori usually causes asymptomatic gastric infection. Chronic gastritis, peptic ulcer disease, and atrophic gastritis are recognized consequences of this infection. Although H. pylori infection causes gastric inflammation virtually in all infected subjects, the majority of infected subjects remain asymptomatic, while certain subset of patients develops atrophic gastritis.3 There is growing evidence of the relationship between low serum vitamin B12 and H. pylori infection,4,5 suggesting that vitamin B12 deficiency, especially in developing countries, is frequently caused by chronic H. pylori gastritis.6–8 In fact, high frequency of suboptimal serum vitamin B12 level has been found in adults in Jordan.9
Antibodies to intrinsic factor (AIFA), which block the binding of cobalamin to intrinsic factor, have been reported in 31–76% of patients with pernicious anemia.10 Anti-parietal cell antibodies (APCA) are associated with atrophic gastritis, and often occur in subjects with gastritis in the absence of pernicious anemia.11,12
The main objective of this study was to evaluate the association of H. pylori infection with APCA and AIFA, and their impact on serum vitamin B12 level.
Patients and methodsThis study was approved by the Institutional Review Board of Jordan University of Science and Technology and King Abdullah University Hospital (KAUH). The study was prospectively conducted at King Abdullah University Hospital, Irbid, Jordan from June 2007 to June 2008. Patients who were referred for upper gastrointestinal endoscopic examination (UGE) for dyspeptic complaints were enrolled in this study. All the patients signed a written consent form. Patients were excluded from this study if they had any of the following: prior eradication therapy for H. pylori, history of gastrointestinal bleeding, history of gastric surgery, vitamin B12 supplementation in the past three years prior to their enrollment, or pregnancy.
An UGE was performed and at least two biopsy specimens were obtained from the antrum and corpus of the stomach. The biopsy tissue was prepared with hematoxylin and eosin, Giemsa staining, and toludine blue to identify H. pylori. Findings of gastric atrophy and H. pylori were recorded. Histopathological examination was performed independently by two experienced pathologists.
Venous blood sample was taken from each patient at the time of UGE for determination of serum vitamin B12 level, APCA and AIFA. Serum vitamin B12 level was determined by using an auto analyzer instrument (Elecseys, USA). Serum vitamin B12 level less than or equal to 200pg/mL was considered low, while serum level above 200pg/mL was considered normal.
APCA were determined by indirect fluorescent antibody tests by using a commercially available kit (The Binding Site Ltd., UK). AIFA were determined by using a commercially available kit (AIFA, Organic, Germany) based on enzyme-linked immune-sorbent assay (ELISA).
Statistical analysisThe statistical analysis was performed using computerized Statistical Package for Social Science (SPSS) program for windows, version 15, and EpiCal program. Numeric values were expressed as mean values±SD. p-Values were calculated by using two-tailed t-test to compare the difference of means between two groups. The difference was considered statistically significant if the p-value was ≤0.05.
ResultsA total of one hundred patients met the inclusion criteria and agreed to participate in the study. H. pylori was positive in 81 patients (81%), 57% were male, mean age of 46 years (range 18–90); H. pylori was negative in 19 patients (19%), 58% were male, mean age of 47 years (range 21–78).
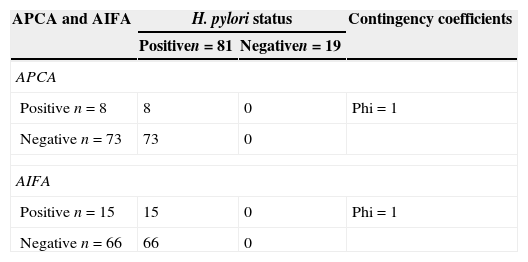
Gastric atrophy was present in 30 (37%) H. pylori-positive and in none H. pylori-negative patients (p=0.91). APCA were present in 8 (9.9%) H. pylori-positive and in none H. pylori-negative patients (p=0.34). AIFA were present in 15 (18.5%) H. pylori-positive and in none H. pylori-negative patients (p=0.09). APCA and AIFA were only present in H. pylori-infected patients. Using phi coefficient to measure of the degree of association, there was a strong association between both APCA and AIFA and the presence of H. pylori infection (Phi=1) (Table 1).
Association of APCA and AIFA with H. pylori infection.
| APCA and AIFA | H. pylori status | Contingency coefficients | |
|---|---|---|---|
| Positiven=81 | Negativen=19 | ||
| APCA | |||
| Positive n=8 | 8 | 0 | Phi=1 |
| Negative n=73 | 73 | 0 | |
| AIFA | |||
| Positive n=15 | 15 | 0 | Phi=1 |
| Negative n=66 | 66 | 0 | |
APCA, anti-parietal cell antibodies; AIFA, anti-intrinsic factor antibodies.
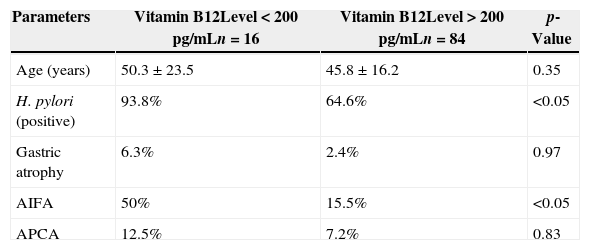
Serum vitamin B12 level was 257.6±79.4pg/mL in H. pylori positive and 322.9±60.7pg/mL in H. pylori-negative patients (p<0.05). Low vitamin B12 was found in 16 patients (16%). H. pylori was positive in 94% among those with low vitamin B12 level compared to 64.6% of those with normal level (p<0.5). AIFA were detected among 50% of those with low vitamin B12 level and in 15.5% of those with normal level (p<0.5) (Table 2).
Parameters associated with serum levels of vitamin B12.
| Parameters | Vitamin B12Level<200pg/mLn=16 | Vitamin B12Level>200pg/mLn=84 | p-Value |
|---|---|---|---|
| Age (years) | 50.3±23.5 | 45.8±16.2 | 0.35 |
| H. pylori (positive) | 93.8% | 64.6% | <0.05 |
| Gastric atrophy | 6.3% | 2.4% | 0.97 |
| AIFA | 50% | 15.5% | <0.05 |
| APCA | 12.5% | 7.2% | 0.83 |
APCA, anti-parietal cell antibodies; AIFA, anti-intrinsic factor antibodies.
The present study disclosed certain association between AIFA and H. pylori infection. Additionally, results from this study showed increased APCA positivity among H. pylori-infected patients, but not among H. pylori-negative patients. The presence of APCA might be a host factor that contribute to the final outcome of chronic H. pylori infection.13 These results are consistent with other studies.14 Lo et al.,15 in their prevalence study of APCA and anti-H. pylori antibodies (AHPA) in patients with gastric adenocarcinoma, found that the prevalence rates of APCA and AHPA were 70% and 53%, respectively, while the prevalence was much lower in controls. The authors concluded that APCA and AHPA can predict atrophic gastritis and, consequently, gastric cancer. In our study, the association was not statistically significant, possibly due to the small sample size, thus reducing the statistical power of the test.
A controlled Italian study16 of asymptomatic subjects with APCA and patients with pernicious anemia found atrophic gastritis on histopathological examination in 18% of asymptomatic APCA subjects, in 75% of patients with pernicious anemia, and only in 3% of controls. In this study, H. pylori was found in 61% of patients without gastric atrophy, while only 19% of patients with atrophy were positive for H. pylori. This result could be explained by the reduction of H. pylori infection as acid secretion decreases. The authors of this Italian study concluded that the frequent detection of H. pylori in subjects with early autoimmune gastritis suggests that H. pylori could have a role in the induction and/or maintenance of autoimmunity at the gastric level. Similar to the above study, we found some association between H. pylori infection and markers of autoimmune gastritis, suggesting that H. pylori infection could trigger gastric autoimmunity.
Initial data showed no significant differences between males and females investigated in this study. Therefore, all data presented here are for both genders combined.
Our study included 100 patients referred for UGE to investigate symptoms of dyspepsia. Eighty-one patients proved to have H. pylori infection by histopathological examination of gastric biopsies. The other 19 patients were found to be H. pylori negative by histopathological examination. This finding is consistent with other studies from Jordan which showed a prevalence rate of H. pylori infection to be around 80%.1
Concerning the presence of AIFA, results from this study demonstrated higher prevalence in H. pylori-infected patients. To our knowledge, no previous studies were conducted to evaluate the prevalence of AIFA in H. pylori-infected patients. Moreover, the presence of AIFA was strongly associated with lower vitamin B12 serum level (p<0.05).
Comparing serum vitamin B12 levels in patients infected and not infected with H. pylori showed a significant difference, with lower serum vitamin B12 level in the infected group (p-value<0.05).
Patients with low serum vitamin B12 level had high prevalence of gastric atrophy and APCA, but this was not statistically significant. AIFA prevalence in patients with low serum level of vitamin B12 was statistically significant (p<0.05).
In our study we found a significant association between H. pylori infection, AIFA and APCA. It appears that these antibodies are only present in H. pylori-infected patients. Based on the results of our study, it is arguable that H. pylori infection could lead to autoimmune gastritis, as reported by other investigators.17
The limitation of this study is the small sample of control individuals, because of the very high prevalence of H. pylori infection in Jordan. This could have led to the lack of statistically significant differences between H. pylori-infected patients and controls. Another limitation of our study is the lack of clinical parameters of vitamin B12 deficiency.
In conclusion, our study showed a strong association between H. pylori infection and the presence of antibodies to gastric parietal cell and to intrinsic factor. AIFA is associated with low serum level of vitamin B12. Therefore, a putative relationship between H. pylori infection and gastric autoimmunity is suggested. However, we believe that large-scale age-matched prospective studies are required to establish the definite association between APCA, AIFA, H. pylori infection and B12 deficiency.
Conflicts of interestThe authors declare no conflicts of interest.