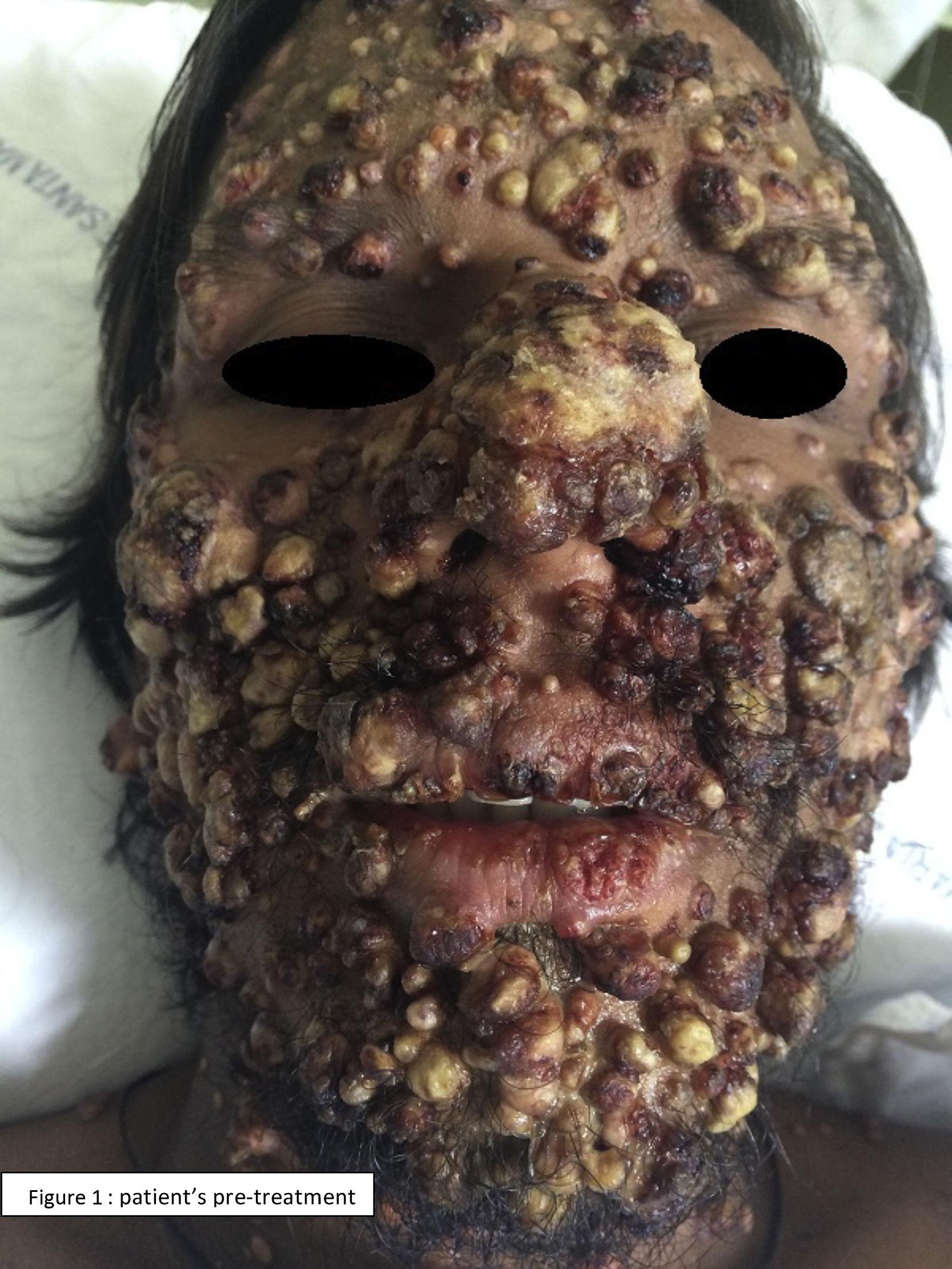
A 37-year-old man with AIDS on antiretroviral therapy, from south of Brazil, was admitted to the hospital with dyspnea and fever. He exhibited umbilicated papulonodular lesions, resembling molluscum contagiosum lesions, scattered in the face, trunk, and lower and upper limbs, associated painful ulcers in the oral cavity and genital region. A direct mycological exam identified fungal elements suggestive of Histoplasma. Histopathological examination demonstrated a granulomatous inflammatory process with massive presence of fungal structures compatible with Histoplasma capsulatum. A fibrobronchoscopy was also performed revealing small and round leveduriform structures with morphological characteristics consistent with Histoplasma in a patient with CD4 T-lymphocyte count of 77/mm3. Treatment with Amphotericin B was initiated. The patient progressed with favorable clinical recovery after five weeks, when treatment was switched to Itraconazole. This case illustrates an exuberant form of disseminated histoplasmosis. The systemic mycosis caused by H. capsulatum is endemic in central and South America. The infection occurs by direct inhalation of fungal spores that are present in soil contaminated with excrements of birds and bats. The clinical manifestation varies according to the immune status of the host and load of exposure. The acquired immunosuppression due to HIV is the major risk factor for disseminated histoplasmosis, which includes pulmonary disease, systemic endothelial-reticular involvement and skin lesions. Cutaneous lesions occur in a wide variety of forms, none of which characteristic of the infection, and result from hematogenic dissemination. Diagnosis can be performed by a biopsy of mucosal or cutaneous lesion (the most rapid method to specific diagnosis), with direct mycological examination and culture. Treatment consists of an induction phase with amphotericin B (standard treatment) followed by 12 months of Itraconazole (maintenance phase) (Figs. 1 and 2).
Conflict of interestThe authors declare no conflicts of interest.
- Home
- All contents
- Publish your article
- About the journal
- Metrics