Among patients infected with the human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS), alcohol use can have negative effects on their survival. Alcohol can aggravate immunosuppression, increase liver toxicity of antiretroviral therapy (ART), and alcohol consumption may reduce patient adherence to ART, which can lead to resistance to antiretrovirals and a decrease in ART effectiveness.1
The present cross-sectional study aimed to assess alcohol consumption among patients with HIV/AIDS and factors associated with this consumption. A total of 108 patients [58 (53.7%) males] with HIV infection or AIDS, with a mean age of 42.7±9.4 years (25–75 years), were assessed prospectively and consecutively at the Clinical Hospital of the Federal University of Uberlândia, in the city of Uberlândia, state of Minas Gerais, Southeastern Brazil. Socio-demographic data, data on adherence to ART and data on risky sexual behavior were collected. Alcohol consumption was assessed through the Alcohol Use Disorders Identification Test (AUDIT)2 and Cut-down, Annoyed, Guilty and Eye-opener (CAGE)3 questionnaires. The AUDIT identifies alcohol use in the previous 12 months and, during this period, all individuals included in the study had already received the HIV/AIDS diagnosis; it is recommended that all individuals with an AUDIT score ≥8 should be considered as a hazardous alcohol drinker.2 The CAGE questionnaire was applied to identify alcohol abuse or dependence during the periods of life prior to and following the HIV/AIDS diagnosis. Furthermore, risky sexual behavior with or without alcohol use before sexual intercourse, and the possible reasons for ART interruptions were also evaluated. This research project was approved by the institutional research ethics committee and an informed consent form was signed by each patient for their participation.
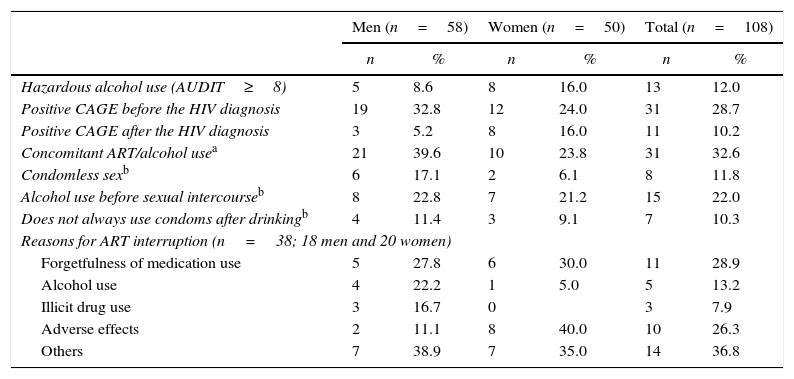
It was observed that 8.6% of men and 16% of women had a hazardous alcohol consumption. During the period of life prior to the diagnosis of HIV infection or AIDS, 32.8% of males and 24% of females had a positive CAGE; during the period following this diagnosis, CAGE was positive among 5.2% of men and 16% of women. Out of the 95 patients undergoing ART, 39.6% of males and 23.8% of females consumed alcohol. Among those who interrupted ART, 13.2% discontinued due to alcohol consumption, which was the second main reason to interrupt ART among men (22.2%). Among patients with an active sexual life, 17.1% of men and 6.1% of women did not use or did not always use condoms, 22.8% and 21.2% frequently consumed alcohol before sexual intercourse, and 11.4% and 9.1% did not always use condoms after drinking (Table 1). The CAGE score of four patients (one man and three women) became positive after the diagnosis of infection with HIV.
Alcohol consumption and associated factors among patients with HIV/AIDS.
| Men (n=58) | Women (n=50) | Total (n=108) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Hazardous alcohol use (AUDIT≥8) | 5 | 8.6 | 8 | 16.0 | 13 | 12.0 |
| Positive CAGE before the HIV diagnosis | 19 | 32.8 | 12 | 24.0 | 31 | 28.7 |
| Positive CAGE after the HIV diagnosis | 3 | 5.2 | 8 | 16.0 | 11 | 10.2 |
| Concomitant ART/alcohol usea | 21 | 39.6 | 10 | 23.8 | 31 | 32.6 |
| Condomless sexb | 6 | 17.1 | 2 | 6.1 | 8 | 11.8 |
| Alcohol use before sexual intercourseb | 8 | 22.8 | 7 | 21.2 | 15 | 22.0 |
| Does not always use condoms after drinkingb | 4 | 11.4 | 3 | 9.1 | 7 | 10.3 |
| Reasons for ART interruption (n=38; 18 men and 20 women) | ||||||
| Forgetfulness of medication use | 5 | 27.8 | 6 | 30.0 | 11 | 28.9 |
| Alcohol use | 4 | 22.2 | 1 | 5.0 | 5 | 13.2 |
| Illicit drug use | 3 | 16.7 | 0 | 3 | 7.9 | |
| Adverse effects | 2 | 11.1 | 8 | 40.0 | 10 | 26.3 |
| Others | 7 | 38.9 | 7 | 35.0 | 14 | 36.8 |
AUDIT, Alcohol Use Disorders Identification Test; CAGE, Cut-down, Annoyed by Criticism, Guilty and Eye-opener; ART, antiretroviral therapy.
The present study showed a reduction in the number of patients with positive CAGE after the HIV/AIDS diagnosis, although this reduction was small among women. Moreover, it should be emphasized that the CAGE of certain patients, particularly women, became positive after the diagnosis of HIV infection. The AUDIT showed high prevalence of hazardous alcohol consumption among the patients evaluated, and alcohol consumption was frequent among those on ART.
Alcohol use was an important cause of ART interruption, particularly among men. Although HIV-related morbidity and mortality have significantly decreased with the use of highly active antiretroviral therapy (HAART), the effectiveness of this treatment depends on patient adherence to antiretroviral medications.1 Alcohol use has been associated with ART nonadherence in several studies, but the strength and causality of these relationship needs to be better characterized.1 In Brazil, two recent studies found no significant association between alcohol use and nonadherence to ART.4,5 However, one study observed higher risk of nonadherence in patients reporting association of alcohol intake and use of illicit drugs or high-intensity alcohol use.4
In addition, it was observed that alcohol consumption increased the chances of high-risk sexual behavior. These results show that the need for the recognition of alcohol consumption among patients with HIV/AIDS should not to be neglected by the health team caring for them. The association between alcohol use and socio-demographic data was not analyzed so that stereotypes would not be made, as all patients needed to be asked about alcohol consumption. The results of this study also emphasize the need to identify alcohol abuse among women. Assessing alcohol consumption using specific instruments enables the identification of less evident cases of alcohol abuse. Patients with HIV/AIDS with problematic alcohol use may require specialized treatment or even multi-disciplinary team follow-up.
FundingFundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG), PIBIC/FAPEMIG/UFU.
Conflicts of interestThe authors declare no conflicts of interest.