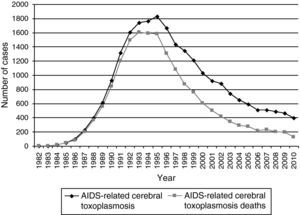
Highly active antiretroviral therapy (HAART) significantly reduced the cerebral toxoplasmosis incidence in HIV-infected patients from high-income countries.1 However, there is scarce epidemiological information about this neurological opportunistic disease in low- and middle-income countries, including Brazil. In this letter, we would like to report some issues about AIDS-related cerebral toxoplasmosis in São Paulo State, Brazil. First, cerebral toxoplasmosis is the third ranking AIDS-defining disease in the HAART-era,2 representing 10% of admissions at Instituto de Infectologia Emilio Ribas (IIER) and 10% (n=3224) of reported cases among 2001–2005 to the Division of Epidemiology Surveillance of the Centro de Referência em Treinamento em DST/AIDS from São Paulo State.3 Second, cerebral toxoplasmosis led to the diagnosis of HIV infection in 35% of cases, and it defined AIDS in 75% of cases admitted at IIER, suggesting a loss of diagnostic and therapeutic opportunities in a subset of HIV-infected persons in Brazil, a middle-income country with universal and free access to HAART.2 Third, short and long-term follow-up data at IIER showed similar outcomes compared with AIDS-related cerebral toxoplasmosis from developed countries.1,2 However, cerebral toxoplasmosis remains a condition with poor prognosis in the natural history of HIV-infected persons.1,4 Fourth, cases reported to the Division of Epidemiology Surveillance of the Centro de Referência em Treinamento em DST/AIDS from São Paulo State, showed a progressive decline of notified cases of AIDS-related cerebral toxoplasmosis during the HAART-era. Fig. 1 shows the evolution of the number of cases from 1982 to 2010 with 1825 reported cases in 1995 and declining to 392 cases in 2010. In addition, Fig. 1 shows a consistent declining of the number of reported AIDS-related cerebral toxoplasmosis deaths. Thus, there has been a reduction in the case-fatality rate of cerebral toxoplasmosis from >90% in the pre-HAART-era to ~30% in recent years. In contrast to this data, the case-fatality rate at IIER (a tertiary referral center) was 13%, suggesting the heterogeneity of outcomes among the several facilities.2 Fifth, similar to that reported in the United States,4 toxoplasmosis cases dropped markedly in the first years of HAART in São Paulo State, but decreased relatively little in recent years, confirming the persistence of late HIV diagnosis, non-adherence to HAART and/or antiretroviral therapy failure in a subset of HIV-infected patients. A number of strategies to reduce morbidity and mortality among HIV-infected patients were recently reviewed5 and several key principles can be proposed to reduce AIDS-related cerebral toxoplasmosis: (1) early HIV diagnosis; (2) linkage to and retention in care; (3) timely treatment of HIV; (4) adherence to HAART; (5) primary and secondary prophylaxis, and (6) optimized diagnosis and treatment.
Our data confirm that frequency and case-fatality rates of AIDS-related cerebral toxoplasmosis improved markedly after the introduction of HAART. However, urgent implementation or optimization of both individual and public health strategies is necessary to reduce current morbidity and mortality. Although they are particularly vital to address in low and middle-income countries, the challenges of AIDS-related cerebral toxoplasmosis are global.1,4–6 A complete eradication of this parasitic disease is unlikely, but a comprehensive approach to improve components of engagement in HIV will determine the impact of this opportunistic disease in the future.
Conflict of interestAll authors declare to have no conflict of interest.
We would like to thank Marcia Polon from the Division of Epidemiology Surveillance of the Centro de Referência em Treinamento em DST/AIDS from São Paulo State, Brazil, for the data about AIDS-related cerebral toxoplasmosis from São Paulo State.