We identified a case of pleomorphic post kala-azar dermal leishmaniasis (PKDL) with different types of skin lesions in different stages of development. He was earlier diagnosed as a case of lepromatous leprosy on the basis of his skin picture and was treated with anti-leprotic drugs for one year in his native village, but without any improvement. We diagnosed him as a case of PKDL on clinical grounds, skin biopsy showing LD bodies and positive DNA-PCR from different types of skin lesions.
Now he improved dramatically with miltefosine in standard dose for one month; and was continued on the medicine for the recommended duration.
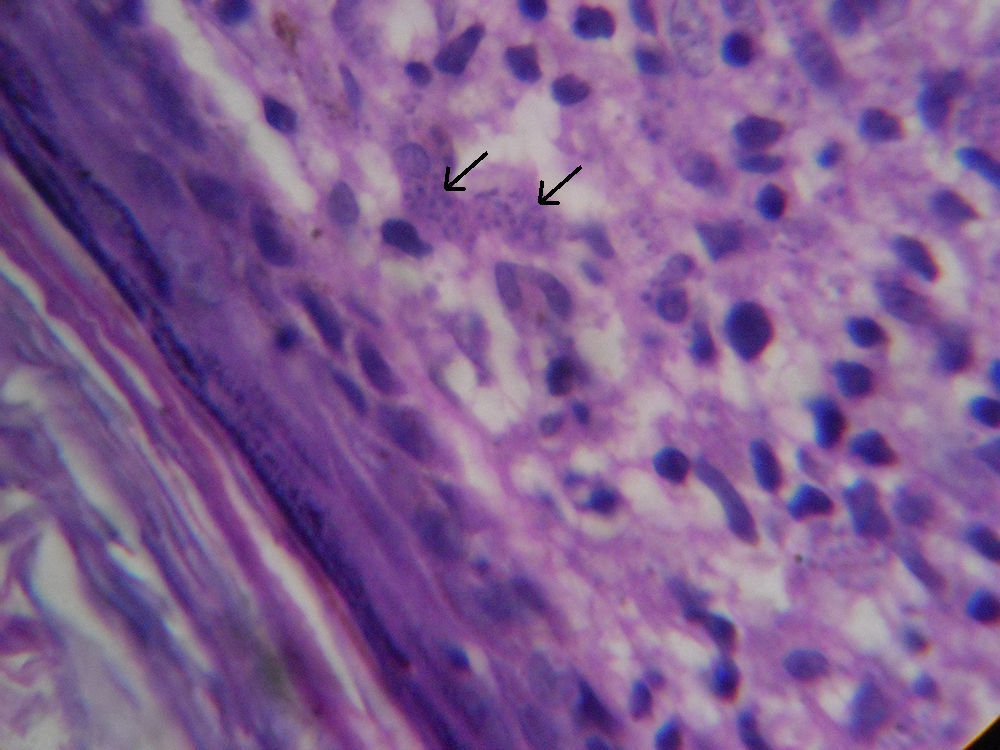
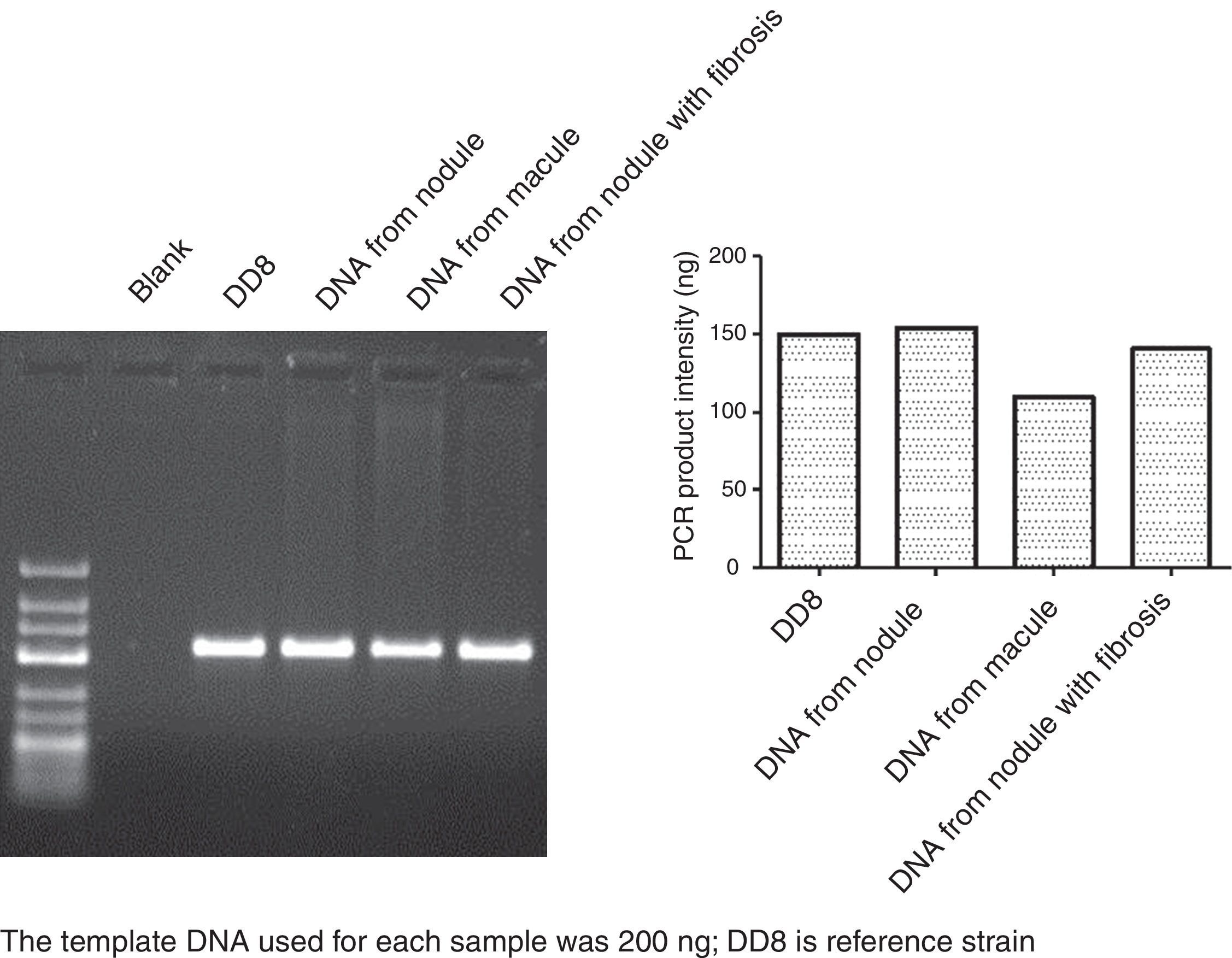
Case proper: A 30-year-old tribal farmer from a remote village of Bihar; a state in eastern India, known to be endemic for leishmaniasis, presented with multiple painless, non-pruritic, progressively increasing hypopigmented macular, papular (Fig. 1), plaque-type, nodular and nodules with central scar over different areas of his body including face, back, upper and lower extremities (Fig. 2A, B) for last one and half years. He first attended a nearby government hospital and was treated there as a case of lepromatous leprosy with multi-drug therapy for one year without any improvement. He presented to us with his progressing skin lesions. On enquiry, he gave a history of prolonged fever with abdominal swelling ten years back for which he was treated with 30 intramuscular injections in his local hospital (probably sodium stibogluconate). He had mild anemia, no significant lymphadenopathy. There was no sensory impairment over the skin lesions or distal limbs. He also did not have any thickening of peripheral nerves. Systemic examination was unremarkable. Investigations revealed presence of mild microcytic anemia. Biochemical tests were normal except slight elevation of serum globulin. VDRL, Hepatitis B, C and HIV serology were all negative. rK39 strip test was negative. Skin snipe from nodule in face was positive for LD bodies, but negative from macular lesions. Skin snipe smear was negative for AFB. Chest X-ray and USG abdomen were normal. Histopathology revealed sub-epidermal clear zone, lymphoplasmacytic granuloma with the presence of LD bodies in Giemsa Stain (Fig. 3). DNA-PCR study of skin biopsy specimen from macular, nodular and scarred lesions (Fig. 5) showed similar degree of positivity for Leishmania donovani DNA. As patient refused injections, we treated him with oral miltefosine 50mg twice a day. Photographs taken after one month showed significant clearing of the lesions (Fig. 4A, B). These following unusual features drew our attention a) the presence of three different types of skin lesions in the same patient (pleomorphic), and b) DNA PCR showed similar degree of positivity in three different morphological types of lesions, though the skin snipe was only positive in nodular lesion from face.
The authors declare no conflict of interest.
Dr. Mitali Chatterjee, Ms. Susmita Roy, Ms. Susmita Ghosh from Dept. of Pharmacology, IPGMER, Kolkata for doing the DNA-PCR. Prof. Bibhuti Saha, HOD, Dept. of Tropical Medicine, School of Tropical Medicine, Kolkata.