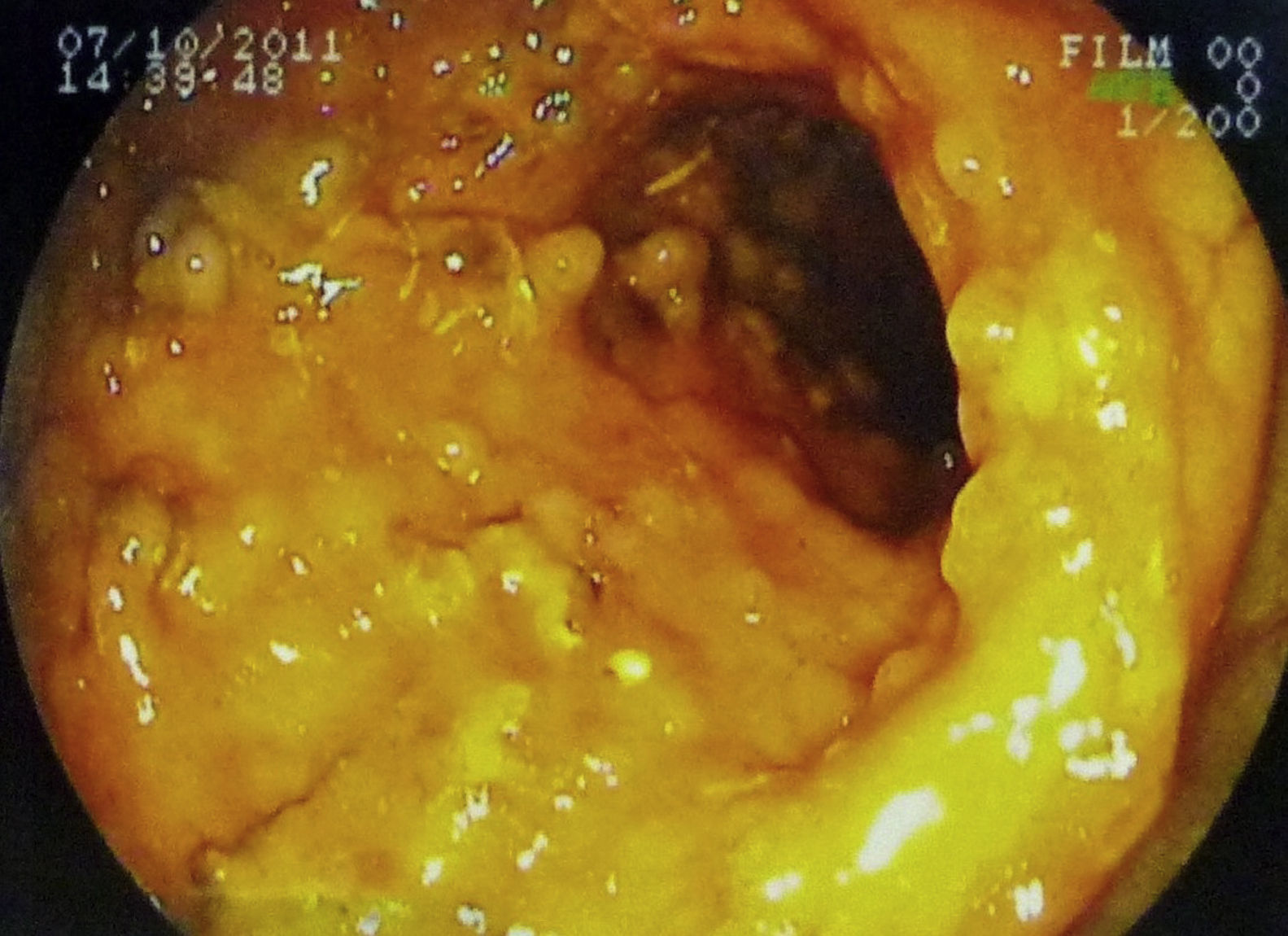
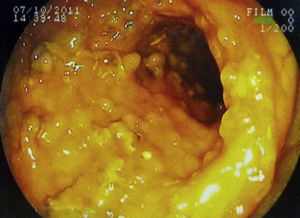
Tuberculosis has a broad array of manifestations. Hemolytic anemia is a rare cause of tuberculosis associated anemia. It is important to recognize given its severe implications. An 18-year-old teenager with a confirmed diagnosis of tuberculosis associated with a positive direct coombs test and anemia, responsive to anti-tuberculosis chemotherapy without the use of corticosteroids is presented. She presented a history of chronic asthenia, weight loss, intermittent fever, night sweats, cough and diarrhea without a history of medication use or transfusions, and was admitted at the Hospital Adriano Jorge, Manaus, Brazil. She appeared emaciated, pale, febrile, tachycardic, and dyspneic. She demonstrated fine rales in the left apex. The laboratory findings showed: hemoglobin 8.3g/dL, hematocrit 27%, MVC 82.1, MCH 25.2, WBC 5.650 (77.4% neutrophils, 11.3% lymphocytes, 10.4% monocytes, 0.9% eosinophiles), platelet count 547,000, positive direct coombs test (IgG), and albumin 2.42g/dL. In three days, the patient demonstrated a drop in her hemoglobin to 6.6g/dL, which responded appropriately to transfusion. Chest X-ray revealed a cavitation in the left pulmonary apex. Chest CT confirmed and also demonstrated a tree-in-bud pattern. Her sputum was positive for acid-fast bacilli (AFB). A PPD test was 20mm. Abdominal CT scan revealed cecum thickening and colonoscopy showed cecal stenosis with diffuse polypoid lesions (Fig. 1). Colonoscopy biopsied culture was positive for Mycobacterium tuberculosis. Standard blood, urine and stool cultures; AFB exam of urine and stool; thick blood smear; anti-nuclear factor and HIV test were all negative. Tuberculosis chemotherapy of rifampicin, isoniazid, pyrazinamide and ethambutol (RIPE) was initiated. The hemoglobin normalized without further transfusions, and the coombs test became negative. Corticosteroids therapy was not necessary. Anemia in tuberculosis is caused by nutritional deficiency, malabsorption and bone marrow suppression.1,2 Hemolytic anemia is rare but important to recognize because the use of immunosuppressants may worsen the infectious process and anti-tuberculosis therapy is the definitive treatment. We describe first a Brazilian patient with tuberculosis and transient hemolytic anemia responsive to tuberculosis chemotherapy without the use of corticosteroids. Both transfusions and anti-tuberculosis drugs are known to cause hemolytic anemia, but, in this case, the hemolysis preceded all interventions. Adults with transient hemolytic anemia secondary to tuberculosis demonstrate a self-limited hemolysis that is responsive to RIPE without corticosteroids.3–7 Children, however, tend to demonstrate a more severe symptomatology that may benefit from corticosteroids. In India, a case was reported of disseminated tuberculosis and hemolytic anemia (Hb 1.8g/dL) in an 8-year-old girl. This patient required transfusions and corticosteroids, but showed clinical improvement only after the start of anti-tuberculosis drugs.8 Gupta et al. reported intestinal tuberculosis and hemolytic anemia (Hb 6g/dL) in an 8-year-old Indian boy who also received corticosteroids but improved only after initiating anti-tuberculosis therapy.9 Normalization of the hematologic parameters only with anti-tuberculosis therapy is proof that tuberculosis should be listed among the infectious causes of hemolytic anemia. Hemolytic anemia can be a fatal complication and, in severe cases, the use of corticosteroids may be indicated but should be used judiciously. Tuberculosis being a common disease, the association with transient hemolytic anemia should be recognized and treated appropriately.
Conflict of interestThe authors have no conflicts of interest to declare.
We thank the patient for authorizing us to use her clinical examination.