Invasive fungal infection (IFI) is frequent in patients with hematologic malignancies or submitted hematopoietic stem cell transplantation (HSCT).
ObjectivesTo evaluate the role of the GM (galactomannan) test in prescribing therapeutic antifungals; to determine invasive aspergillosis (IA) frequency, the factors associated with positive GM test, and the in-hospital mortality.
MethodsWe conducted a retrospective observational study including patients aged 18 or over with hematological malignancy or submitted to HSCT. GM test was measured twice weekly. The hypothesis of IFI was considered in patients with neutropenia and persistent fever despite broad-spectrum antibiotics.
ResultsA total of 496 patients were evaluated; the mean of GM tests performed per patient was 4.2 (+3.1), and 86 (17.3 %) had positive results. IFI was diagnosed in 166 (33.5 %) and IA in 22 (24.6 %) patients. Positive GM test was more frequent in patients with IFI (72.2 % and 25.1 %; OR 8.1; 95 % CI 4.8 - 13.8), and was associated with therapeutic antifungals prescription (52, 9 % and 20.5 %; OR 4.3, 95CI% 2.0 - 9.4), as well as lung abnormalities on HRCT (45.3% vs. 21.5 %; OR 3.0, 95 %CI 1.4 - 6.5). Mortality was 31.6 %. In the multivariate analysis, the variables associated with mortality were the hypothesis of IFI (OR 6.35; 95 % CI 3.63–11.12.0), lung abnormalities on HRCT (57.9 % and 26.9 %; OR 2 0.6; 95 % CI 1.5 – 4.4), and positive GM test (57.9 % and 26.9 %; OR 2.7 95 % CI 1.6 - 4.5).
ConclusionsPositive GM test was associated with lung abnormalities on HRCT and with the introduction of therapeutic antifungals. If adequate anti-mold prophylaxis is available, the GM test should not be used as screening, but to investigate IFI in high-risk patients. The diagnosis of IFI, positive GM test and lung abnormalities on HRCT were predictors of hospital mortality in patients with hematological malignancies or undergoing HSCT.
Invasive Fungal Infection (IFI) is a complication seen in immunosuppressed patients, especially among those undergoing chemotherapy for hematologic malignancies or Hematopoietic Stem Cell Transplantation (HSCT).1-3 Despite the evolution in transplantation procedures and the use of prophylactic antifungals, the incidence of IFI remains high.4,5 Invasive Aspergillosis (IA) is the most common IFI in patients who do not receive effective mold prophylaxis and accounts for approximately 50% of these infections.3 The prognosis of IFI/IA depends on early diagnosis, adequate treatment, and the reversal of the immune alteration. Delay in starting treatment is often associated with increased mortality.5-8 These fungal infections present diagnostic challenges associated with traditional culture and histological examination methods. The diagnosis is based on the combination of the patient's risk factors, clinical symptoms and signs, culture, histopathological exams, and detection of antigenic components of the fungus, such as Galactomannan (GM).9,10 The GM test has a sensitivity of 71% (95% CI 68%‒74%) and specificity of 89% (95% CI 88% and 90%) in patients with IA.11 The GM test has been used to screen high-risk patients or for microbiological confirmation in patients suspected of IFI/IA. GM testing is available in many hospitals, but there are still questions about the role it plays in decision-making related to antifungal treatment in high-risk IFI/IA patients.6,12-14
This study aimed to evaluate the role of the GM test in the prescribing of therapeutic antifungals in patients with hematological malignancies or undergoing HSCT at a university public hospital of the Unified Health System (SUS) to determine the frequency of proven, probable, and possible IA, and to evaluate the factors associated with the positive GM test, antifungal used and in-hospital mortality.
Material and methodsA retrospective observational study was carried out, analyzing medical records. Cases were identified from records at Unicamp's LEMDI (Laboratory of Molecular Epidemiology and Infectious Diseases), which has performed all GM tests since its introduction in 2011. According to the institution's protocol, the test was requested twice a week for neutropenic patients or for patients with a hypothesis of IFI.
The GM test was performed by the ELISA technique (Enzyme-Linked Immuno Sorbent Assay) using the Platelia Aspergillus test (Bio-Rad, Paris, France). The GM test is performed according to the manufacturer's recommendations on blood or bronchoalveolar lavage fluid, and a GM Optical Density Index of 0.5 on two sequential samples is considered positive. The result is available on the day of its completion.
Inclusion criteria were patients aged 18 or over with a diagnosis of hematologic malignancy, hospitalized in the oncohematology wards or in the HSCT unit, who underwent the GM test from 2012 to 2017. All events were included when the patient had more than one hospitalization or episode of neutropenia with GM measurement. Severe neutropenia was considered if the neutrophil count was < 500 cells/mL for more than seven days.
Outcome variables were frequency of IA proven, probable, and possible, factors associated with positive GM tests, use of therapeutic antifungal, and in-hospital mortality, calculated as the ratio of patients who died during hospitalization to the total number of patients included in the study.
Demographic, clinical, laboratory, microbiological, antimicrobial usage, antifungal data, HRCT (High-Resolution Chest Tomography) findings, GM results, and evolution were collected. Information was obtained until discharge or death. Cases were classified according to the probability of IA into proven, probable, and possible infection according to the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium (EORTC/MSG).9
IA possible was assumed when empirical antifungal was prescribed to patients with neutropenia, and persistent fever despite broad-spectrum antibiotics and without microbiological or imaging evidence of IFI.
IA probable was defined in patients with clinical symptoms, altered findings in HRCT, or a positive GM test.
Prophylaxis for IA was considered adequate if the patient received voriconazole or echinocandins. Antifungal treatment was considered adequate when the patient received amphotericin in different formulations or voriconazole.15
Candidemia was diagnosed by blood culture and invasive fusariosis by blood culture or culture of biopsy material.
Considering that patients admitted to the oncohematology ward or HSCT unit could present different risk factors for IFI or for mortality, the initial descriptive analysis was carried out according to the place of hospitalization.
Patients were followed only during hospitalization until discharge or death; therefore, we calculated the in-hospital mortality.
Categorical variables were described as frequency and percentage, and continuous variables as mean and standard deviation. In comparative analyses, the Chi-Square and Student's t-test were used for categorical and continuous variables, respectively. Two-tailed p-values < 0.05 were accepted as statistically significant.
Variables associated with the positivity of the GM test, the use of antifungal, and the evolution to death, at the p-value of 0.05, were included in the logistic regression analysis using the backward conditional technique. IBM SPSS Statistics, version 21.0 for Windows, was used for the statistical analysis.
The collected data were stored in RedCap (Research Electronic Data Capture) https://redcap.fcm.unicamp.br/redcap_v10.9.0/.
The medical ethics committee approved the research (CAAE: 24708019.0.0000.5404).
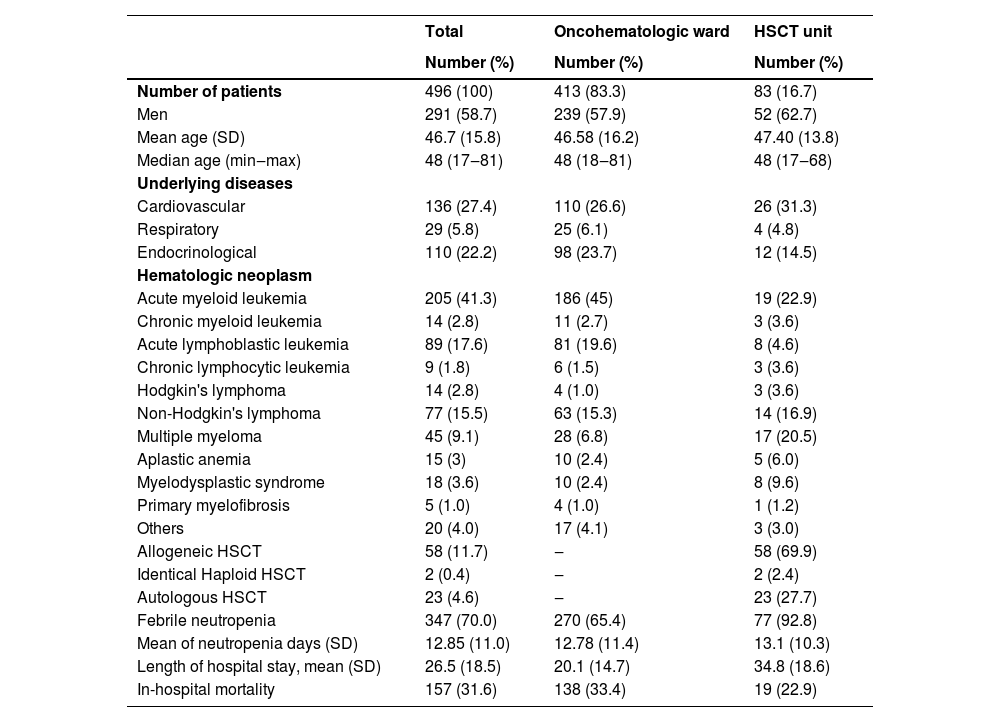
ResultsA total of 496 patients were included, of which 413 (83.3 %) were admitted to the oncohematologic ward and 83 (16.7 %) to the HSCT unit. Patient characteristics, underlying diseases, and duration of neutropenia are described in Table 1.
Clinical and epidemiological characteristics of patients.
HSTC, Hematopoietic Stem Cell Transplantation; SD, Standard Deviation; min‒max, minimal‒maximal.
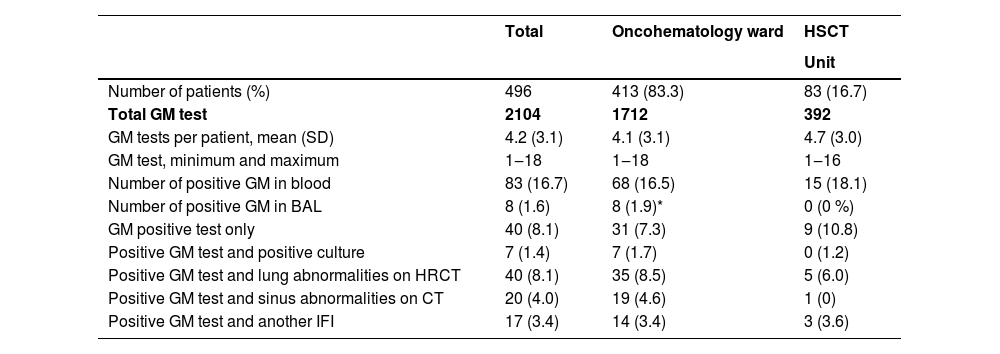
A total of 2104 GM tests were performed, mean of 4.1 (±3.1) per patient. The GM test was positive in 86 patients, representing 23.5 negative tests for one positive. GM was positive in 17 (3.4 %) patients with other fungal infections. Table 2 shows the different combinations of positive GM test with positive culture, HRCT abnormalities in HRCT, and sinus CT among the patients included in the study.
GM test results related to the presence of other findings.
HSTC, Hematopoietic Stem Cell Transplantation; SD, Standard Deviation; GM, Galactomannan; computed tomography; IFI, Invasive Fungal Infection.
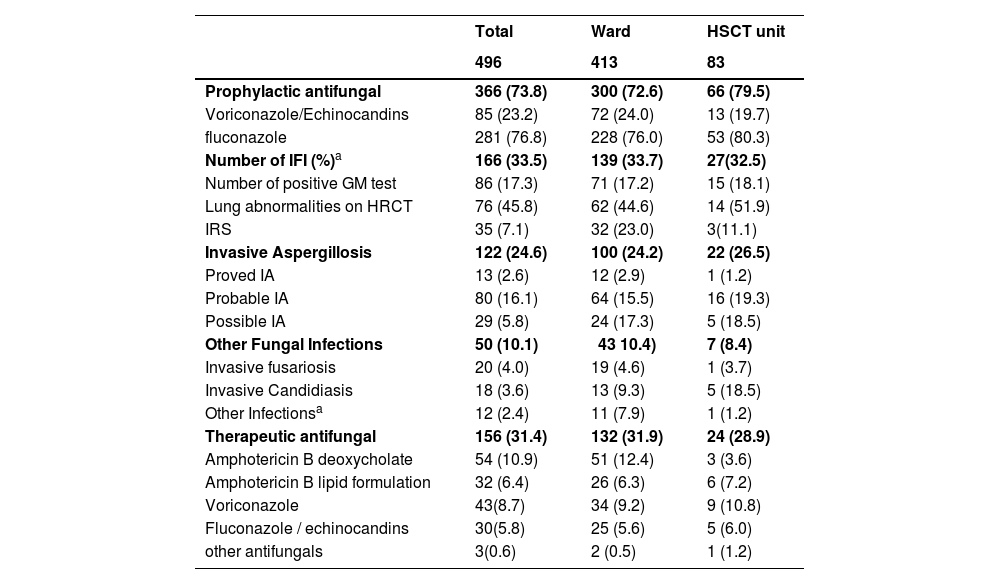
IFI was diagnosed in 166 patients (33.5 %), and six patients had more than one IFI. Lung abnormalities on HRCT were identified in 76 (45.8 %), and Invasive Rhinosinusitis (RSI) in 35 (7.1 %) (Table 3). The main HRCT suggestive findings of IPA (Invasive Pulmonary Aspergillosis) were the presence of nodules in 32 patients (19.5 %) and surrounding areas of ground glass in 30 (18.5 %) patients.
Diagnosis of IFI and antifungal use.
| Total | Ward | HSCT unit | |
|---|---|---|---|
| 496 | 413 | 83 | |
| Prophylactic antifungal | 366 (73.8) | 300 (72.6) | 66 (79.5) |
| Voriconazole/Echinocandins | 85 (23.2) | 72 (24.0) | 13 (19.7) |
| fluconazole | 281 (76.8) | 228 (76.0) | 53 (80.3) |
| Number of IFI (%)a | 166 (33.5) | 139 (33.7) | 27(32.5) |
| Number of positive GM test | 86 (17.3) | 71 (17.2) | 15 (18.1) |
| Lung abnormalities on HRCT | 76 (45.8) | 62 (44.6) | 14 (51.9) |
| IRS | 35 (7.1) | 32 (23.0) | 3(11.1) |
| Invasive Aspergillosis | 122 (24.6) | 100 (24.2) | 22 (26.5) |
| Proved IA | 13 (2.6) | 12 (2.9) | 1 (1.2) |
| Probable IA | 80 (16.1) | 64 (15.5) | 16 (19.3) |
| Possible IA | 29 (5.8) | 24 (17.3) | 5 (18.5) |
| Other Fungal Infections | 50 (10.1) | 43 10.4) | 7 (8.4) |
| Invasive fusariosis | 20 (4.0) | 19 (4.6) | 1 (3.7) |
| Invasive Candidiasis | 18 (3.6) | 13 (9.3) | 5 (18.5) |
| Other Infectionsa | 12 (2.4) | 11 (7.9) | 1 (1.2) |
| Therapeutic antifungal | 156 (31.4) | 132 (31.9) | 24 (28.9) |
| Amphotericin B deoxycholate | 54 (10.9) | 51 (12.4) | 3 (3.6) |
| Amphotericin B lipid formulation | 32 (6.4) | 26 (6.3) | 6 (7.2) |
| Voriconazole | 43(8.7) | 34 (9.2) | 9 (10.8) |
| Fluconazole / echinocandins | 30(5.8) | 25 (5.6) | 5 (6.0) |
| other antifungals | 3(0.6) | 2 (0.5) | 1 (1.2) |
**Three cases of trichosporonosis, three mucormycosis, two curvaliosis, two pneumocystoses, one paracoccidioidomycosis, one histoplasmosis.
***Three patients in palliative care did not receive antifungal therapy.
IFI, Invasive Fungal Infection; IA, Invasive Aspergillosis; HSTC, Hematopoietic Stem Cell Transplantation; IRS, Invasive Rhinosinusitis; HRCT, High-Resolution Chest Tomography.
The IA hypothesis was done in 24.6 % (122/496) of patients included in this study and 73.5 % (122/166) of patients with IFI. IA was classified as proven in 7.8 % (13/122), probable in 16.1 % (80/122), and possible in 17.5 % (29/122) patients with IFI, and in 2.2 %, 16.1 % e 5.8 % among the 496 included patients, respectively (Table 3).
Other fungal infections were diagnosed in 42.7 % (50/496) patients and represented 30.1 % (50/166) of patients with IFI. Fusariosis was diagnosed in 4.0 % (20/496) of the included patients, representing 12.1 % (20/166) of the IFI. In addition, three cases of trichosporonosis, three mucormycoses, two curvaliosis, two pneumocystoses, one paracoccidioidomycosis, one histoplasmosis, and one cryptococcosis were diagnosed (Table 3).
IFI was treated with amphotericin B in 51.8 % (86/166) of patients, and 25.9 % (43/166) with voriconazole. Data on the use and antifungals used are described in Table 3.
Patients admitted to the oncohematology ward and the HSCT unit were similar in terms of clinical and epidemiological characteristics and occurrence of IFI, and different in relation to the length of hospital stay and mortality. In this way, they were grouped to analyze the factors associated with the positive GM test, the prescription of antifungal therapy, and in-hospital mortality.
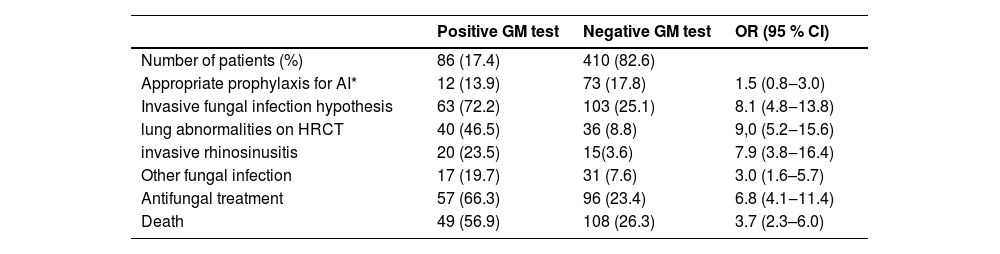
Negative GM test was more frequent among patients who did not receive adequate anti-mold prophylaxis, but it was not statistically significant (17.9 % and 13.9 %; OR = 1.5, 95 % CI 0.8–3.0) (Table 4).
Factors associated with positive GM test.
GM, Galactomannan; OR, Odds Ratio; CI, Confidence Interval; IA, Invasive Aspergillosis; HRCT, High-Resolution Chest tomography.
Positive GM test was more frequent in patients with a hypothesis of IFI (72.2 % and 25.1 %; OR = 8.1; 95 % CI 4.8 to 13.8); among patients with lung abnormalities on HRCT (46.5 % and 8.8 %; OR = 9.0, 95 % CI 5.2‒15.6); patients with IRS (23.5 % and 3.6 %; OR = 7.9, 95 % CI 3.8‒16.4), and among those who died (56.9 % and 26.3 %; 3.7 95 % CI 2.3‒6.0) (Table 4).
The variables associated with the use of therapeutic antifungal were mean days of neutropenia (17.5 + 12.2 and 10.6 + 9.2; p = 0.002), positive GM test (52.9 % and 20.5 %; OR = 4.3, 95 % CI 2.0‒9.4) and presence of lung abnormalities in HRCT (45.3% vs. 21.5 %; OR = 3.0, 95 % CI 1.4‒6.5).
In-hospital mortality occurred in 31.6 % (157/496) of patients. In the multivariate analysis by logistic regression, the risk factors identified for mortality were having IFI HD (OR = 6.35, 95 % CI 3.63‒11.12), positive GM test (OR = 2.7, 95 % CI 1.6‒4.5), and lung abnormalities in HRTC (OR = 2.6, 95 % CI 1.5‒4.4).
DiscussionAll patients in this cohort had a GM test during hospitalization and were diagnosed with hematologic neoplasia or underwent HSCT. They presented the epidemiological and clinical characteristics considered at high risk for IFI, highlighting the large number of patients with acute myeloid leukemia (41.3%) and patients with prolonged neutropenia associated with fever (70%).1-3,10
The GM test positive helped in the diagnosis of IA, being nine times more frequent among patients with altered HRCT findings (OR = 9.0; 95% CI 5.2 to 15.5) and about eight times more among those with IRS (OR = 7.9; 95% CI 3.8 to 16.4). As described in other studies, these data suggest a relationship between GM test positivity, degree of angioinvasion, or more advanced fungal disease.16,17
HRCT findings were mainly the presence of nodules and ground-glass infiltrate, confirming the importance of chest tomography in diagnosing IA.18 These findings, although not specific, are more frequent than classic findings such as the halo sign and the air crescent sign. They also present a good correlation with fungal infection and are included in the criteria of probable IA by EORTC.16-18
Jin J (2019) performed a post-hoc analysis of the HRCT findings of 395 patients with hematologic malignancy or allogeneic HSCT with suspected invasive aspergillosis and observed that ground-glass attenuation and pulmonary nodules were the changes most associated with subsequent confirmation of IA.17
The incidence of IFI in our study was higher when compared to other national and international studies.19-22 Aspergillosis occurred in 24.6% of the patients and 73.5% of those with a hypothesis of IFI. Kontoyiannis (2010), in his prospective study, identified 983 IFI among 875 patients undergoing HSCT, and Invasive aspergillosis (43%), invasive candidiasis (28%), and zygomycoses (8%) were the most common IFIs.22
Proven or probable IA was diagnosed in 31% of cases of filamentous fungal infections in the study conducted in Brazil by Garnica et al.13
In the present study, the frequency of IA was high. It may be related to the fact that most patients (76.8%) received prophylaxis with fluconazole because voriconazole was only available at the hospital in the final period of the study.
Another fact to be highlighted was the high frequency of invasive fusariosis, the second most diagnosed IFI, occurring in 4.0% of the patients, representing 12.1% of the IFI. A high incidence of invasive fusariosis has been reported in Brazilian studies.19-21 With the use of prophylactic voriconazole, the incidence of fusariosis has represented 10% to 25% of IFI among patients with hematological malignancies or submitted to HSCT.22-24
It is important to report that the rooms of the HSCT unit of this institution have air control through HEPA filters (High-Efficiency Particulate Arrestance) and positive pressure air flow, but this does not occur in the oncohematology ward, where the majority of patients (83.3 %) have cared. These environmental conditions may have increased the possibility of exposure to fungal conidia and higher rates of infections. Proven IA and invasive fusariosis were often among patients admitted to the oncohematology ward. The absence of HEPA in the rooms of patients at risk of IFI probably represents the reality of most Brazilian SUS hospitals that care for patients with hematological malignancies.
Invasive Pulmonary Aspergillosis (IPA) and IRS are frequent presentations of IA; this is expected if we consider the form of acquisition of the fungus, which lodges in the airways after inhaling.1,16 In the present study, 45.8% of patients with the IFI hypothesis had suggested findings of IA on HRCT.
The GM test was positive in 52.6% of patients with HRCT findings, rates similar to those described by other authors.14 Jung et al. (2018), evaluating the tomographic findings of adult patients with proven or probable infection, concluded that angioinvasion is more frequent in patients with positive GM.16
All individuals underwent GM tests, but only those with clinical IFI hypotheses had HRCT and sinus CT performed. These data are greater than other institutions with the same approach investigating IFI/IA, perhaps due to the lack of adequate infrastructure, such as HEPA filters, and the lack of access to the first-choice antifungals in the first period of study.25
Depending on the patient's clinical data or the findings on imaging exams, the patients received antifungal treatment before or after the result of the GM test; because it is performed on Tuesdays and Thursdays, the result may be available on the same day or within one to four days after collection.
Currently, at our institution, prophylactic VCZ is included in the protocol for assisting patients at high risk of IA. In this context, we believe the GM test should be performed after suspicion of IFI and no longer as a surveillance test among high-risk patients. With the prophylactic use of VCZ, the pretest probability of IA will decrease, and false positive results will increase, making the interpretation more difficult for the decision to prescribe antifungals.2,19,26
One hundred and fifty-six patients (31.4%) received antifungal treatment; Amphotericin B (AB) was the most frequently prescribed, mainly the AB deoxycholate. Here we also emphasize that, in the early years of the study, AB was often the only therapeutic option available at the hospital. Patients with a longer mean period of neutropenia, with a positive GM test, and with pulmonary involvement were more likely to receive antifungal treatment. Certainly, these data, interpreted together or sequentially, greatly increase the likelihood of IFI/IA and confidence in the introduction of antifungal treatment.27-29
The in-hospital mortality of patients with IFI/IA is high,2,30,31 and similar to what was observed in this study (31.7 %). It was higher among patients with the IFI hypothesis. A prospective Brazilian study that included eight centers and 192 patients found that 30-day survival was significantly lower in patients who developed IFI compared to patients without IFI (60.0% vs. 91.6 %, respectively, p < 0.001).19
In the present study, the hypothesis of IFI, the positive GM test, and altered lung alterations in HRCT, were independently associated with mortality in the multivariate analysis. These findings are described by other authors.14,26,27 One can understand that these patients may have a large fungal burden, with greater angioinvasion, resulting in greater lung involvement and greater severity of cases. In addition, pulmonary involvement may be associated with more systemic severe repercussions and clinical instabilities.7
Our study has some limitations related to its retrospective design, it included only patients from a single institution, and it did not analyze some variables, such as disease recurrence and transplant incompatibility, which are known to have an impact on prognosis. However, it has the advantage of including a large sample of patients, who probably have similar characteristics to those cared for in other Brazilian institutions, who do not have HEPA and positive pressure in their wards, nor the first-choice antifungals are available.
ConclusionPositive GM testing was associated with lung abnormalities on HRCT and with the introduction of therapeutic antifungals. If adequate anti-mold prophylaxis is available, the GM test should not be used as screening, but in the context of clinical suspicion of IFI in high-risk patients. The diagnosis of IFI, positive GM test, and lung abnormalities on HRCT are independent predictors of hospital mortality in patients with hematological malignancies or undergoing HSCT
Ethics approval statementThe local ethics committee (research ethics committee of University Hospital) approved the design of this study. CAAE: 24708019.0.0000.5404.
Consent for publicationAll authors approved the final version submitted.
Authors’ contributionsConception and design: Lucieni de Oliveira Conterno.
Analysis and interpretation of data: All.
Drafting of manuscript: Lucieni de Oliveira Conterno; Plinio Trabasso.
Supervision: Lucieni de Oliveira Conterno
This project was funded by process nº 2019/09594-7, Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) on behalf of Lucieni de Oliveira Conterno.