Ventilator-associated pneumonia (VAP) is the most significant nosocomial infection in patients in the intensive care unit (ICU) who have been on mechanical ventilation (MV) for over 48hours, and is related to higher morbidity and mortality of these patients (24% to 72%).1,2 During a prospective study, 813 patients were hospitalized in the ICU of the Clinical Center of Vojvodina, Novi Sad, Republic of Serbia. All patients were on MV for over 72hours. 40% of our patients were on MV for five to ten days. Dostanic et al.3 have obtained similar results. The mean duration of MV was 222.3hours. There were both male and female patients, and their mean age was 55 years. VAP was suspected in 115 patients. Microorganisms were isolated and identified in 82 patients. Of the total number of analyzed patients with suspected VAP, 29% had no bacteria, 28% had only one isolated bacteria, while the remaining 43% of patients had polymicrobial isolates.
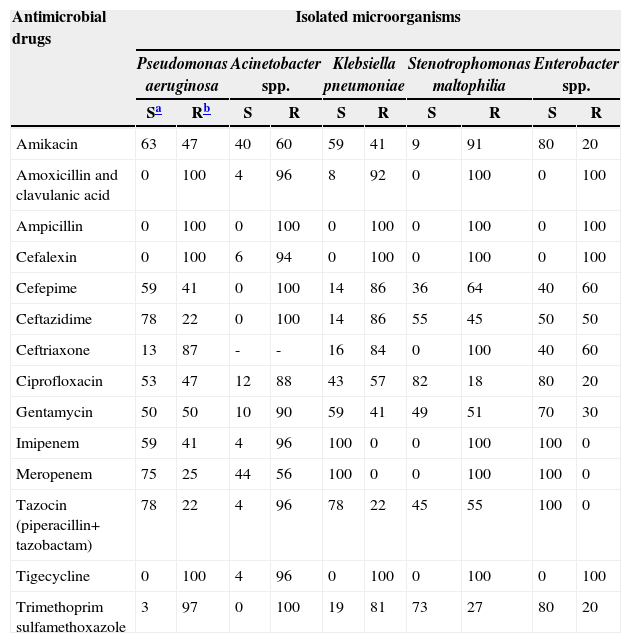
Testing bacterial sensitivity to antimicrobial drugs was performed using a standard disc diffusion method by Kirby-Bauer, according to the guidelines of the European Committee. All isolated microorganisms showed over 50% resistance for amoxicillin + clavulanic acid, ampicillin, cefalexin, ceftriaxone, and tigecyclin (Table 1).
Resistance of isolated microorganisms to the tested antimicrobial drugs.
| Antimicrobial drugs | Isolated microorganisms | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pseudomonas aeruginosa | Acinetobacter spp. | Klebsiella pneumoniae | Stenotrophomonas maltophilia | Enterobacter spp. | ||||||
| Sa | Rb | S | R | S | R | S | R | S | R | |
| Amikacin | 63 | 47 | 40 | 60 | 59 | 41 | 9 | 91 | 80 | 20 |
| Amoxicillin and clavulanic acid | 0 | 100 | 4 | 96 | 8 | 92 | 0 | 100 | 0 | 100 |
| Ampicillin | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 |
| Cefalexin | 0 | 100 | 6 | 94 | 0 | 100 | 0 | 100 | 0 | 100 |
| Cefepime | 59 | 41 | 0 | 100 | 14 | 86 | 36 | 64 | 40 | 60 |
| Ceftazidime | 78 | 22 | 0 | 100 | 14 | 86 | 55 | 45 | 50 | 50 |
| Ceftriaxone | 13 | 87 | - | - | 16 | 84 | 0 | 100 | 40 | 60 |
| Ciprofloxacin | 53 | 47 | 12 | 88 | 43 | 57 | 82 | 18 | 80 | 20 |
| Gentamycin | 50 | 50 | 10 | 90 | 59 | 41 | 49 | 51 | 70 | 30 |
| Imipenem | 59 | 41 | 4 | 96 | 100 | 0 | 0 | 100 | 100 | 0 |
| Meropenem | 75 | 25 | 44 | 56 | 100 | 0 | 0 | 100 | 100 | 0 |
| Tazocin (piperacillin+ tazobactam) | 78 | 22 | 4 | 96 | 78 | 22 | 45 | 55 | 100 | 0 |
| Tigecycline | 0 | 100 | 4 | 96 | 0 | 100 | 0 | 100 | 0 | 100 |
| Trimethoprim sulfamethoxazole | 3 | 97 | 0 | 100 | 19 | 81 | 73 | 27 | 80 | 20 |
Acinetobacter spp. was the most prevalent bacteria (65%) in respiratory secretion of patients on MV, and it presented multidrug-resistance in over 90% of cases. Results from this research showed identification of polymicrobial isolates in 43% of cases; 23% of cases presented two bacteria, 16% presented three bacteria, 3% presented four bacteria, and 1% presented five bacteria. Combes et al.,4 isolated two bacteria in 70% of cases; however, they found 16.7% of tribacterial cases, similarly to our findings.
In our research, Klebsiella pneumoniae was resistant to third-generation cephalosporins in over 80% of cases, while in a study from Poland the resistance rate ranged from 56% to 73%.5
The mortality rate was 68%, which is in agreement with the literature.1,2 Based on the data obtained, we can conclude that the incidence of VAP at the ICU was high.
Conflict of interestAll authors declare to have no conflict of interest.
This work was supported by the Ministry of Education, Science and Technological Development of the Republic of Serbia.