Chronic hepatitis C virus infection patients have higher rates of psychiatric disorders than the general population. Chronic hepatitis C virus infection is known to be associated with impaired health related quality of life. To our knowledge, there is no previous research of health related quality of life in chronic hepatitis C patients that combined structured psychiatric interview and careful psychopathological evaluation, including depression, anxiety and fatigue instruments. The aim of this study was to evaluate health related quality of life of chronic hepatitis C patients and to investigate the association with sociodemographic, psychopathological and psychiatric factors.
Materials and methodsEighty-one individuals with chronic hepatitis C virus infection receiving care at a Brazilian public university-based outpatient service for infectious diseases were enrolled in the study. The World Health Organization Quality of Life Scale Brief Version was used to assess health related quality of life. Standard psychiatric interview (Mini International Neuropsychiatric Interview-Plus) was conducted to establish Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Axis I psychiatric diagnosis. Further instruments completed psychopathological investigation: Beck Depression Inventory, Hospital Anxiety and Depression Scale, Brief Fatigue Inventory, Hamilton Depression Scale and Hamilton Anxiety Scale. Pearson Chi-Square and Kruskal–Wallis were performed for categorical and continuous univariate analysis, respectively. Correlation between psychopathological and health related quality of life scores was performed according to Spearman's correlation. Multivariate analysis was performed according to stepwise forward ordinal logistic regression. The significance threshold was fixed at α=0.05.
ResultsDepressive disorders were associated with worse scores in overall health related quality of life and in all domains. Fatigue was associated with lower scores in physical and psychological domains, and married status with higher scores in psychological health related quality of life. We found strong correlation among scores of depression, fatigue and health related quality of life.
ConclusionDepression and fatigue must be properly investigated and managed in HCV patients in order to improve HRQL. WHOQOL-BREF proved to be a useful instrument to assess HRQL in HCV patients.
Chronic hepatitis C virus (HCV) infection is a major health problem with around 160 million people infected worldwide.1 HCV leads to cirrhosis in up to 20% of those chronically infected and is the primary indication for liver transplantation.2 This burden is multiplied by the impact of HCV on health related quality of life (HRQL). Common complaints are fatigue, musculoskeletal pain, depression and perceived inability to function effectively.3,4 HCV itself may diminish HRQL even in the absence of advanced liver disease, perhaps as a result of extrahepatic symptoms related to HCV, cognitive dysfunction or psychosocial implications.5
Previous studies have implicated psychiatric disorders, especially depression, as contributing factor impairing quality of life of HCV patients.6 Nevertheless most studies on HRQL in HCV did not perform structured clinical interview in order to establish Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Axis I psychiatric diagnosis.3,6,7 Psychiatric disorders are more common in HCV patients than in the general population and may constitute a major cause of antiviral treatment interruption with negative impact on treatment response rates and prognosis.8 Fatigue and irritability are also common symptoms in HCV patients and may impair HRQL.9
There is scarce literature on the World Health Organization Quality of Life Scale Brief Version (WHOQOL-BREF) use in HCV patients.3 The WHOQOL-BREF is found to be a high quality patient-centered tool suited for individual assessment in clinical practice and research.10 One previous study showed good correlation among WHOQOL-BREF, Short Form-36 and Chronic Liver Disease Questionnaire in HCV patients.3 One recent work determined normative values for the WHOQOL-BREF in the Brazilian general population.11
The National Institutes of Health had recommended studies that measure not only traditional biological outcomes in HCV (i.e., HCV RNA, liver enzyme levels, liver histology), but also extrahepatic manifestations and patient-oriented outcomes.12 One recent review identified some gaps in the literature regarding assessment of symptoms and outcomes reported as important by HCV patients and also endorsed the importance of further research.13 The study of HRQL in HCV patients, including psychopathological and psychiatric thorough evaluation, is in line with these recommendations.
This study aimed to evaluate HRQL of a Brazilian sample of HCV patients and to investigate its association with sociodemographic, psychopathological and psychiatric factors using structured psychiatric interview and careful psychopathological investigation.
Materials and methodsStudy design, setting and participantsBetween May 2009 and November 2010, a cross sectional study with a convenience sample of HCV patients were performed at a public university-based outpatient service for infectious diseases (CTR-DIP Orestes Diniz-SMSA-BH/UFMG) in Belo Horizonte, Minas Gerais, Brazil. Approximately 400 HCV infected patients are currently under medical assistance at this service. All patients had more than 18 years of age and had anti-HCV antibody positive by third-generation enzyme-linked immunosorbent assay for more than six months and HCV RNA detectable by polymerase chain reaction (AMPLICOR, Roche Molecular Systems). Patients were excluded if they had any of the following: co-infection with hepatitis B virus or HIV, or low scores in the Mini Mental Status Examination14 suggestive of cognitive deficit.
ProceduresAll patients were assessed on the same day of routine clinical evaluation. Sociodemographic, clinical and laboratory data, including liver biopsy with Metavir score15 were obtained through chart review and patient interview. The presence of comorbid conditions was also assessed by chart review and categorized as hypertension, diabetes, or other. Cirrhosis was defined according to documented liver biopsy, ultrasound or decompensated liver disease, defined as a history of at least one of the following: ascites, jaundice, variceal bleeding, hepatic encephalopathy, hematemesis, palmar erythema, gynecomastia.
Psychiatric evaluation was conducted by an experienced psychiatrist who performed a structured clinical interview using the Mini International Neuropsychiatric Interview (M.I.N.I.-Plus version).16 This instrument allows a psychiatric diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and the International Classification of Diseases, 10th Revision Axis I diagnostic criteria.
HRQL was measured by the WHOQOL-BREF, a generic HRQL instrument designed by the World Health Organization for healthy people and patients, used as an outcome measure in many countries and cultures.10,17 It consists of 26 item self-administered questionnaire based on the preceding two weeks. WHOQOL-BREF interpretation considers four HRQL domains, namely, physical, psychological, social relationships and environment, besides overall health and quality of life perception. It has shown excellent psychometric and clinimetric properties, such as test–retest reliability, internal consistency, discriminant validity, and construct validity.18 This instrument had been previously translated into Portuguese and validated for use in the Brazilian population.19
Depressive symptoms were measured by three instruments: Beck Depression Inventory (BDI), Hospital Anxiety and Depression Rating Scale (HAD) and Hamilton Depression Rating Scale (HAM-D). BDI is a self-rating scale with 21 items, including somatic and non-somatic symptoms.20 It is the most used self-rating depression scale, both in the clinical practice and in research settings, and has proved to be the most efficient inventory to screen for depression in HCV patients.21
Anxiety was measured by the Hamilton Anxiety Rating Scale (HAM-A)22 and the Hospital Anxiety and Depression Rating Scale (HAD).23
Fatigue was assessed through the Brief Fatigue Inventory (BFI),24 a self-administered scale used to measure severity of fatigue. Average scores were categorized, according to authors’ recommendation, in mild (0–3 points), moderate (4–6 points), or severe fatigue (7–10 points). This instrument has proved to be useful in HCV patients, with concurrent validity when compared to other instruments such as the Fatigue Impact Scale.5 A complementary analysis of fatigue was performed through its specific item on the BDI (item 17). Irritability was investigated through another specific item of the BDI (item 11).
Statistical analysisHRQL results were analyzed by two distinct methods. In the first one, a standardized conversion of Likert scale data projected onto a 0–100 scale (to each domain and to overall health and quality of life perception). This method is commonly used in the literature and provides results comparable to other studies. Absolute scores were also useful in order to investigate correlation among HRQL, depressive and fatigue scores. A second method, used in the present study for all univariate and multivariate analysis, consists of transforming the 0–100 scale into an ordinal data according to interquartile ranges: 0–25, 25–50, 50–75, 75–100. This method has been previously studied for HRQL instruments and may be more appropriate to inferential process than statistical analyses that often use absolute scores with discrete, asymmetrical, and limited distributions.25
Pearson Chi-Square and Kruskal–Wallis were performed for categorical and continuous univariate analysis, respectively. Correlation between psychopathological and HRQL scores was performed according to Spearman's correlation. Multivariate analysis was performed according to stepwise forward ordinal logistic regression. The significance threshold was fixed at α=0.05. The power corresponding to sample size was calculated as the accumulated probability of the standard normal distribution of the next percentile. SPSS, version 20 (SPSS Inc., Chicago, IL) was used to conduct all the analysis.
Hypothesizing that subthreshold depression can impact negatively on HRQL, we made a careful investigation of depressive symptoms. Therefore, we made a ROC curve analysis of best cutoff value for BDI score capable of distinguishing the two lower percentiles in WHOQOL-BREF overall HRQL. We also performed a detailed analysis of BDI items in order to investigate if there were some items with stronger association to HRQL.
Ethical issuesThis study was previously approved by the Research Ethical Committee of the Federal University of Minas Gerais (number 560/08) and written informed consent was obtained from all subjects.
ResultsEighty-eight HCV patients were invited for an eligibility interview. Seven patients did not enter the study. Three of them refused to participate, and four had Mini Mental Status Examination suggestive of cognitive impairment. Finally, 81 patients were enrolled in the study. Comparing the 81 enrolled patients with the seven that did not enter the study, there was no significant statistical difference related to: gender (p=0.705), age (p=0.527), ethnicity (p=0.135), years of education (p=0.204), years since HCV diagnosis (p=0.264) and viral genotype (p=0.724). Married status or stable relationship was less common in non-enrolled patients (p=0.015), which also presented more inflammatory activity (p=0.038) and fibrosis (p<0.001) at liver biopsy.
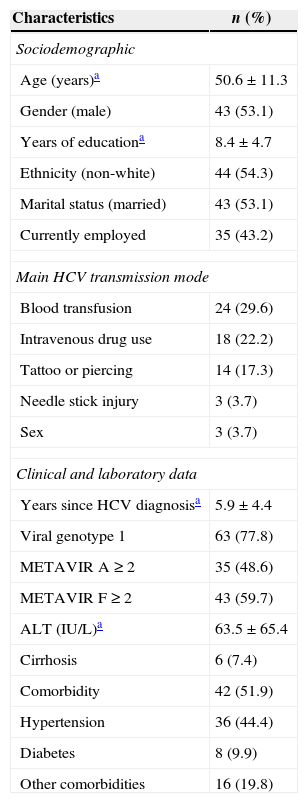
Sociodemographic, clinical features and laboratory data of the studied sample are presented in Table 1. There was a similar proportion of male and female, and the mean age was 43 years old. Non-white individuals were predominant (54.0%) and the mean education was eight years. About half of the subjects declared to be married and only 14% declared to live alone. Less than half of the patients (43.0%) were employed. Regarding interferon-alpha (IFN) use, 34 patients were never exposed to it (naïve) 17 patients were currently using pegylated IFN at standard doses, and 30 patients had been previously treated with IFN. The two main HCV transmission modes were blood transfusion (29.6%) and intravenous drug use (22.2%). The mean age since HCV diagnosis was 5.9 years, and viral genotype 1 was predominant (77.8%). Mean alanine aminotransferase was 63.5IU/L, and despite more than half of patients presenting significant hepatic fibrosis, according to METAVIR classification, only 7.4% had cirrhosis. Approximately half of patients had at least one clinical comorbidity, with hypertension being the most common.
Sociodemographic, clinical characteristics and laboratory data of 81 patients with chronic hepatitis C virus infection.
| Characteristics | n (%) |
|---|---|
| Sociodemographic | |
| Age (years)a | 50.6±11.3 |
| Gender (male) | 43 (53.1) |
| Years of educationa | 8.4±4.7 |
| Ethnicity (non-white) | 44 (54.3) |
| Marital status (married) | 43 (53.1) |
| Currently employed | 35 (43.2) |
| Main HCV transmission mode | |
| Blood transfusion | 24 (29.6) |
| Intravenous drug use | 18 (22.2) |
| Tattoo or piercing | 14 (17.3) |
| Needle stick injury | 3 (3.7) |
| Sex | 3 (3.7) |
| Clinical and laboratory data | |
| Years since HCV diagnosisa | 5.9±4.4 |
| Viral genotype 1 | 63 (77.8) |
| METAVIR A≥2 | 35 (48.6) |
| METAVIR F≥2 | 43 (59.7) |
| ALT (IU/L)a | 63.5±65.4 |
| Cirrhosis | 6 (7.4) |
| Comorbidity | 42 (51.9) |
| Hypertension | 36 (44.4) |
| Diabetes | 8 (9.9) |
| Other comorbidities | 16 (19.8) |
ALT, alanine aminotransferase.
According to DSM-IV criteria, 46 patients (56.8%) had current psychiatric disorder: 26 (32%) had depressive disorders, 18 (22.0%) anxiety disorders, 7 (9.0%) alcohol use disorders, and 7 (9.0%) illicit drug use disorders. Among depressive disorders, there were 23 patients with major depression and three with distimia. The most common anxiety disorders were specific phobia and generalized anxiety disorder, presented in nine and eight patients, respectively. Of note, 26 patients had depressive disorder diagnosis, but only nine of them were currently using any antidepressant. Furthermore, only 27 (58.7%) out of 46 patients diagnosed with psychiatric disorder had such condition registered in their medical chart.
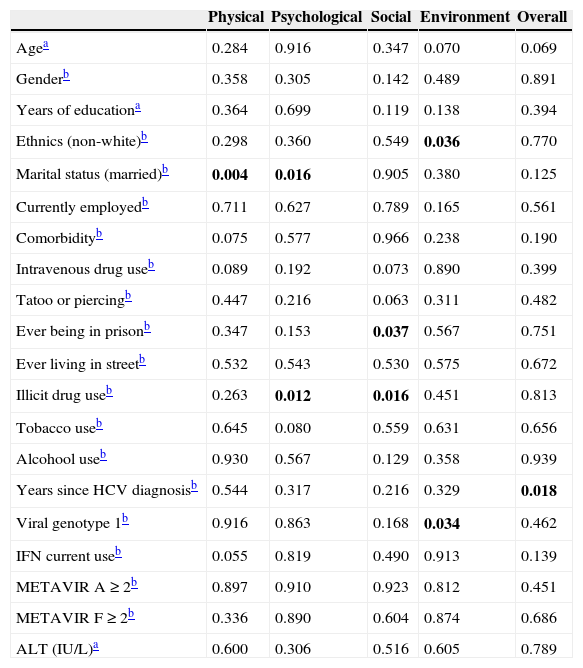
The median (range) HRQL scores were: 60.7 (17.9–100) on physical domain; 70.8 (8.3–95.8) on psychological domain; 58.3 (8.3–100) on social domain; 56.3 (12.5–96.9) on environment domain; 65.5 (0–100) on overall HRQL. In univariate analysis (Table 2), non-white subjects and viral genotype 1 were associated with lower environment HRQL. Married individuals, or with stable relationship, had higher scores both in physical and psychological domains. Previous history of incarceration was associated with lower scores in social domain. Previous or current illicit drug use was associated to lower scores in psychological and social domains. More years since diagnosis of HCV were associated to lower scores in overall HRQL. Viral genotype 1 was associated to lower scores in environment domain. Patients with physical comorbidity seemed to have lower scores on physical domain, compared to those without physical comorbidity, but this difference was not statistically significant (p=0.075).
Correlation between sociodemographic, epidemiological, clinical features and health related quality of life measures of 81 patients with chronic hepatitis C virus infection.
| Physical | Psychological | Social | Environment | Overall | |
|---|---|---|---|---|---|
| Agea | 0.284 | 0.916 | 0.347 | 0.070 | 0.069 |
| Genderb | 0.358 | 0.305 | 0.142 | 0.489 | 0.891 |
| Years of educationa | 0.364 | 0.699 | 0.119 | 0.138 | 0.394 |
| Ethnics (non-white)b | 0.298 | 0.360 | 0.549 | 0.036 | 0.770 |
| Marital status (married)b | 0.004 | 0.016 | 0.905 | 0.380 | 0.125 |
| Currently employedb | 0.711 | 0.627 | 0.789 | 0.165 | 0.561 |
| Comorbidityb | 0.075 | 0.577 | 0.966 | 0.238 | 0.190 |
| Intravenous drug useb | 0.089 | 0.192 | 0.073 | 0.890 | 0.399 |
| Tatoo or piercingb | 0.447 | 0.216 | 0.063 | 0.311 | 0.482 |
| Ever being in prisonb | 0.347 | 0.153 | 0.037 | 0.567 | 0.751 |
| Ever living in streetb | 0.532 | 0.543 | 0.530 | 0.575 | 0.672 |
| Illicit drug useb | 0.263 | 0.012 | 0.016 | 0.451 | 0.813 |
| Tobacco useb | 0.645 | 0.080 | 0.559 | 0.631 | 0.656 |
| Alcohool useb | 0.930 | 0.567 | 0.129 | 0.358 | 0.939 |
| Years since HCV diagnosisb | 0.544 | 0.317 | 0.216 | 0.329 | 0.018 |
| Viral genotype 1b | 0.916 | 0.863 | 0.168 | 0.034 | 0.462 |
| IFN current useb | 0.055 | 0.819 | 0.490 | 0.913 | 0.139 |
| METAVIR A≥2b | 0.897 | 0.910 | 0.923 | 0.812 | 0.451 |
| METAVIR F≥2b | 0.336 | 0.890 | 0.604 | 0.874 | 0.686 |
| ALT (IU/L)a | 0.600 | 0.306 | 0.516 | 0.605 | 0.789 |
IFN, interferon-alpha; ALT, alanine aminotransferase.
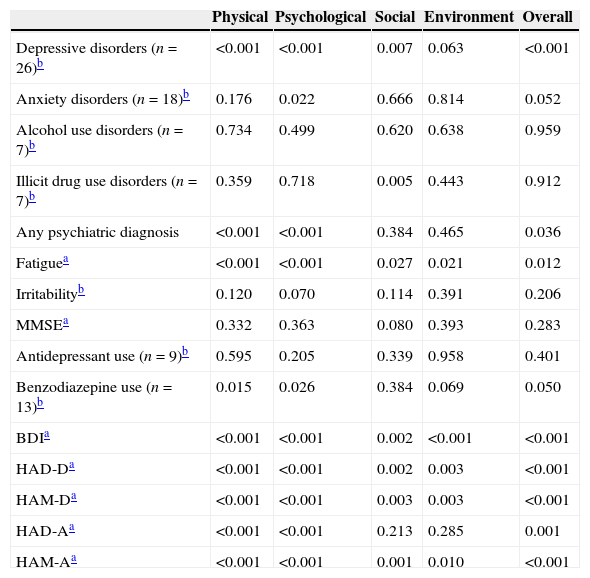
Correlation between psychopathological factors, psychiatric diagnosis and HRQL is presented in Table 3. We found strong correlation between depression scores, according to BDI, and HRQL scores, according to WHOQOL-BREF: physical (rho −0.593; p<0.001), psychological (rho −0.691; p<0.001), social (rho −0.401; p<0.001), environment (rho −0.489; p<0.001), overall (rho −0.588; p<0.001).
Correlation between psychopathological factors, psychiatric diagnosis and health related quality of life measures of 81 patients with chronic hepatitis C virus infection.
| Physical | Psychological | Social | Environment | Overall | |
|---|---|---|---|---|---|
| Depressive disorders (n=26)b | <0.001 | <0.001 | 0.007 | 0.063 | <0.001 |
| Anxiety disorders (n=18)b | 0.176 | 0.022 | 0.666 | 0.814 | 0.052 |
| Alcohol use disorders (n=7)b | 0.734 | 0.499 | 0.620 | 0.638 | 0.959 |
| Illicit drug use disorders (n=7)b | 0.359 | 0.718 | 0.005 | 0.443 | 0.912 |
| Any psychiatric diagnosis | <0.001 | <0.001 | 0.384 | 0.465 | 0.036 |
| Fatiguea | <0.001 | <0.001 | 0.027 | 0.021 | 0.012 |
| Irritabilityb | 0.120 | 0.070 | 0.114 | 0.391 | 0.206 |
| MMSEa | 0.332 | 0.363 | 0.080 | 0.393 | 0.283 |
| Antidepressant use (n=9)b | 0.595 | 0.205 | 0.339 | 0.958 | 0.401 |
| Benzodiazepine use (n=13)b | 0.015 | 0.026 | 0.384 | 0.069 | 0.050 |
| BDIa | <0.001 | <0.001 | 0.002 | <0.001 | <0.001 |
| HAD-Da | <0.001 | <0.001 | 0.002 | 0.003 | <0.001 |
| HAM-Da | <0.001 | <0.001 | 0.003 | 0.003 | <0.001 |
| HAD-Aa | <0.001 | <0.001 | 0.213 | 0.285 | 0.001 |
| HAM-Aa | <0.001 | <0.001 | 0.001 | 0.010 | <0.001 |
MMES, Mini Mental Status Examination; BDI, beck depression inventory; HAD-D, Hospital Anxiety and Depression Scale, depression subscale; HAM-D, Hamilton Depression Scale; HAD-A, Hospital Anxiety and Depression Scale, anxiety subscale; HAM-A, Hamilton Anxiety Scale.
According to BFI, fatigue was found to be mild in 34 patients (42.0%), moderate in 32 patients (39.5%) and severe in 15 patients (18.5%). We also found strong correlation between fatigue scores, according to BFI, and HRQL scores: physical (rho −0.644; p<0.001), psychological (rho −0.624; p<0.001), social (rho −0.336; p=0.002), environment (rho −0.322; p=0.003), overall (rho −0.422; p<0.001). Benzodiazepine current use (n=13) was associated with severe fatigue (p=0.043), and its use did not differ according to gender (p=0.249). A significant correlation between depression scores, according to BDI, and fatigue scores, according to BFI, was noticed (rho 0.646; p<0.001).
BDI analysis revealed some interesting data. Its individual item analysis showed that irritability (item 11) was one of the two most important items associated to lower HRQL scores on physical, psychological domains and on overall HRQL. BDI fatigue, according to item 17, was associated with poorer HRQL on physical (p=0.001), psychological (p=0.030) domain and overall HRQL (p=0.003) but neither with social (p=0.328) nor environment (p=0.207) domains. Best BDI cutoff score to predict worse overall HRQL was 16 points.
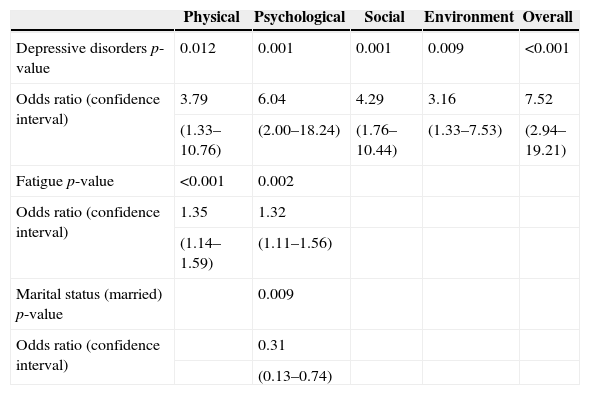
HRQL determinants, according to ordinal, stepwise, forward, multivariate analysis, are shown in Table 4. The power corresponding to sample size was calculated considering depressive disorders and overall HRQL: 1β=0.826; i.e., power=82.6%. It means 17.4% chance of type II error when considering association between depression and HRQL.
Health related quality of life determinants – ordinal, stepwise forward, multivariate analysis of 81 patients with chronic hepatitis C virus infection.
| Physical | Psychological | Social | Environment | Overall | |
|---|---|---|---|---|---|
| Depressive disorders p-value | 0.012 | 0.001 | 0.001 | 0.009 | <0.001 |
| Odds ratio (confidence interval) | 3.79 | 6.04 | 4.29 | 3.16 | 7.52 |
| (1.33–10.76) | (2.00–18.24) | (1.76–10.44) | (1.33–7.53) | (2.94–19.21) | |
| Fatigue p-value | <0.001 | 0.002 | |||
| Odds ratio (confidence interval) | 1.35 | 1.32 | |||
| (1.14–1.59) | (1.11–1.56) | ||||
| Marital status (married) p-value | 0.009 | ||||
| Odds ratio (confidence interval) | 0.31 | ||||
| (0.13–0.74) |
We found that depressive disorders, fatigue and non-married status were independently associated with poorer HRQL in HCV patients. To our knowledge this is the first study to assess HRQL in HCV patients using WHOQOL-BREF that combined psychiatric structured interview and careful psychopathological evaluation, including depression, anxiety and fatigue instruments.
One previous Brazilian HRQL study that performed psychiatric structured interview in HCV patients used SF-36 and had several exclusion criteria, such as IFN use, hypertension, diabetes and hypothyroidism, limiting its external validity.26 This study found lower frequency of mood (18.9%) and anxiety disorders (15.6%), possibly reflecting more stringent inclusion criteria.
Elevated frequency of depressive disorders in HCV patients found in our study is in accordance with the literature that reports higher rate than those found in other chronic infectious diseases like chronic hepatitis B.27 Furthermore, the literature shows that HRQL seems to be worse in HCV patients when compared to chronic hepatitis B patients.28 The high rate of unreported psychiatric diagnosis in charts and the low percentage of antidepressants use in the studied patients with depressive disorder highlight the need for improvement of psychiatric diagnosis and treatment in infectious disease reference centers. Another Brazilian study also found elevated frequency (84.6%) of unrecognized mental disorders in HCV patients followed at a university-based clinic.29 Our result endorses the importance of depression diagnosis and treatment among HCV patients.
More than half of the patients showed moderate to severe fatigue according to BFI, similar to chronic fatigue rates in HCV patients reported in other studies.30,31 One previous study with HCV–HIV co-infected patients showed that self-reported fatigue was associated with impairment in physical, psychological and social HRQL domains, and was a stronger predictor of worse HRQL than depression.6 Two previous studies, not specifically with HCV patients, evaluated temporal relations between fatigue and depression, and found that each one might act as independent risk factors for each other.32 The cross-sectional nature of our study did not allow for an explanation of causality between depression and fatigue, but endorses their relevance in predicting HRQL in HCV patients, notably in physical and psychological domains. Effective therapeutic interventions to reduce the burden of fatigue are desirable in this context.
Being married was associated with better HRQL, also shown in previous studies with HCV patients.6,33 One of these reports also found association between nonmarried status and impairment in social HRQL, but not in physical or psychological domains.6 Living alone did not interfere in HRQL scores. The low frequency of patients with advanced liver disease in our sample could explain, at least in part, the lack of influence of living alone on HRQL.
Gender did not interfere significantly in any HRQL domain, or overall HRQL, in contrast to previous studies that showed lower scores of HRQL in female individuals.26,34 Age also did not influence significantly HRQL. Age interference in HRQL of HCV patients is controversial, with some studies showing negative impact of age,34,35 while others no significant influence.31
Our studied sample showed similar scores of HRQL in physical, psychological and environment domains, but lower scores in social domain when compared to the Brazilian general population WHOQOL-BREF normative data. The underrepresentation of lower socioeconomic classes in normative data, with consequent higher scores of HRQL, could explain, at least in part, the difference in social domain scores.11
Our study had some clear limitations. Only 17 patients (21.0%) were using IFN during the study evaluation. This number may be too small in order to investigate IFN impact on HRQL. Economic aspects like monthly income, that could possibly have some influence on HRQL, were not investigated.
In conclusion, WHOQOL-BREF proved to be a useful instrument to assess HRQL in HCV Brazilian patients with good ability to distinguish patients with and without emotional distress or other unfavorable determinants. Depression and fatigue scales, as BDI and BFI, could also be used as basic easy-to-use measures of HCV patients’ well-being in clinical settings. The proper diagnosis and management of depression and fatigue in HCV patients could improve health assistance and warrant better patient-oriented outcomes, including HRQL. Future longitudinal studies with larger samples may be useful to better define the issue of causality or reverse causality between depression and fatigue in HCV patients, moreover to determine whether therapeutic strategies for these clinical problems can mitigate the associated HRQL burden.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank Dr. Mery Natali Silva Abreu for her careful assistance in statistical analysis. This study was partially funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Fapemig).