Exposure to Pneumocystis jirovecii (P. jirovecii) can lead to a wide variety of presenting features ranging from colonization in immunocompetent patients with lung disease, to invasive infections in immunocompromised hosts. Colonization by this fungus in patients with chronic obstructive pulmonary disease (COPD) could be associated with higher rates of exacerbations and impaired lung function in these patients.
Our objective was to determine whether colonization by P. jirovecii in patients with COPD is associated with increased exacerbations and deterioration of lung function.
This was a prospective cohort study on patients with COPD. All participants meeting selection criteria underwent clinical and microbiological assessments and were then classified as colonized vs. non-colonized patients. Chi-squared tests were performed and multivariate logistic models were fitted in order to obtain risk ratios (RR) with 95% confidence intervals (CI).
We documented a frequency of colonization by P. jirovecii of 32.3%. Most patients were categorized as having GOLD B and D COPD. The history of significant exacerbations in the last year, health status impairment (COPD Assesment Tool ≥10), airflow limitation (percent of post-bronchodilator FEV1), and BODEx score (≥5) were similar between groups. After a 52-week follow-up period, the rate of adjusted significant exacerbations did not differ between groups. However, a decrease in FEVI was found in both groups.
The etiological role of Pneumocystis jirovecii (P. jirovecii) as an opportunistic infectious agent is well known, and frequently leads to pneumonia in human inmmunodeficiency virus (HIV) infected patients, as well as in other conditions associated with immunosuppression. However, colonization by P. jirovecii (defined as the detection of the fungus without symptoms or signs suggestive of pneumonia) has been detected from young ages with reported seroprevalences up to 73%.1 The main difference regarding colonized patients, who unlike those with clinical infection, is a low microbial load.2 Colonization has been reported in up to 20% of immunecompetent patients through the analysis of bronchoalveolar lavage (BAL) samples and oropharyngeal washes through nested polymerase chain reaction (PCR).3,4
Furthermore, certain pathological conditions facilitate colonization, including immunosuppression by HIV, transplantation, malignancy, autoimmune diseases, immunosuppressive drugs, and pregnancy.2 The presence of chronic lung diseases has also been associated with predisposition for colonization. The aim of the present study was to evaluate the rate of colonization and the implications in the course of disease in a cohort of patients with COPD in Bogotá, Colombia.
Material and methodsRecruitmentWe conducted a prospective multicenter cohort study. Recruitment took place in two separate pulmonology units in the city of Bogota, in Colombia, from May 2015 to October 2017 through convenience sampling. Patients aged 40 years or more at the time the study was carried out and past medical histories remarkable for COPD were included in the study. All patients who entered the study freely signed an Informed Consent form. The Ethics and Research Committee of both institutions approved the study protocol. All processes in the study complied with the ethical principles defined in the Declaration of Helsinki.
Definition of the dependent variableThe dependent variable was defined as the presence or absence of colonization by P. jirovecii. We assessed the presence of colonization through the isolation of the fungus in induced sputum samples obtained after nebulization with hypertonic saline solution. If a non-representative sample was obtained, this procedure was repeated 48 h after the first attempt, in accordance with the European Respiratory Society parameters.5,6
Induced sputum samples were treated with a mucolytic solution composed of 4% sodium hydroxide, 3% trisodium citrate and N-acetyl-L-cysteine by centrifugation at 3000 rpm. Later, a phosphate buffer solution prepared with disodium phosphate and monopotassium phosphate was added to prevent pH changes and to simultaneously dilute and neutralize toxic substances.
DNA extraction was carried out with the commercial High Pure PCR Template Preparation (Roche®-Switzerland) following the manufacturer`s recommendations. The eluted product was quantified using the Eppendort BioSpectrometer ®. Real-time PCR (rt-PCR) was performed with the LightMix® Assay for P. jirovecii (Roche). A 244 base pair (bp) fragment from the surface glycoprotein gene of P. jirovecii was amplified through rt-PCR, by a pair of primers labeled with the Red 640 probe that is detected in the 640λ channel. The rt-PCR reaction had an internal control of a 278 bp fragment, consisting of a hybridization probe labeled with the Red 690 probe that is detected on the 705λ channel. The amplification process was performed on the LightCycler® 2.0 (Roche) under the following conditions: denaturation at 95 °C for 10 min, amplification by 50 cycles (95 °C for 5 s, 62 °C for 5 s and 72 °C for 15 s) and a cooling step at 40 °C for 30 s.
Definition of independent variablesCOPD was defined in accordance with the GOLD (Global Initiative for COPD) 2014 as any patient with dyspnea, chronic cough or sputum production, with a history of exposure to risk factors for the disease and the presence of persistent airflow limitation defined through a post-bronchodilator forced expiratory volume in one second to forced vital capacity ratio (FEV1/ FVC) <0.7.7 Patients with HIV-infection, solid organ or bone marrow transplants, autoimmune diseases, and malignant neoplasms who were receiving chemotherapy were excluded from the study. Likewise, patients with any disease or condition that required immunosuppressive treatments (methotrexate, cyclosporine, azathioprine, biological therapy or prednisolone with a daily dose regimen of at least 15 mg during the previous month) were not included.
Other studied variables included: sex, age, exposure to cigarette and/or wood smoke, comorbidities, exacerbations during the previous year, severity and classification of COPD, Body Mass Index (BMI), classification of dyspnea by the Modified Medical Research Council (mMRC) Dyspnea Scale,8 COPD Assessment Test (CAT)9 and post-bronchodilator FEV1 (percentage of the predicted value) and treatment.
Data collectionAll patients who met the previously described criteria were followed up for 52 weeks. Pre- and post-bronchodilator volume flow curves were assessed through the use of a MasterScreen Body (Jaeger) plethysmograph, in all participants on the first visit (day 0). The latter was performed according to the standards of the American Thoracic Society under the characteristics of validation and quality control as depicted by GOLD 2014 guidelines.7 Also, the BODEx index10 and the COPD Assessment Test (CAT) were applied and scores were calculated for each participant.
After the initial assessment, follow-up appointments were carried out every 180 days. In the second visit (day 180 of follow-up), in addition to the medical assessment and application of the CAT, information was collected regarding exacerbations and their respective classification. Significant exacerbations were defined as ≥ 1 severe exacerbation and/or ≥2 moderate exacerbations. On the third visit (day 360 of follow-up), in addition to the previous procedures, pre- and post-bronchodilator volume flow curves were performed in order to assess lung function and document any changes from baseline. In addition, telephone follow-up was performed every two months between face-to-face appointments, for the assessment of vital status, health status, and possible exacerbations.
Statistical analysisVariables categorized into dichotomous variables are presented using frequencies and percentages. Comparison of among these variables was performed through Chi-squared test. In addition, multivariate regression models (before and after adjustment) were employed for assessing association between the dependent and independent variables.
Risk ratios (RR) with 95% confidence intervals (CI) were obtained and are presented after adjustment for confounding variables (GOLD classification and treatment usage) in Fig. 1. The statistical level of significance was set at p < 0.05. Data was analyzed with the statistical software STATA 14®.
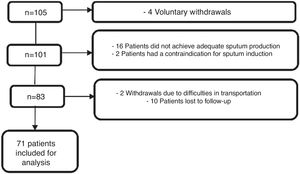
ResultsOne hundred and five patients were continuously recruited over a 29-month period. A total of 24 patients who signed the informed consent, voluntarily withdrew from the study. Of these, four patients left the study before data collection was completed, 16 participants did not achieve adequate sputum production, two patients had an exacerbation at the time of sputum collection and thus induction was contraindicated, two patients withdrew due to difficulties in transportation to the institution, and 10 participants were lost to follow-up. As a result, 71 patients were included for analysis as depicted in Fig. 1.
We documented a frequency of colonization by P. jirovecii of 32.3% (23 patients), of whom 65% were male, mean age 72 years. The mean time since diagnosis of COPD was eight years in colonized patients, and 10 years among non-colonized patients.
Most patients were categorized as having GOLD B and D COPD. In the group of colonized participants, 52% were classified as GOLD D, while 46% of non-colonized were categorized as GOLD B, suggesting that colonized patients had more severe disease, although not significantly different (p = 0.269). Regarding risk factors for COPD, 60% of colonized patients had been exposed to biomass for at least five years and 65% had a past medical history remarkable for tobacco smoking over five pack-years. Colonized patients more often had gastroesophageal reflux (34.7%) and cardiovascular disease (34.7%), while lower rates of depression (13%) and osteoporosis (8.7%) were found. These findings did not differ significantly from non-colonized participants. The history of significant exacerbations in the last year, health status impairment (COPD Assessment Tool ≥10), airflow limitation (percent of post-bronchodilator FEV1) and BODEx score (≥5) was of 43%, 96%, 57%, 24% in colonized patients and 35%, 87%, 64%, 18% in non-colonized patients, respectively, with no significant differences between groups (p = 0.513, p = 0.270, p = 0.241, p = 0.839, respectively). In addition, there were no significant differences in the use of control medication or oxygen therapy between groups either. Further characterization of the sample can be found in Table 1.
Clinical characteristics of patients with COPD according to colonization status.
| P. jirovecii colonization status | Positive (n = 23) | Negative (n = 48) | p-Value | |
|---|---|---|---|---|
| Biomass exposure >5 years | 14 (60.8%) | 35 (72.9%) | 0.304 | |
| Tobacco smoking ≥5 pack years | 15 (65.2%) | 27 (56.25%) | 0.472 | |
| Comorbidities | Depression | 3 (13%) | 12 (25%) | 0.248 |
| Osteoporosis | 2 (8.7%) | 7 (14.58%) | 0.485 | |
| Cardiovascular disease | 8 (34.78%) | 13 (27.08%) | 0.506 | |
| Gastroesophageal reflux | 8 (34.78%) | 12 (25%) | 0.391 | |
| Diabetes Mellitus | 4 (17.39%) | 8 (16.67%) | 0.939 | |
| Significant exacerbations in the last year | 10 (43.48%) | 17 (35.42%) | 0.513 | |
| mMRC ≥ 2 | 18 (78.26%) | 42 (87.5%) | 0.442 | |
| CAT ≥10 | 22 (95.65%) | 41 (87.23%) | 0.27 | |
| %FEV1 | 57.3 (20.7) | 64.7 (24.7) | 0.241 | |
| GOLD classification | B | 8 (34.78%) | 21 (45.65%) | 0.269 |
| D | 12 (52.17%) | 15 (32.61%) | ||
| BODEx ≥5 | 5 (23.81 %) | 8 (17.78%) | 0.839 | |
| Inhaled corticosteroids | 18 (78.26%) | 34 (70.83%) | 0.508 | |
| Long acting anticholinergics | 13 (56.52%) | 26 (54.17%) | 0.852 | |
| Long acting Beta2-agonists | 13 (56.52%) | 25 (52%) | 0.726 | |
| Oxygen therapy | 19 (82.6%) | 38 (79.2%) | 0.733 | |
P. jirovecii, Pneumocystis jirovecii.
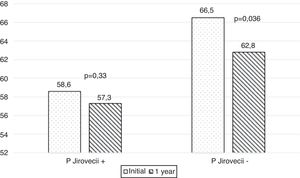
After a 52-week follow-up period, the rate of adjusted significant exacerbations did not differ between groups (p = 0.444). Furthermore, a decrease in FEVI was found in both groups, but was not significantly different between the two groups (Fig. 2).
DiscussionCOPD is characterized by decreased airflow, which can persist, and is usually progressive and not fully reversible. Acute exacerbations of COPD consist in a sudden worsening of symptoms, where bacterial colonization is one of the major etiologies.11–13 Nonetheless, the growing relevance of viruses and fungi in COPD is just beginning to be appreciated and studied.14–17 Colonization by P. jirovecii can be detected in healthy volunteers, but may be predisposed by certain conditions, such as immunosuppression due to HIV, transplantation, malignancy, autoimmune diseases, immunosuppressive drugs, and pregnancy.2
Also, mild immunosuppression, such as chronic lung diseases has been associated with predisposition for colonization.18,19 Colonization by P. jirovecii detected with molecular methods in patients with different lung diseases occurs in more than 21%; of these, 40% had chronic obstructive pulmonary disease (COPD), 20% had lung cancer, and 7% had cystic fibrosis18 Also, prevalence of up to 34% have been detected in patients with diffuse interstitial lung disease (ILD).20 The reported prevalence of colonization by this fungus in patients with COPD ranges from 10% to 65%. Our study detected a colonization rate of 32.3%, similar to previous findings of studies using similar molecular techniques. Thus, we consider that the differences on reported prevalence rates could be attributable to the techniques used to evaluate colonization, since molecular methods have proven to be much more sensitive than staining methods.3,182121–29
Furthermore, it has been determined that HIV-infected patients colonized by P. jirovecii have an eight-fold greater risk of airway obstruction when compared to non-colonized patients, even after adjusting for smoking history.24 In addition, P. jirovecii colonization has been associated with the severity of COPD in HIV-negative patients, even after adjusting for smoking history and immunosuppression. Recent reports stated that 37% of patients with severe COPD and only 5% of those with mild disease were colonized, in contrast to 9% of patients with other lung diseases,22 confirming not only the higher prevalence of colonization in patients with COPD unlike other pulmonary diseases, but also the association of such colonization with the severity of disease. Results from our study suggest that patients with COPD who were colonized with P. jirovecii had more severe disease, higher symptom burden and decreased lung function, as disclosed in previous reports. However, statistical significance was not reached.
It could be assumed that the high prevalence of detection of this fungus in patients without pneumonia is a finding associated with structural disease, immunosuppression by corticosteroids, or exposure to cigarette smoke. However, our study found no significant differences in medication use or risk exposures when comparing colonized and non-colonized patients.
Studies in animal models have suggested an association between colonization and deterioration of lung function detected through plethysmography and computed tomography.30 In humans, colonization by P. jirovecii has been associated with a systemic inflammatory response25 and locally enhanced Th1 activity.31,32 This is in accordance with recent studies of the lung microbiome that have led to important discoveries on changes in microbial composition that could potentially affect disease development and progression in COPD.23,33 The so-called vicious circle hypothesis, proposes that inhalation insults impair the innate immune defense system which leads to changes in abundance, taxonomic composition, and phylogenetic diversity of the lung microbiome. This leads to maladaptive inflammatory responses which generates further impairment of lung defense mechanisms and altered lung microbiome, setting up the vicious circle.34 Despite this theory,35 our study did not reveal significant differences between colonized and non-colonized patients in exacerbations or spirometry values after a 52-week follow-up period.
Our study has some strengths. To the best of our knowledge, this is the first study to assess the frequency of colonization by P. jirovecii in patients with COPD in Colombia and the first to assess outcomes in immunocompetent patients colonized by this fungus in Latin America. In addition, our study used induced sputum as the respiratory sample for molecular analysis. This non-invasive technique is known to produce reliable results. Furthermore, it compares favorably to bronchoalveolar lavage fluid for the diagnosis of infectious diseases36 and as a measure of airway inflammation in asthma, COPD and interstitial pulmonary disease.37 In addition, this is a widely available approach, which also carries less risk as compared to other invasive techniques, while maintaining diagnostic power.
However, some limitations must also be disclosed. The lack of statistically significant results may be attributed to a limited sample size, which in part was due to limitations to obtain adequate respiratory samples, because the requirements for sputum induction were not fulfilled by a significant number of patients. It is important to highlight that colonization by P. jirovecii does not seem to be permanent. A study in healthy people found that 20% were initially colonized and it persisted only in a minority of them after six months.4 Another study in newborns and their mothers found that P. jirovecii colonization varies over time, going from positive to negative and vice versa during the follow up.38 Regarding patients with lung diseases, there is a study in patients with cystic fibrosis that showed a continuous colonization/clearance cycle by different genotypes of the fungus.39 Unfortunately, this information is not available for COPD patients. These findings add complexity to data interpretation and raise the question if colonization is indeed a risk factor for COPD progression and how long it takes for it to be significant. In this study we did not perform follow up PCR which may be a limitation for interpretating the results.
ConclusionsFurther studies must confirm the lack of association between colonization by P. jirovecii and outcomes in immunocompetent patients living with COPD in order to improve care in this group of patients.
Funding detailsThis work was supported by the Hospital Universitario San Ignacio and the Pontificia Universidad Javeriana; Colombia under Grant ID 6339. The funding source had no involvement in the collection, analysis or interpretation of data nor in the writing and submission of the manuscript.
Conflicts of InterestThe authors declare no conflicts of interest.
Data availability statementThe datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
This study was reviewed and approved by the Institutional Research Boards at both Hospital Universitario San Ignacio and Pontificia Universidad Javeriana with the approval Code 2014/81. All patients signed an informed consent form. The privacy rights of human subjects was always observed. All processes in the study comply with the ethical principles defined in the Declaration of Helsinki and are in line with the recommendations for the conduct, reporting, editing and publication of scholarly work in medical journals.