The aim of this study was to evaluate the effect of the work environment and expertise/specialty degree of dentists on their behavior, awareness, and attitudes regarding cross-infection control during the COVID-19 pandemic.
DesignThe study population consisted of Turkish dentists who work in private clinics, public clinics and university hospitals. The demographic information of the participants, their awareness of the COVID-19 acute respiratory disease, and clinical measures taken against cross-infection were evaluated with an online survey. Between the 10th and 20th of November 2020, 2,400 surveys were e-mailed to dentists.
ResultsA total 454 professionals answered the survey. According to the results, 29.3% of the participants performed only urgent care during the pandemic period, whereas 59.9% of them performed both urgent and routine treatments. Among the responding dentists, 90.6% stated that they were worried about aerosol-generating dental procedures, but there was no differences between genders (p = 0.119). Most participants, especially specialists (p = 0.160) , applied strict cross-infection control methods during the COVID-19 pandemic (77.2%). These dentists used personal protective equipment (PPE) at rates that varied between 75.5% and 98.4%. Nonetheless, the rate of PPE use was different between genders and degrees of expertise: women used PPE more frequently than men (p = 0.025), and specialists used PPE more often than the other dentists (p = 0.04). Finally, there was a weak positive correlation between the level of PPE use and expertise (r = 0.121; p = 0.010).
ConclusionsDespite the overall knowledge of the participants regarding COVID-19 symptoms, transmission routes, and the guidelines needed to prevent the virus from spreading, the dental specialists followed infection control methods more strictly. Even though the participants were concerned about dental practices that create microbial aerosols during the pandemic period, they continued their clinical routines using high PPE levels and taking extra clinical precautions to avoid cross-infection.
In late December 2019, several patients with viral pneumonia were epidemiologically associated with a seafood market in Wuhan, China. The identified coronavirus that caused the infections was designated as “2019 novel coronavirus” ( COVID-19) using next-generation sequencing.1,2 The infection by COVID-19, confirmed by droplet transmission and human-to-human transmission, is a significant public health problem, with 88 million reported infection cases and over 1.9 million deaths globally.3,4 COVID-19 uses the angiotensin-converting enzyme II (ACE2), which is an enzyme and a cell entry receptor to invade the host cells. The typical clinical symptoms of infected patients are fever, dry cough, dyspnea, headache, and pneumonia. The progression of the disease may result in respiratory failure, pneumonia, alveolar damage, and even death.5
A.erosols are suspensions of liquid or solid particles containing all kinds of microorganisms and are responsible for the airborne transmission of microorganisms.6,7 Aerosols consist of small particles called droplet nuclei (1–5 μm) or droplets (> 5 μm). . Aerosols can contaminate surfaces in a range of one meter and form form a potential route of infection route in the lungs because [.1] they can penetrate the alveoli.7,8
Cross contamination is the spread of pathogens from one source to another through direct contact from patient-to-patient contact, patient-to-clinical staff contact by droplet transmission. The conjunctival, nasal, or oral mucosa from infected people produces droplets and aerosols containing microorganisms.8,9 Dentists are at high risk of cross-contamination due to frequent direct or indirect contact with dental instruments and surfaces contaminated with aerosols, blood, and saliva.10 Aerosols containing microorganisms in the oral cavity are created when high-speed handpieces and air/water sprays are used in dental procedures. Aerosols11,12 emitted into the air from high-speed handpieces used during caries removal or composite resin polishing increase the cross-contamination risk for dentists. Tooth preparation, removal of old fillings, debonding or removal of orthodontic composite remnants, scaling with a cavitron, and oral prophylaxis are procedures that carry a cross-contamination risk.11,13 However, the infectious character of aerosols produced in dental procedures depends on virulence dose, pathogenicity of the microorganism, and contaminated contents of the patient, such as plaque, blood, calculus, and saliva.14,15
According to the American Dental Association (ADA), the practice of the dental profession during the COVID-19 pandemic poses a unique challenge due to the high amount of aerosols and droplets produced, which are inevitable during routine dental procedures.16 Therefore, eeffective infection control strategies are needed to prevent the spread of COVID-19 during dental procedures.9 For this purpose, the American Centers for Disease Control and Prevention (CDC) recommends the performance of additional infection prevention, control procedures during the COVID-19 pandemic. Such extra clinical precautions, which should be applied to all patients and not only to those with suspected or confirmed COVID-19 cases, can prevent the spread of microbial aerosols and the contamination of dental equipment and materials.17,18
The aim of this study was to evaluate the effect of the work environment and expertise/specialty degree of dentists on their behavior, awareness, and attitudes regarding cross-infection control during the COVID-19 pandemic.
MethodsSample size The study population consisted of Turkish dentists who work in private and public clinics and university hospitals. The sample size required for the study was calculated based on the total number of dentists (34,045) in Turkey. With a 95% confidence interval, the power analysis estimated that 384 or more people should be involved . The Ethics Committee of the Istanbul Gelisim University approved the study protocol (ethical approval number: 2020/29).
Survey instrument The study questionnaire consisted of two parts and contained 20 closed-ended questions. The first part of the questionnaire aimed to learn the demographic characteristics of the participants (i.e., sex, age, work experience, workplace profile). The second part of the questionnaire aimed to evaluate the awareness of the participants about COVID-19 and clinical precautions against cross-infection based on the “COVID-19 infection control guidelines” published by the CDC.17 Experts previously examined the content adequacy of the questionnaire to evaluate the construct validity of the questions. As a first pilot evaluation, questions were sent to five specialists (two pediatric dentists, a restorative dentistry specialist, a statistician, and a general dentist). The questionnaire was revised according to the suggestions made by the experts. Two experts (a pediatric dentist and a restorative dentistry specialist) retested the questionnaire to check whether they were consistent with semantics and conceptual framework. After a language suitability review by a Turkish language expert, the questionnaire was created with Google Documents. . The e-mail announced that participation was voluntary and that the personal data would remain confidential. The study was designed and implemented under the Helsinki Declaration.
Statisticalanalysis Survey results were evaluated with descriptive statistics such as the number and percentage. The data were analyzed using IBM ® SPSS ® (version 24.0;IBM,Chicago,IL,USA). Mean, standard deviation, range, and frequency for variables were calculated. Pearson chi-square analysis was used for the crosstab of variables; the Spearman's rank correlation test was used to evaluate correlation between gender, specialty, and attitudes of the dentists towards cross infection. A p-value <0.05 was considered statistically significant.
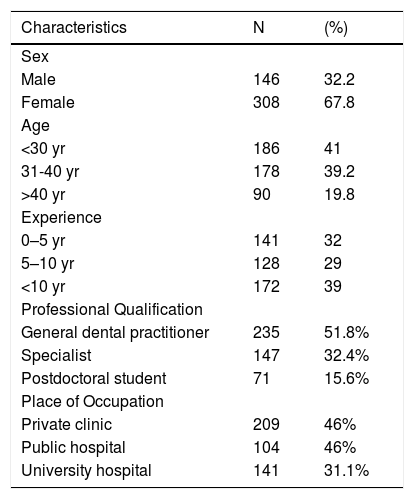
ResultsBetween November 10th and 20th, 2020, 2,400 questionnaires were e-mailed to the dentists, and 454 of them returned their responses, indicating a response rate of 18.9%. The demographic data revealed that 41% of the study population were aged < 30 years, 39.2% were aged between 31–40 years, and 19.8% had > 40 years. A total of 67.8% of the participants were female (Table 1).
Description of the demographic and professional characteristics of participants.
In terms of professional experience, 33.5% of the participants had >10 years, 33.5% had 5-10 years, and 33% had <5 years of experience. A large proportion of participants (51.8%) were general dentists, followed by dental specialists (32.4%) and post-graduate students (15.6%).A total of 46% of the respondents worked in private clinics, 22.9% in public clinics, and 31.1% in university hospitals (Table 1).
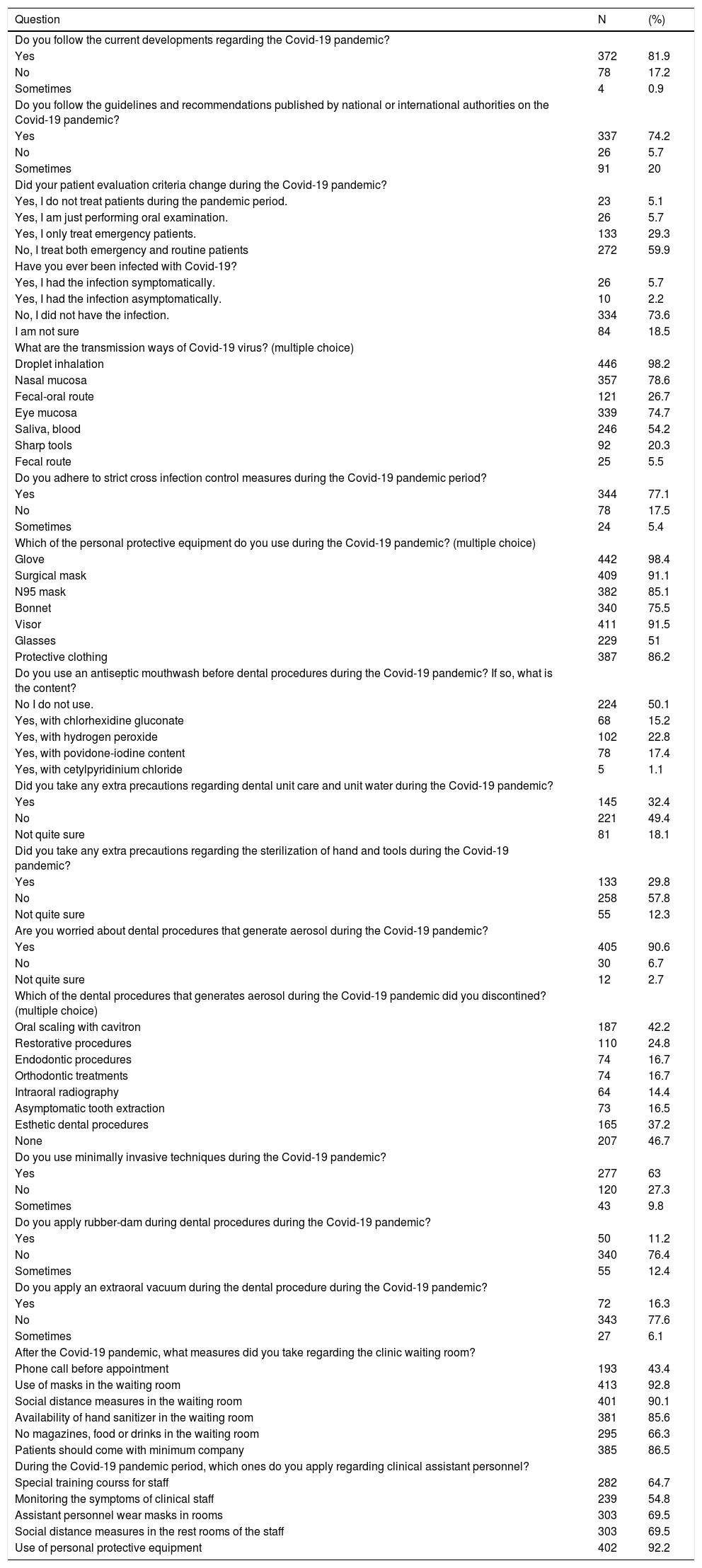
Of all the respondents, 81.9% indicated that they followed the current developments regarding COVID-19, and 74.2% of the participants followed the guidelines and recommendations published by national or international authorities regarding the COVID-19 pandemic (Table 2). there was no statistically significant difference between the responses given by men and women (pp=0.374, p=0.974, respectively) or between specialist and other dentists (p=0.061, p=0.137, respectively). Around 5.7% of the participants had symptomatic COVID-19 infection, 2.2% experienced a non-symptomatic infection, 73.5% did not have the disease, and the remaining participants indicated that they were not sure whether they had it or not. (Table 2).
Dentists' awareness of the COVID-19 pandemic and their answers about cross infection control measures.
Most respondents knew that droplet inhalation (98.2%), nasal mucosa (78.6%), fecal-oral route (26.7%), eye mucosa (74.7%), saliva/blood (54.2%), and contaminated sharp instruments (20.3%) were COVID-19 transmission routes. The knowledge level of specialist dentists about the COVID-19 transmission routes was higher than others (p=0.012). There was no statistically significant difference between the answers provided by female/male participants regarding their knowledge of COVID-19 transmission routes t (p=0.258).
Only 5.1% of the participants stated that they did not perform dental peocedures during the pandemic , whereas 5.7% stated that they only performed oral examinations . Also, 29.3% of the professionals mentioned that they only performed urgent procedures. Most respondents (77.2%) followed strict cross-infection control methods, and no statistically significant difference among genders (p = 0.261) was observed regarding the cross-infection control methods . On the other hand, specialists performed cross-infection controls more strictly than the others did (p = 0.16).
Personal protective equipment (PPE) usage rates varied from 75.5% to 98.4% among the participants. The rate of PPE usage was higher in females than in their male counterparts (p=0.025) andspecialists compared to other dentists (p=0.04). There was a weak positive correlation between the frequency of PPE use and expertise of the professionals (r=0.121, p=0.01). Among the respondents, 90.6% stated that they were worried about aerosol-generating dental procedures, and no statistical difference between genders was detected (p=0.119). A total of 46.7% of the participants reported that they did not suspend any dental procedures. Of these,11.3% used rubber-dam and 16.3% used an oral aerosol vacuum during dental procedures to prevent COVID-19 infections. Still, this difference was not statistically significant between genders (p=0.235) . The use rate of rubber-dam use by general dentists was statistically higher than of the other professionals (p=0.005) . Still there was no difference between participants in terms of using oral aerosol vacuum. About half of the respondents (49.9%) reported performing antiseptic mouthwashes on patients before the dental procedure. The use of hydrogen peroxide mouthwash by specialists was significantly higher (p=0.008), but no significant difference was observed for other types of mouthwashes(p> 0.05).
Extra precautions regarding the dental unit and sterilization of hand instruments were reported by 32.4% and 29.8% of the participants, respectively. Around 92.8% of the participants took precautions toward patients and their relatives/companions in the waiting room and 92.2% took precautions toward the dental staff to prevent contamination..
DiscussionDental procedures include the use of high-speed handpieces and air/water sprays and other processes that generate droplets and aerosols,19 dental clinics are among the highest risk environments in terms of cross contaminationDue to the microorganisms that survive in these particles, dental clinics are among the highest-risk environments for cross-contamination and COVID-19 infections.15,19 Therefore, all dental staff, especially dentists, face cross-infection risk caused by aerosols that can move deeper into the respiratory tract and even the the lungs during the COVID-19 pandemic.8,20 The presence of COVID-19 in the saliva of infected patients poses an additional risk after an aerosol-forming dental procedure.21 A recent report suggests that coronaviruses associated with severe acute respiratory syndrome can survive in aerosols for at least three hours, even if their infectious potential is reduced.22 It is necessary to establish and implement cross-infection control criteria according to evidence-based principles during the COVID-19 pandemic to minimize the microbial load of the aerosols produced.8,19
This research was aimed to evaluate the effect of the expertise/specialty degree [.1] of dentists and their work environment on their behavior, awareness, and attitudes toward cross-infection control during the COVID-19 pandemic. The results of this questionnaireare crucial for highlighting the transmission prevention strategies by professionals during the COVID-19 pandemic.
The demographic characteristics of the participants in this study are shown in Table 1. According to Table 2, most participants (81.9%) followed the current developments related to the COVID-19 pandemic and the guidelines and recommendations published by national/international authorities (74.2%). Also, 5.7% of participants reported had symptomatic COVID-19 infection. According to gender and qualification variables, there was no significant difference in responses to these two questions (p>0.005). According to a study conducted in Lombardy, Italy, 4.43% of the participants had suffered one or more symptoms related to COVID-19 and only 2% of dentists were confident in avoiding infection.23
Whereas the knowledge of the participants about droplet inhalation (98.2%), nasal mucosa (78.6%), eye mucosa (74.7%), and saliva/blood (54.2%) was acceptable, their knowledge of the fecal-oral route (26.7%) and contaminated sharp tools (20.3%) was insufficient to prevent COVID-19 infections( Table 2). The awareness of specialist dentists on this question was higher than of others (p=0.012). In a similar studies, the awareness of dentists about transmission routes was reported to be 71.82%.23 and 90% . 24
According to Peng et al.9, as a dental professionals play important roles in preventing the transmission of COVID-19, they should take extra infection control measures during dental practice to prevent person-to-person transmission in the clinics. During the COVID-19 pandemic, the first step of the infection control protocol recommended by ADA16 and CDC17 is to evaluate whether the patient is at an emergency situation or not. Elective and non-emergency procedures should be postponed, and dental treatments should be performed after considering the risk of COVID-19 transmission during the pandemic. According to Table 2, 59.9% of the respondents in this study performed both urgent and routine dental procedures. Since the pandemic has been presented in Turkey since March 2020, this may be the reason why many dentists return to routine dental procedures. As observed in Lombardy and Milan, the European regions where the pandemic caused most deaths, most dentists continued dental routine care by taking preventive measures.23 In this study, most participants (77.2%) followed strict cross-infection control methods during the COVID-19 pandemic, and specialists follow them more strictly (p=0.16). Participants from a similar study. 24
According to ADA16 and CDC,17 the second step is to determine PPE competence to perform dental procedures.16 The use of PPE against saliva or blood in dental procedures is considered the most crucial preventive strategy as the second step in the infection control protocol.16,17,25 Among the respondents, the use of disposable gloves (98.4%), surgical masks (91.1%), N95 masks (85.1%), disposable headsets (75.5%), face shields (91.5%), glasses/visors (51%), and protective suits (86.2%) were reported as effective methods to prevent COVID-19 infections(Table 2 ). It was found that the PPE use rate was statistically higher in females (p=0.025) and specialists (p=0.04), and there was a correlation between level of expertise and PPE use (r=0.121, p=0.01). The most commonly used PPE by Italian dentists were gloves (93.22%), surgical mask (74.56%), glasses/visor (91.28%), headsets (63.75%), and facial filters (58.84%).23 . The PPE use rate among endodontists from the United States was reported to be as follows: N95 mask (83.1%), face shield (58.9%), protective suit (36.8%), and headset (55.2%).26
Adopting professional precautions in dental practices that create microbial aerosols during the pandemic should be considered on a universally. . Standard precaution procedures should include more detailed and careful protection methods.19 According to Dawson et al.20 aerosols produced by operating the rotary instruments can reach all levels of the respiratory tract. Therefore, aerosol-forming procedures, including the use of handpieces, air/water spray and ultrasonic scalers, should be avoided, or PPE during the pandemic to prevent infections.16,20 According to a study that evaluated bacterial load in dental treatments, the amount of bacterial load in bioaerosols at a distance of 1.5 meter from the oral cavity of the patient was found to be higher than a 1 meter distance. Handpiece use significantly decreased contamination at all sampled distances from the oral cavity of the patient (average 970 CFU/m2/hour).18 According to the results obtained here , most of participants (90.6%) worried about aerosol generating dental procedures. Near 53.3% of participants suspended aerosol generating procedures,whereas 42.2%, 37.2%, and 24.8% of them stated they suspended oral scaling, aesthetic dental procedures and restorative procedures, respectively.
Other methods recommended to minimize droplet and aerosols spreading are to apply minimally invasive/atraumatic restorative techniques, a high-powered saliva ejector, and a rubber dam .17 The ubber-dam isolation can reduce airborne particles by up to 70% within a 3-feet diameter from the operational field.9,27 The current survey results revealed that 11.3% and 16.3% of the participants prefered rubber-dam and oral aerosol vacuum during the dental procedures, respectively. General dentists used the rubber dam at a higher rate than the other dentists (p=0.005). Although 80% of endodontists from the United States stated concerns about dental procedures, 82% reported that they performed treatments during the pandemic. Most of them were usedusedrubber-dam, and 16.9% added oral aerosol vacuum to their practice.26
Mouthwashes containing antimicrobials (i.e. chlorhexidine gluconate, essential oils, povidone-iodine or cetylpyridinium chloride) can be used to reduce COVID-19 viral load or to prevent contamination.17,25 According to the obtained results , hydrogen peroxide was the preferred mouthwash by 22.8% of dentists, and most of especialits (38.7%) preferred hydrogen peroxide mouthwash (p=0.008). Koletsi et al.19 reported that using 0.2% tempered chlorhexidine (CHX) before routine ultrasonic scaling resulted in a significant reduction in aerosol-associated bacterial load. Peng et al.9 suggested that CHX may not effectively kill COVID-19 virus , because it is vulnerable to oxidation to use an oxidative mouthwash (H202) before the procedure.
During the pandemic, attention should be paid to the maintenance of dental units and clinical equipment. One should be aware of potential risks of contaminated water intake and colonization by pathogenic microbial species.28 Due to the pandemic, using water filters in dental units, 3-6% hydrogen peroxide disinfection, CHX or specially designed biofilm removal systems is recommended.29 Attention should also be paid to the standard maintenance of the dental unit and unit water system. The water quality of the clinic must follow the safe drinking water standard (<500 CFU/mL).30 Extra-precaution regarding dental unit and sterilization of hand instruments was reported by 32.4% and 29.8% of the participants. However, routine cleaning and maintenance of autoclaves, air compressors, suction systems and aspirators, radiography equipment, amalgam mixers and other dental equipment should be meticulously done according to the manufacturer's instructions to decrease cross-infection risks . It is also recommended to use suction systems and aspirators with high suction power and antiseptic agents applied to the water system of the dental units.28,30 Additionally,COVID-19 has been shown to remain active at room temperature from two hours to nine days and more infectious in 50% relative humidity than 30%. Therefore, maintaining a clean and dry environment in the clinic will help reduce COVID-19 persistence .9
Providing cross infection control training to dental staff, maintaining only the required sterile equipment for the dental procedure, maintaining all other materials away from possible contamination in a closed cabinet, and carefully sterilizing contaminated equipment after the procedure are other essential strategies to prevent COVID-19 infections.17 When participants were asked about the precautions they had taken regarding dental staff and administrative order, PPE use (92.2%), social distancing measures (69.5%) and providing special courses (64.7%) were reported. According to Table 2, the suggested precautionsby the participants to prevent COVID-19 transmission in the waiting rooms include contacting patients by phone before the appointment and questioning about their COVID-19 symptoms (43.3%), using face masks (92.8%), applying social distance (minimum distances of 6-feet) measures (90.1%), using 60% alcohol-based hand sanitizer (85.6%), removing objects frequently touched by clients, removing foods and beverages, and limiting the number of relatives/companions of patients (66.3%).
The limitations of our study can be listed as a middle-sized sample, data collection limited to a short time period, and low level of e-mail responders due to the pandemic. New studies evaluating the theawareness and attitude of dentists towards the COVID-19 pandemic should be planned using larger samples with fewer variables.
ConclusionAlthough the knowledge of participants about the symptoms, transmission routes and adherence to the infection prevention guidelines were sufficient, dental specialists must follow infection control methods more strictly. Participants were concerned about dental procedures that create microbial aerosols during the pandemic period, yet they continued to deliver dental care using high PPE levels and took extra clinical precautions to avoid cross infection infection by COVID-19. Higher adherence by healthcare professionals to high-level cross-infection methods during dental procedures that generate microbial aerosols will undoubtedly reduce pandemic spreading
Author ContributionsM.M., design, data analysis, and interpretation, drafted and critically revised the manuscript; E.E. contributed to conception, data acquisition, contributed to analysis and interpretation, critically revised the manuscript; All authors gave final approval and agree to be accountable for all aspects of the work.
FundingNo funding