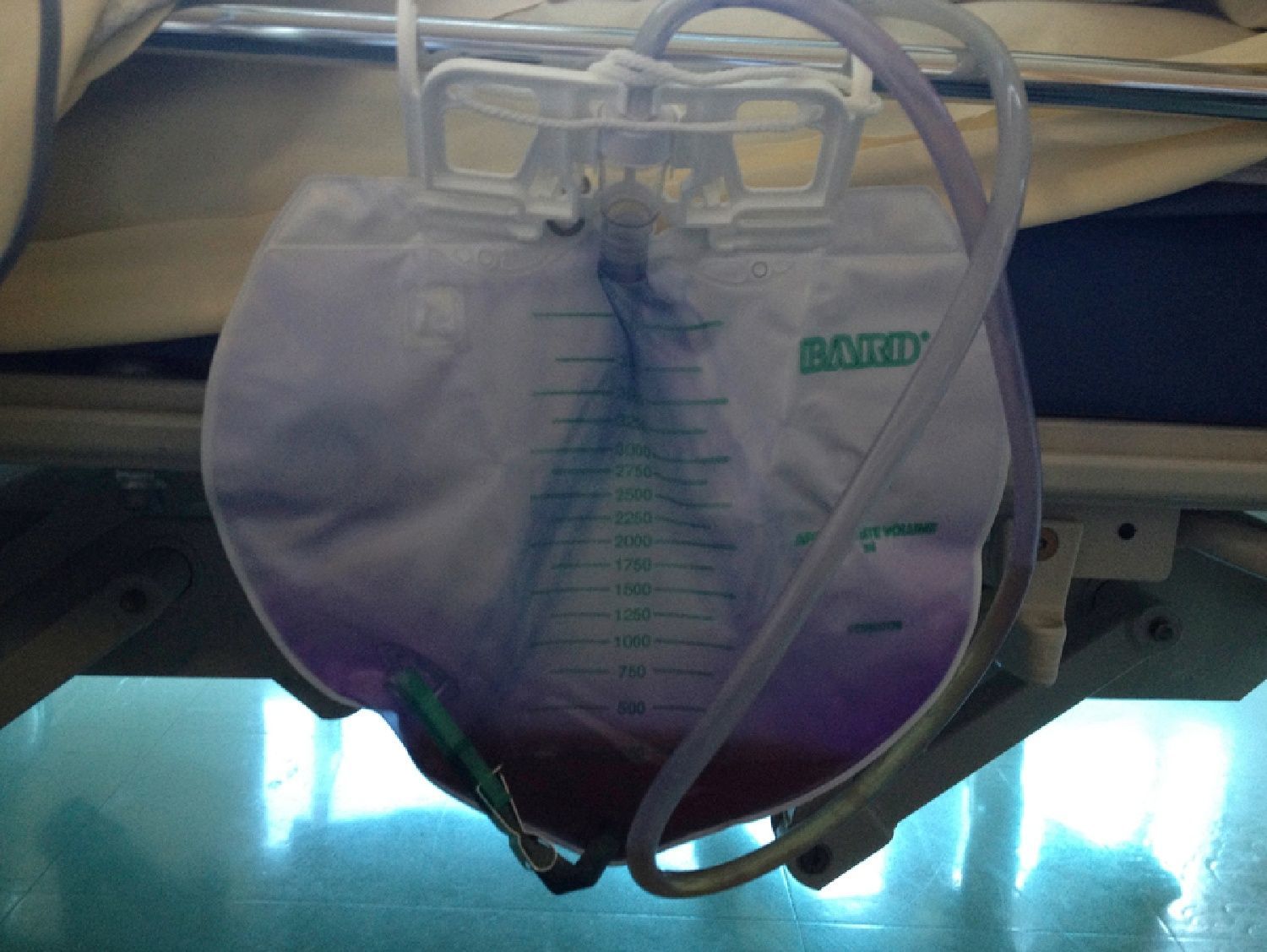
An 87-year-old woman was hospitalized for post-fall syndrome. Even though there was improvement in the post-fall syndrome, she had urinary retention, associated with fecaloma. Urinary catheterization showed acute urinary retention of 500mL. Urine microscopy and culture showed a resistant Escherichia coli strain. Given the absence of both clinical signs (apart from urinary retention) and inflammatory syndrome, no antibiotic therapy was initiated. Six days after inserting the indwelling catheter, purple coloration of the urine bag and the catheter appeared, with no modifications of urine color (Fig. 1). Another urine microscopy and culture performed long after catheter withdrawal, showed disappearance of the E. coli. Purple urine bag syndrome (PUBS) remained.
PUBS is a rare phenomenon first described in 1978.1 It can appear from a few hours to many days after catheterization.2 PUBS mainly occurs in elderly women,2 but cases in men and children have been described. Risk factors are urinary tract infection due to various pathogens, including E. coli; chronic constipation; use of laxatives; prolonged urinary catheterization; alkaline urine pH; tryptophan-rich foods; renal failure; and cognitive disorders.3,4 Being bedridden, which is associated with risk of constipation, seems to be a triggering factor for PUBS.2 After colonization by one or several bacteria, there are many biochemical reactions that start with tryptophan metabolism. Tryptophan is deaminated to form indole, which undergoes hepatic conjugation to form indoxyl sulphate. This is metabolized into indoxyl, indirubin, and indigo.2 These urinary components interact with the polyvinyl chloride of the catheter and urine bag to cause the purple coloration. Concerning the PUBS treatment, some authors recommend a short antibiotic therapy, whereas other authors recommend a simple change of urine bag and catheter.2–4 Although PUBS is rare, medical and paramedical teams must be aware that this phenomenon is not a serious complication of urinary tract disease.
Conflict of interestAll authors declare to have no conflict of interest.
The authors are grateful to Mr. Philip Bastable.